Healthcare Considerations for the Pregnant and Postpartum Patient
Normal Changes, Complications, and Implications for Care
Online Continuing Education Course

Course Description
Obstetric CEU course for all nurses and EMTs/paramedics. Covers patient management and common pregnancy complications such as bleeding and gestational diabetes. Care for pregnant women in all healthcare settings. Learn about risk factors, signs and symptoms, nursing care, maternal and fetal implications, and patient teaching.
"Terrific medical information for nurses!" - Kerri, RN in California
"The case studies were an excellent contribution to understanding the content." - Rose, RN in New Mexico
"Excellent course. Very organized, highlighting important concepts about each pregnancy complication. Thank you!" - Loretta, RN in California
"From start to finish, it took me two hours to complete, and I consider myself a fast reader and good comprehender of information. Knowing how that can differ greatly from person to person, I think these courses are all very on target as far as content and hours awarded. Thank you." - Amy, RN in Kansas
Healthcare Considerations for the Pregnant and Postpartum Patient
Normal Changes, Complications, and Implications for Care
Copyright © 2022 Wild Iris Medical Education, Inc. All Rights Reserved.
LEARNING OUTCOME AND OBJECTIVES: Upon completion of this continuing education course, you will be able to identify the normal changes, possible complications, and implications for care for the pregnant and postpartum patient. Specific learning objectives to address potential knowledge gaps include:
- Describe the ways in which pregnancy affects patient care.
- Differentiate normal from abnormal lab values in pregnancy.
- Identify signs and symptoms indicating possible pregnancy complications.
- Discuss the medical management and nursing care typically provided in response to the most common complications of pregnancy.
- Summarize relevant patient teaching offered to patients with gestational diabetes.
- Name the complications that can arise when amniotic membranes rupture prematurely.
- Discuss issues related to preterm labor and birth.
- List the most common postpartum complications.
TABLE OF CONTENTS
- How Pregnancy Affects Patient Care
- Normal Changes During Pregnancy
- Pregnancy-Related Bleeding Complications
- Hyperemesis Gravidarum
- Pregnancy-Related Hypertensive Complications
- Gestational Diabetes Mellitus (GDM)
- Amniotic Membrane Complications
- Preterm Labor and Birth
- Postpartum Complications
- Conclusion
- Resources
- References
HOW PREGNANCY AFFECTS PATIENT CARE
Nurses encounter pregnant and postpartum patients in a wide variety of settings, such as obstetric offices, emergency departments, urgent care clinics, primary care offices, mental health settings, and more. Thus, it is imperative for nurses to know when a patient’s pregnancy may have implications for procedures, diagnostics, medications, etc. It is also important for nurses to be able to distinguish normal from abnormal changes in pregnancy and to recognize signs and symptoms of pregnancy complications in order to provide appropriate care. With a patient who is pregnant, potential impacts on the health of the fetus must also be taken into consideration.
Pregnancy complications are occurring in increasing numbers, with more than 50,000 women in the United States affected annually by the most severe complications. Approximately 700 women die annually in the United States from pregnancy-related complications. Leading causes of death vary by timing relative to the end of pregnancy, and approximately 3 in 5 pregnancy-related deaths are thought to be preventable. Improving access to care and providing quality prenatal care—including managing chronic conditions and educating patients about warning signs—can help to prevent maternal death (CDC, 2019a).
RACIAL/ETHNIC DISPARITIES IN PREGNANCY-RELATED DEATHS
Significant racial/ethnic disparities exist in pregnancy-related mortality. Researchers found that Black and American Indian/Alaska Native women have a pregnancy-related mortality ratio approximately three times as high as that of White women, although preventability did not differ significantly by race/ethnicity or timing of death. Late postpartum deaths in Black women were attributable to increased cardiomyopathy (CDC, 2019b; Petersen et al., 2019). Sixty percent of pregnancy-related deaths are preventable.
According to the CDC (2019a), “every death reflects a web of missed opportunities.” They recommend the following path forward:
- Healthcare providers can:
- Help patients manage chronic conditions
- Communicate with patients about warning signs
- Use tools to flag warning signs early so women can receive timely treatment
- Hospitals and health systems can:
- Standardize coordination of care and response to emergencies
- Improve delivery of quality prenatal and postpartum care
- Train nonobstetric providers to consider recent pregnancy history
- States and communities can:
- Assess and coordinate delivery hospitals for risk-appropriate care
- Support review of the causes behind every maternal death
- Women and their families can:
- Know and communicate about symptoms of complications
- Note pregnancy history any time medical care is received in the year after delivery
Research has shown that there are “significant knowledge deficits in the care of patients presenting [to the emergency department] with high-risk conditions associated with pregnancy.” To address this issue, researchers recommend incorporating a specific list of obstetric complaints in the emergency department triage and acuity scale, including hypertension, headache, edema, abdominal pain, visual disturbances, and signs of stroke or pulmonary embolism (Wolf et al., 2021).
The use of medications must be reviewed for pregnancy risk. Information with regard to pregnancy, lactation, and females and males of reproductive potential are included as narratives in drug manuals. Examples of medications with potential adverse fetal effects include androgens, angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers, certain antiseizure medications, certain antidepressants, some antibiotics, retinoids, and warfarin (Lockwood & Magriples, 2022).
When the use of diagnostic imaging is indicated during pregnancy, its potential risks and the potential risks of not having the imaging must be considered. For instance, ionizing radiation received from X-rays and CT scans increases the risk for miscarriage, congenital anomalies, genetic disease, growth restriction, and developmental disorders. However, MRI and diagnostic ultrasound do not show any adverse maternal or fetal effects. Gadolinium, a contrast agent, should generally be avoided in pregnancy disorders (Kruskal, 2022).
In order to provide adequate care to pregnant and postpartum patients, it is necessary to be informed about high-risk situations in pregnancy. Learning the timing of issues that cause pregnancy-related deaths can help (see table below).
| Timing | Percentage | Causes |
|---|---|---|
| (Petersen et al., 2019) | ||
| During pregnancy | 31.3% | Other noncardiovascular medical conditions (e.g., endocrine, hematologic, immunologic, renal); other cardiovascular conditions (e.g., congenital heart disease, ischemic heart disease, cardiac valvular disease, hypertensive heart disease, congestive heart failure); infection |
| Day of delivery | 16.9% | Hemorrhage, amniotic fluid embolism, other cardiovascular conditions |
| Days 1–6 postpartum | 18.6% | Hemorrhage, hypertensive disorders of pregnancy, infection |
| Days 7–42 postpartum | 21.4% | Infection, other cardiovascular conditions, cerebrovascular accidents |
| Days 43–365 postpartum | 11.7% | Cardiomyopathy, other noncardiovascular medical conditions, other cardiovascular conditions |
Conditions prior to conception that can complicate a pregnancy include:
- Asthma
- Depression
- Diabetes
- Eating disorders
- Epilepsy and seizure disorders
- High blood pressure
- HIV
- Migraine
- Overweight and obesity
- Sexually transmitted infections
- Thyroid disease
- Uterine fibroids
The most prevalent complications that arise during pregnancy include:
- Anemia
- Depression
- Ectopic pregnancy
- Fetal problems
- Gestational diabetes
- High blood pressure
- Hyperemesis gravidarum
- Infections
- Miscarriage
- Placenta previa
- Placental abruption
- Preeclampsia
- Preterm labor
(Office on Women’s Health, 2021)
Nurses working with pregnant patients are in a unique position to identify, monitor, and provide care to patients who are affected by complications during pregnancy. It is essential for nurses to be familiar with these complications, as well as the maternal and fetal implications, medical treatment and management, and nursing care necessary to address these problems.
TERMINOLOGY
This course uses both the terms patient and woman when referring to those who are pregnant, while recognizing that not all people capable of pregnancy identify as female. For example, some individuals who are pregnant may identify as transgender men or gender nonbinary. In addition to needing standard care, these patients may require additional care and counseling.
NORMAL CHANGES DURING PREGNANCY
During pregnancy, the body undergoes normal physiologic changes in the cardiovascular, hematologic, renal, and gastrointestinal systems to accommodate and support the developing fetus. In the absence of illness, the body can generally compensate for these changes. However, in the presence of conditions such as anemia, clotting disorders, increased bleeding, preeclampsia, and trauma caused by motor vehicle accidents or intimate partner violence (IPV), the body may not be able to compensate for the changes.
When caring for pregnant patients, nurses must be aware of both the normal and abnormal physiologic changes that occur during pregnancy and the resulting laboratory values. This enables them to identify situations early and plan appropriate interventions.
Cardiovascular and Hematologic Changes
Maternal circulation changes during pregnancy to accommodate an increase in blood volume of up to 50%, including a 45% to 50% increase in plasma volume and 20% to 30% increase in red blood cells. Since these percentages are not equal, the subsequent hemoglobin/hematocrit will reflect a normal physiologic anemia of pregnancy.
During pregnancy, the systemic vascular resistance (SVR) of the blood vessels lowers due to increased levels of hormones. This decreasing SVR is an expected result of the increasing progesterone and prostaglandin levels, which relax smooth muscle, producing vasodilatation.
As a result of the increased volume and decreased resistance, cardiac output (and heart rate) rise. Therefore, there is a normal lowering of the blood pressure, especially in the second trimester. This sometimes causes dizziness or feeling faint in women as they rise to standing during the second trimester. Their pressure should stabilize and approach prepregnancy numbers by the third trimester.
White blood cell (WBC) counts, especially neutrophils, increase naturally during pregnancy. During active labor there may be another normal increase, even in the absence of infection. In nonpregnant patients, a normal WBC count is somewhere between 5 and 10 (5,000–10,000 cells/mm3), but for pregnancy, those normal values can be between 6 and 16 in the third trimester and may reach 20 to 30 in labor and early postpartum. When evaluating for infection, therefore, you need to look for other clinical indicators—such as increased temperature, bacteriuria, WBC in urine, uterine tenderness, and fetal tachycardia—and document them.
| Nonpregnant | Pregnant – 1st trimester | Pregnant – 2nd trimester | Pregnant – 3rd trimester | |
|---|---|---|---|---|
| (Cunningham, 2022) | ||||
| Hemoglobin (HGB) (g/dL) | 12–15.8 | 11.6–13.9 | 9.7–14.8 | 9.5–15 |
| Hematocrit (HCT) | 35.4%–44.4% | 31.0%–41.0% | 30.0%–39.0% | 28%–40% |
| Red blood cells (RBC) (x106/mm3) | 4.0–5.2 | 3.42–4.55 | 2.81–4.49 | 2.71–4.43 |
| White blood cells (WBC) (x106/mm3) | 3.5–9.1 | 5.7–13.6 | 5.6–14.8 | 5.9–16.9 |
Pregnancy is typically considered a hypercoagulable state—meaning that most pregnant women clot more readily than normal and are predisposed to deep-vein thrombosis or other clot-related conditions. During pregnancy there is an increase in certain factors in the clotting cascade due to normal adaptation. Platelets are usually unchanged in pregnancy, and increased levels of platelets are rare.
ABNORMAL CHANGES
- Diastolic murmur or very loud systolic murmur
- Rising blood pressure before the 20th week
- WBC levels above 20–30,000 cells/mm3, or shifts in the differential, especially a larger percentage of bands/stabs appearing, or a sharp increase in WBC level
- A true anemia (HGB <11.5 g/dL and HCT <30%)
Renal Changes
The renal system undergoes many changes in pregnancy to accommodate increased metabolic and circulatory requirements. The system clears the body of both maternal and fetal waste and is affected by the increased blood volume and lowered systemic vascular resistance. As previously mentioned, progesterone has a relaxing effect on vascular tissue, thus enhancing the renal blood flow and function. The increased plasma flow into the renal system causes the glomerular filtration rate (GFR) to rise dramatically.
Renal clearance of many substances is generally elevated in pregnancy, causing lower-than-usual serum levels of the renal markers blood-urea-nitrogen (BUN) and creatinine. Increased filtration does not mean enhanced reabsorption, however. The increase in glucose load during pregnancy is often spilled into the urine and not reabsorbed. Therefore, spillage of some glucose in pregnancy is not always indicative of pathology.
The anatomy of the pregnant uterus causes changes in the location and pressure of other internal organs. The bladder becomes slightly concave and is displaced forward and upward. The uterus causes the ureters to become dilated and more tortuous, especially the right ureter. Detectable hydronephrosis or hydroureter (i.e., dilation of the renal pelvis and ureter caused by obstruction to free flow of urine) during pregnancy is considered normal and may take 3–4 months post delivery to fully resolve.
| Nonpregnant | Pregnant | |
|---|---|---|
| (Cunningham, 2022) | ||
| Serum creatinine | 0.5–0.9 mg/dL | 0.53–0.9 mg/dL decrease |
| Serum BUN | 7–20 mg/dL | 8–10 mg/dL decrease |
| Serum uric acid | 2.5–5.6 mg/dL | 2–6.3 mg/dL |
| Urine creatinine clearance | 91–130 mL/min | 69–166 mL/min |
| Urine uric acid | 150–990 mg/24 hrs | Increases |
| Urine glucose | 60–115 mg/dL | Increases |
ABNORMAL CHANGES
- 24-hour urinary protein >300 mg
- Serum creatinine rising (indicates renal damage, possibly from preeclampsia)
- WBC >5 from urine sample (high-powered microscopic field)
- Bacteria >20 in urine sample (centrifuged urinalysis) (indicates UTI)
Gastrointestinal Changes
Increased progesterone levels also affect the gastrointestinal (GI) system of the pregnant woman. General tone, lower esophageal sphincter tone, and motility are decreased. This predisposes the woman to increased incidence of reflux (heartburn) and constipation. As the gravid uterus displaces the internal organs, this incidence increases.
The liver increases its production of lipids and cholesterol. This change, combined with delayed gallbladder contraction (due to progesterone-influenced relaxation), may lead to increased gallstone formation (expected) or inflammation of the gallbladder (abnormal). The liver also plays a role in the production of the clotting factors.
In addition to increased production of lipids and certain clotting factors, some enzymes found within the liver are also increased without indicating pathology. It is important to distinguish a normal rise in these levels from a pathologic change caused by organ damage or destruction arising, for example, from preeclampsia or hepatitis. In preeclampsia, microclots in the liver and capsular edema are danger signs, and if clotting factors become affected, the patient is at a high risk for disseminated intravascular coagulation (DIC). Diagnoses are not based upon a single abnormal value.
| Liver Enzymes | Nonpregnant | Pregnant |
|---|---|---|
| (Cunningham, 2022) | ||
| Alanine transaminase (ALT) | 4–71 units/L | Unchanged |
| Aspartate aminotransferase (AST) | 12–38 units/L | Unchanged |
| Alkaline phosphatase (ALP) | 33–96 units/L | > up to 2–4 times |
| Lactate dehydrogenase (LDH) | 115–221 units/L | Upper end of normal to 524 units/L |
Abnormal hepatic lab values can indicate such conditions as cholelithiasis, preeclampsia, hepatitis, cholestasis, and HELLP syndrome.
COVID-19 AND PREGNANCY
While pregnancy does not increase the risk of SARS-CoV-2 infection, it does increase the risk for severe disease. Pregnant women with COVID-19 experiencing severe or critical disease, particularly in the third trimester, appear to be at increased risk for preterm birth, cesarean birth, and stillbirth. They do not appear to be at risk for miscarriage or congenital anomalies. Asymptomatic patients in any trimester are at increased risk for developing preeclampsia (Berghella & Hughes, 2022).
PREGNANCY-RELATED BLEEDING COMPLICATIONS
Vaginal bleeding during pregnancy must always be investigated, particularly if it is enough blood to drop into the toilet or to warrant use of a menstrual pad. Bleeding can indicate pregnancy loss, placenta previa, placental abruption, ectopic pregnancy, or gestational trophoblastic disease. Events that may result in a small amount of bleeding (perhaps seen on toilet paper after voiding) due to cervical irritation include recent vaginal intercourse or recent cervical exam.
Pregnancy Loss
Pregnancy loss (also referred to as spontaneous abortion or miscarriage) is defined as a nonviable intrauterine pregnancy less than 20 weeks’ gestation (Prager et al., 2022b). This loss occurs without intervention from the patient or another person.
Pregnancy loss affects 10%–31% of pregnancies (Prager et al., 2022a). Risk for pregnancy loss increases with increasing maternal age and prior pregnancy loss. Pregnancy loss can be caused by a number of other factors, including chromosomal abnormalities, maternal infection, maternal endocrine disorders (e.g., hypothyroidism, uncontrolled diabetes), reproductive system abnormalities (e.g., cervical insufficiency), substance use, environmental factors (exposure to toxins and pollutants), and maternal injury.
NURSING CARE
The primary nursing intervention for all types of pregnancy loss is to ensure patient safety by identifying and controlling any bleeding and hemorrhagic shock. Symptoms of hemorrhagic shock include an increased heart rate, decreased blood pressure, cool and clammy skin, lightheadedness, and confusion. The nurse should anticipate the need for oxygen therapy and fluid and blood replacement. Patients should be blood-typed and cross-matched in case blood transfusion is necessary.
Pregnancy loss may be managed expectantly, with medication, or with surgery. Medication administration may include misoprostol (Cytotec) with or without the use of a prior dose of methotrexate. Misoprostol may be used to help in expelling the pregnancy tissue or to control bleeding. A patient-centered approach is recommended. By encouraging patients to participate in decision making about their care, they are likely to feel more satisfied.
The nurse monitors the patient’s vital signs, oxygen saturation, intake and output, and laboratory results according to institutional policies. If a patient experiences a threatened abortion but the fetus does not die, the nurse may be responsible for monitoring fetal heart sounds and the overall well-being of the fetus depending on gestational age. The nurse should administer prescribed anti-D-immune globulin (human) (RhoGAM) to Rh-negative patients within 72 hours to prevent alloimmunization (an immune response to the fetus’s blood cells).
RhoGAM
RhoGAM should be given to Rh-negative patients at approximately 28 weeks’ gestation, within 72 hours of the birth of an Rh-positive baby, with the possibility of maternal fetal hemorrhage (such as trauma to the abdomen during pregnancy, after an ectopic pregnancy, bleeding during pregnancy, after a pregnancy loss or induced abortion, after attempt at cephalic version, and after invasive procedures [e.g., amniocentesis]).
COMPLICATIONS
Two serious complications of missed abortions are infection and disseminated intravascular coagulation (DIC). Infection can occur as a result of carrying an expired fetus and is a serious health threat to these patients. DIC produces clotting, bleeding, and ischemia that occur simultaneously. Symptoms include sudden shortness of breath, chest pain, and/or cyanosis. Bleeding from the nose, gums, and IV sites, as well as petechiae, also occur in the presence of DIC. Treatment is aimed at delivering the fetus and placenta, which will stop the overactivation of the clotting process. Patients are treated with oxygen therapy and are usually given blood products.
| Normal in Pregnancy | DIC | |
|---|---|---|
| * Made when clots are broken down (Cunningham, 2022) |
||
| Fibrinogen (factor I) | 244–696 mg/dL | ⇓ |
| Platelets | 146–429 x109/L | ⇓ |
| D-dimer* | 200–1600 ng/mL | ⇑ |
PATIENT TEACHING
Nurses are responsible for ensuring that patients are adequately prepared to care for themselves upon discharge from the hospital following treatment or monitoring for a pregnancy loss. It is important that patients understand the warning signs of further complications and the importance of reporting such signs to their healthcare practitioner.
Warning signs include fever, foul-smelling vaginal discharge, significant bright-red vaginal bleeding, and pelvic pain. In addition, patients are encouraged to maintain pelvic rest (nothing per vagina) for two weeks. Experiencing a pregnancy loss is challenging for women both physically and emotionally, and they need to rest for a few days after discharge. They may be prescribed iron supplements for blood loss and/or antibiotics to treat or prevent infection. Foods such as liver, green leafy vegetables, dried foods, and eggs provide needed iron. Additional fluid intake is recommended.
It is important that the nurse recognize and acknowledge the patient’s loss or threatened loss. The patient is educated that it is normal to go through a grieving process. The patient should also be provided with appropriate community referrals for counseling and/or support groups. A patient may be eager to become pregnant again after losing a fetus; however, she should be encouraged to allow her body to rest and recover before attempting another pregnancy and to discuss with her healthcare practitioner when the appropriate time to conceive would be.
CASE
Rihanna is 29 years old and pregnant for the fifth time. Her first pregnancy resulted in birth at 34 weeks’ gestation and produced her only living child. She subsequently had three pregnancy losses at 12 weeks, 14 weeks, and 18 weeks. Rihanna is currently at 12 weeks’ gestation and is at the clinic for her first prenatal checkup. She was seen crying quietly in the waiting room and later states, “My mother-in-law says that if I weren’t such a weak person, I would not keep losing my babies.”
Discussion
Rihanna has had three consecutive pregnancy losses, which indicates that she has a history of recurrent pregnancy losses. Her healthcare practitioner discusses possible causative factors, such as cervical insufficiency or genetic disorders. It is important that Rihanna understand that her behavior did not cause the numerous losses. The nurse caring for Rihanna supports and offers encouragement to her throughout the pregnancy.
(Case study courtesy of Sharon Walker, RN, MSN.)
Ectopic Pregnancy
Ectopic pregnancies occur when the ovum is fertilized by the sperm but implants at a site other than the endometrium of the uterus. Ninety-six percent of ectopic pregnancies occur in the fallopian tubes (Tulandi, 2022a). Other possible implantation sites include the cervix, ovary, or abdominal cavity.
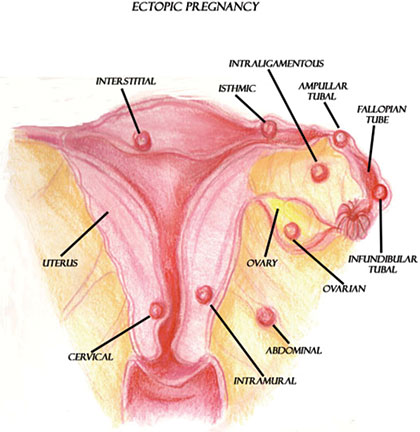
Possible implantation sites for ectopic pregnancies.
(Illustration courtesy of Sim London Jr.)
Ectopic pregnancies are caused by a variety of factors, which include anything that would prevent or slow the fertilized ovum’s journey to the lining of the uterus. More specifically, anything that causes scarring in or blocks the fallopian tubes may cause an ectopic pregnancy.
Patients who are of advanced maternal age or have reproductive system anomalies, a history of tubal surgery, pelvic genital infections, in utero diethylstilbestrol (DES) exposure, intrauterine devices (IUDs), cigarette smoking, in vitro fertilization, or use fertility drugs are at higher risk for having an ectopic pregnancy. The literature also suggests that women who douche regularly have a higher risk of an ectopic pregnancy (Tulandi, 2022b).
SIGNS AND SYMPTOMS
Signs and symptoms of an ectopic pregnancy include vaginal bleeding, lack of menstruation (amenorrhea), and abdominal pain. However, other disease processes (e.g., pregnancy loss) may be responsible for such symptoms. Transvaginal ultrasound and human chorionic gonadotropin (hCG) laboratory testing are necessary to diagnose an ectopic pregnancy.
The outcome of an ectopic pregnancy depends on the location of implantation. The ovum may naturally reabsorb into the body, or the structure supporting the ovum may rupture. If the implantation site is a fallopian tube, the tube may rupture and cause internal hemorrhaging and hypovolemic shock, which is a life-threatening event for the patient.
Signs and symptoms of a ruptured fallopian tube include vaginal bleeding; severe abdominal pain or pelvic, shoulder, or neck pain (as a result of blood leaking out of the fallopian tube and irritating the diaphragm); weakness; dizziness; decreased blood pressure; and increased pulse. It is important to note that many patients experiencing an ectopic pregnancy are asymptomatic prior to tubal rupture.
MEDICAL MANAGEMENT
An ectopic pregnancy implanted in a fallopian tube requires either pharmacologic or surgical management. Pharmacologic management with methotrexate is indicated if the tube is unruptured, the ectopic pregnancy is less than 3–4 cm, there is no fetal cardiac activity, and the patient is stable hemodynamically. Methotrexate is an antimetabolite chemotherapeutic agent that stops cells from dividing and thus stops the gestation. Methotrexate treatment is usually performed on an outpatient basis. Renal and liver function tests should be confirmed before administering methotrexate due to possible toxicity issues (Tulandi, 2022a).
Surgical management includes salpingostomy and salpingectomy. Salpingostomy requires a small linear incision in the tube to remove the pregnancy tissue. This protects the tube for a future pregnancy. A salpingectomy involves the removal of the affected fallopian tube.
NURSING CARE
The nurse caring for a patient experiencing an ectopic pregnancy observes for changes in the patient’s blood pressure and pulse, which could indicate hypovolemic shock resulting from hemorrhage. Regular assessment of vaginal bleeding is also essential. Rh-negative patients require administration of prescribed RhoGAM to prevent alloimmunization. Finally, the nurse is responsible for monitoring and controlling pain levels.
If salpingostomy or salpingectomy is performed, the nurse monitors vital signs, oxygen saturation, intake and output, and laboratory results according to institutional policies. As with all patients experiencing a pregnancy loss, it is important for the nurse to recognize the loss and to provide resources to assist the patient in coping with the emotions that accompany the experience of an ectopic pregnancy.
PATIENT TEACHING
Nurses are responsible for ensuring that the patient is aware of signs and symptoms that require a call to the healthcare practitioner or a return visit to the emergency room following hospital discharge. More specifically, a patient who experiences pain, significant bleeding, or a fever and chills must notify her healthcare practitioner. The nurse should provide the patient with a clear understanding of the normal feelings of anger, sadness, or guilt that may arise following an ectopic pregnancy and that these feelings are part of the grieving process for someone experiencing the loss of a pregnancy.
If laparoscopic surgery was performed, the patient may experience upper abdominal or referred shoulder pain related to carbon dioxide gas inserted into the abdomen during surgery (insufflation). Nurses provide the patient with instructions to ambulate often and to change positions frequently to assist with movement and absorption of this gas.
If methotrexate is used for the treatment of an ectopic pregnancy, the nurse educates the patient about its unpleasant side effects (nausea and vomiting) and informs the patient to avoid vitamins containing folic acid, which can decrease the effectiveness of the medication. The patient should also avoid vaginal intercourse until hCG is undetectable, avoid sun exposure to limit methotrexate dermatitis, and avoid nonsteroidal anti-inflammatory drugs (NSAIDs) (Tulandi, 2022c).
CASE
Cora is a 42-year-old newlywed. She comes into the Women’s Health Clinic complaining of vaginal bleeding and abdominal pain that is completely unlike her usual monthly cramping. She describes her pain as “very sharp” and an “11” on a scale of 0 to 10. Her vital signs are: temperature 98.8 °F, pulse 102 beats/min, respirations 24/min, and blood pressure 102/64 mmHg. She indicates that her blood pressure is “usually 130/90 mmHg.” She is unable to recall the date of her last menstrual period. Additionally, she has almost soaked an entire pad in the last hour.
Cora is very anxious and says, “I’ve never had any real female problems before, except for the little cramping I get on the first day of my period. I shouldn’t be having this difficulty because I keep my female parts very clean by douching weekly.” She sheepishly admits to having had gonorrhea five years ago.
Discussion
Cora is immediately assessed for an ectopic pregnancy. Her risk factors include: advanced maternal age, regular douching, and history of a sexually transmitted infection. She is bleeding heavily and showing evidence of hypovolemia. The priority in this situation is to ensure patient safety by obtaining and sustaining hemodynamic stability. Nursing interventions for Cora include monitoring her vital signs, amount of vaginal bleeding, intake and output, and laboratory results. Cora’s nurses are also involved with administering and teaching about prescribed medications (e.g., RhoGAM, methotrexate) and monitoring for potential side effects.
(Case study courtesy of Sharon Walker, RN, MSN.)
GESTATIONAL TROPHOBLASTIC DISEASE (GTD)
Gestational trophoblastic disease, most commonly the hydatidiform mole or molar pregnancy, occurs when the chorionic villi of the placenta increase as a result of genetic abnormalities. The villi swell, forming fluid-filled sacs, which have the appearance of tiny clusters of grapes within the uterus.
Patients with a GTD exhibit light to heavy bleeding and even hemorrhage. Bleeding can be bright red or watery and brown, appearing similar to prune juice. Anemia may result due to bleeding. Additionally, as a result of the proliferation of tissues and the presence of clotted blood, the uterus may appear larger than expected for gestational age. Despite an enlarged uterus, fetal heart tones and movement are absent. Serum hCG levels are also increased, and patients may experience hyperemesis.
Molar tissues are removed by surgical uterine evacuation. Intravenous oxytocin is usually administered to contract the uterus during suction evacuation to increase uterine tone and decrease blood loss.
Patients are followed for one year after removal of a molar pregnancy to detect choriocarcinoma, or cancer associated with GTD. If serum hCG levels do not return to prepregnancy levels, there is a possibility that choriocarcinoma may be present, and further investigation is necessary. Therefore, it is essential that patients understand the need for follow-up.
Placenta Previa
Placenta previa is the complete or partial covering of the internal os of the cervix by the placenta (see illustration). Placenta previa occurs when the placenta implants in the lower portion of the uterus near the internal cervical os. Previas are classified according to the degree to which they cover the os. Specifically, if the lower border of the placenta is less than 2 cm to the internal cervical os but not covering the os, the placenta is considered low-lying.
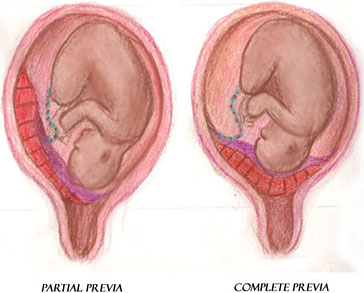
Placenta previa with partial covering of the internal os (left) and placenta previa with complete covering of the internal os (right).
(Illustration courtesy of Sim London Jr.)
As the pregnancy nears term and the cervix dilates, the placenta implanted near or over the internal cervical os is disrupted and bleeding can occur. The bleeding places the patient and fetus at risk. The major factors that place patients at risk for a placenta previa include previous placenta previa, previous cesarean delivery (risk increases with an increasing number of cesarean deliveries), and multiple gestation (Lockwood & Russo-Stieglitz, 2022a).
SIGNS AND SYMPTOMS
The most significantly recognized symptom of placenta previa is painless, bright-red vaginal bleeding or hemorrhage during late pregnancy. However, bleeding may not occur until labor begins. If there is a diagnosis or high suspicion of placenta previa, it is imperative that vaginal examinations be avoided, because stimulation of the placenta may cause hemorrhage. The bleeding as a result of placenta previa could cause the patient to hemorrhage and go into shock, and the fetus could experience hypoxia and possibly death from maternal bleeding.
As a result of the abnormally implanted placenta, the fetus is often in a transverse or breech position, which may be noted during fundal examination.
MEDICAL MANAGEMENT
As previously mentioned, vaginal examination must be avoided if a patient presents with painless, bright-red vaginal bleeding because hemorrhage may occur. A transabdominal ultrasound can be performed to diagnose the previa. It may be followed by a transvaginal ultrasound in order to better visualize the cervix and placenta. Medical management of a placenta previa is largely determined by gestational age, fetal status, amount of bleeding, and type of previa.
Some patients may deliver vaginally if they are near term, the cervix is ripe, the previa is not total, the fetal heart tracing does not show fetal compromise, and there is minimal bleeding. However, if heart tracings indicate fetal compromise, significant bleeding, or hemorrhage, or a complete previa is present, a cesarean section is usually necessary.
NURSING CARE
Nursing care for patients hospitalized with a placenta previa involves close monitoring of bleeding as well as fetal and maternal status. Significant bleeding or hemorrhage should be quantified and reported immediately to the appropriate healthcare provider. Careful monitoring of bleeding is imperative, as vital sign changes may not be initially evident. Regular assessment of fetal heart rate (FHR) and movement is necessary. Heart rate patterns that indicate fetal compromise (i.e., recurrent late or prolonged decelerations, absent or marked FHR variability) should be reported to the healthcare practitioner immediately.
Nonstress testing to evaluate fetal status is performed during bleeding episodes according to medical orders or institutional policy. Patients should be blood-typed and cross-matched in case a blood transfusion is necessary. Blood loss should be quantified. Intravenous access should be maintained for prompt administration of fluids or blood products.
Anti-D-immune globulin (RhoGAM) is given to Rh-negative patients during each bleeding episode to prevent alloimmunization. If bleeding episodes are within three weeks of administration, readministration is not necessary (Lockwood & Russo-Stieglitz, 2022b).
PATIENT TEACHING
Patients with a placenta previa and a history of bleeding should avoid moderate and strenuous exercise, heavy lifting, and standing for prolonged periods, and are encouraged to prohibit vaginal examinations. Patients are advised to avoid any sexual activity that may lead to orgasm, since the uterine contractions that result could provoke bleeding. They are also advised to call their provider promptly if bleeding or labor occurs. If asymptomatic, cesarean section should be scheduled at 36 to 37 weeks (Lockwood & Russo-Stieglitz, 2022b).
Placental Abruption
Placental abruption, often referred to as an abruption or abruptio placentae, is the premature separation of the normally implanted placenta from the uterine wall before delivery of the fetus. It is considered an obstetrical emergency. Bleeding occurs between the uterine wall and the placenta.
Placental abruption is a potentially life-threatening event for the patient and the fetus, depending on the severity of the abruption. Patients with an abruption are at risk for developing hypovolemic shock, disseminated intravascular coagulation (DIC), and possibly death. Since the placenta is the source of oxygenation for the fetus, premature separation of the placenta from the uterine wall can place the fetus at great risk for hypoxia and death.
Placental abruption is classified according to the degree of placental separation and subsequent hemorrhage. An abruption can be partial or complete, with apparent or concealed hemorrhage (see illustrations). An abruption is partial if a section of the placenta separates from the uterine wall but a portion of the placenta remains attached. A complete abruption, the most emergent form, occurs when the entire placenta detaches from the uterine wall. Apparent hemorrhage refers to bleeding that is evident, while a concealed hemorrhage denotes bleeding that is obscured.
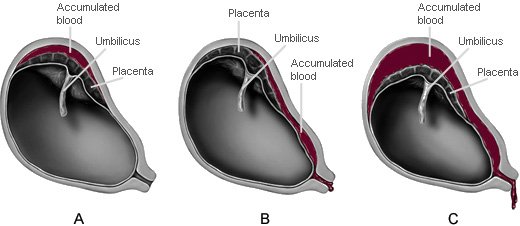
A. Partial placental abruption with concealed hemorrhage
B. Partial placental abruption with apparent hemorrhage
C. Complete placental abruption with apparent hemorrhage
(Illustrations by Jason McAlexander. © Wild Iris Medical Education.)
Aside from abruptions occurring as a result of trauma, the cause of placental abruption is largely unknown. However, there are several factors that place patients at risk for an abruption, including the strongest risk factors of previous abruption, cocaine or other drug abuse, and eclampsia (Ananth & Kinzler, 2022).
SIGNS AND SYMPTOMS
The classic signs and symptoms of placental abruption include an abrupt onset of vaginal bleeding, which may be dark red due to old blood from a concealed abruption; uterine tenderness; and a board-like abdomen. Patients often complain of an aching or dull pain in the abdomen or lower back. Additionally, frequent uterine contractions with poor uterine resting tone (the baseline pressure of the uterus between contractions) are frequently noted.
MEDICAL TREATMENT
Placental abruption is usually diagnosed by abdominal ultrasound in addition to the presenting signs and symptoms. Treatment is based on the degree of placental separation and subsequent hemorrhage as well as the status of the patient and fetus. In the presence of severe abruption and hemorrhage, emergency cesarean section is performed unless delivery is imminent.
NURSING CARE
Although vaginal delivery is preferred to cesarean section for patients who are hemodynamically stable, the nurse must be prepared to deal with the possibility of severe hemorrhage and hypovolemic shock, as well as the resulting fetal distress. Intravenous access with a large-bore catheter is placed to accommodate the administration of fluid and blood products.
It is necessary to monitor carefully the status of the patient and fetus. Frequent vital signs and fetal heart tones, as well as monitoring and documentation of blood loss, is essential. Maternal bleeding may be indicated by falling hemoglobin and hematocrit or abnormal CBC (complete blood count). Abnormal vital signs, bleeding, or fetal heart patterns indicating fetal compromise should be reported immediately to the appropriate healthcare provider. Observation and documentation of the patient’s intake and output and pain and comfort levels are also essential. Patients should be blood-typed and cross-matched in case a blood transfusion is necessary. RhoGAM is indicated for Rh-negative patients. Fetal distress may be indicated by electronic fetal monitoring changes, such as tachycardia followed by bradycardia, absent variability, decelerations, and/or sinusoidal tracing.
Because the potential for patient and fetal injury is high in the presence of placental abruption, it is important to address the emotional needs of the patient. Patients should be kept informed of the status of the fetus, and the nurse should be available and ready to answer any questions that patients or their families may have.
PATIENT TEACHING
Patients are instructed to report bleeding and severe abdominal pain immediately. It is important to inform patients with placental abruption that emergency delivery may be necessary. If a patient must have an emergency cesarean section, the nurse must quickly communicate to the patient and family what will occur before and during the procedure. Nurses should remember that hemorrhage and emergency surgery can be very frightening; therefore, clear and honest information must be given to the patient and family as frequently as possible.
| Assessment | Placenta Previa | Placental Abruption |
|---|---|---|
| Pain | Painless | Uterine tenderness; severe abdominal pain and possibly aching or dull pain in the lower back |
| Bleeding | Bright red | May be concealed; if noted, it is often dark red |
| Uterus | No unusual contractions or irritability | “Board-like” abdomen; uterine irritability with poor resting tone |
| Risk for postpartum hemorrhage | High risk; due to low placement of the placenta, there is limited uterine contraction | High risk due to poor contractility of the uterus following an abruption |
CASE
Rebecca has her first prenatal visit at 30 weeks’ gestation. She is extremely quiet, holds her head down, and stays very close to her husband, speaking in whispers only to him. Rebecca’s husband then repeats her comments and questions to the nurse and clinic staff. Her uterine height and the fetal heart tones are all within normal limits. However, the nurse observes multiple bruises in various stages of healing on the patient’s torso and legs and a moderate amount of dark vaginal blood on her peri-pad. Although Rebecca (through her husband) denies any pain, she is sweating profusely and seems to have abdominal pain.
Discussion
The presence of bruises at various stages of healing and Rebecca’s dependence on her partner to answer for her are possible indications of intimate partner violence. There is also a possibility of placental abruption related to abdominal trauma. The patient has dark red vaginal bleeding and evidence of abdominal pain. It is important for the healthcare practitioner to speak with Rebecca in private to discern the cause of her bruising and possible abuse. In addition, the nurse must ensure the safety of the patient and the fetus.
(Case study courtesy of Sharon Walker, RN, MSN.)
HYPEREMESIS GRAVIDARUM
Nausea and/or vomiting occur normally during pregnancy and can affect up to 90% of pregnancies. Symptoms often start at 5–6 weeks’ gestation and usually subside by 20 weeks. Dietary changes can help alleviate the symptoms. These include eating before or as soon as feeling hungry; additional snacks; small, frequent meals; avoiding triggers; and consuming ginger. Nausea and vomiting that develop after 10 weeks’ gestation may also be caused by conditions unrelated to pregnancy (e.g., gastrointestinal disorders) and should be investigated (Smith et al., 2022a, 2022b).
Nausea and vomiting that occurs regularly beyond 20 weeks’ gestation and involve hypovolemia and weight loss >5% of prepregnancy body weight during pregnancy is termed hyperemesis gravidarum, or severe, persistent nausea and vomiting. The cause of hyperemesis is unknown, however elevated hormonal levels and relaxation of smooth muscle resulting in delayed stomach emptying, along with stress, are believed to play a part in this disorder.
Patients with hyperemesis gravidarum frequently become dehydrated and may have metabolic acidosis as a result of starvation. In addition, patients may become alkalotic from a loss of hydrochloric acid during vomiting. Electrolyte imbalances such as hypokalemia and vitamin deficiencies are also common in patients with hyperemesis gravidarum. Ultimately, long-term nausea and vomiting can cause renal and/or gastrointestinal impairment in the pregnant patient.
Dehydration occurring from hyperemesis gravidarum may also result in preterm labor, which can negatively impact the fetus. In addition, dehydration impairs placental perfusion and affects nutrient intake and oxygenation of the fetus. Moreover, due to the severe nausea and vomiting associated with hyperemesis, poor maternal nutrient intake is common and fetal growth may be compromised, causing low-birth-weight infants.
Signs and Symptoms
Normal first-trimester nausea and vomiting can be challenging for pregnant women. However, patients with hyperemesis gravidarum are frequently debilitated by unrelenting vomiting and dry retching. Common signs and symptoms of hyperemesis gravidarum include:
- Poor appetite
- Poor nutritional intake
- Vomiting beyond 20 weeks’ gestation
- Significant weight loss (>5% of prepregnancy weight)
- Ketonuria unrelated to other causes
- Dehydration (dry mouth and mucous membranes, decreased skin elasticity [turgor], and dark, concentrated urine)
Medical Treatment
When diagnosing hyperemesis gravidarum, it is important to investigate the underlying causes of nausea and vomiting. These causes can include gastroenteritis, pancreatitis, hepatitis, peptic ulcer disease, and pyelonephritis. Patients usually require intravenous fluids and antiemetics to manage hyperemesis. While most care for hyperemesis is provided in the patient’s home, some patients may require hospitalization for nutritional support via enteral or parenteral access.
Nursing Care
Nurse caring for patients with hyperemesis gravidarum includes monitoring and providing physical care as well as psychosocial support. The nurse will administer IV fluids and antiemetics. Intake and output are carefully monitored, as well as gastrointestinal status. Laboratory results (e.g., ketones, electrolytes, complete blood count, liver enzymes) are carefully monitored, with abnormal results reported to the appropriate healthcare practitioner. It is also important to monitor for weight loss since the constant, prolonged nausea and vomiting associated with hyperemesis may easily result in malnutrition for pregnant patients.
Often patients are unable to work or tend to activities of daily living. This underscores the need for the nurse to address the psychosocial needs of patients, which may involve simply listening to the patient or a referral to appropriate resources.
Patient Teaching
Most of the nursing care provided to patients with hyperemesis gravidarum involves teaching the patient strategies to manage the associated nausea and vomiting. It is important for patients to understand the need to eat small, frequent low-fat meals throughout the day. Usually, toast, dry cereal, and other bland foods (e.g., bananas, rice, and apples) are well tolerated. Consistent protein intake is also helpful in preventing nausea (Smith et al., 2022b). Patients are instructed to identify and avoid foods and odors that trigger nausea and vomiting.
In addition, patients should be encouraged to maintain adequate fluid intake to prevent dehydration. Since constant, prolonged vomiting affects the patient’s mouth and desire to eat, nurses also teach and encourage patients to provide and maintain adequate oral care. It is important to provide appropriate instructions regarding their medications to patients who are prescribed antiemetics.
Positive ketones in the urine indicate that patients are using fat stores to provide energy to themselves and their growing fetuses. For patients who are required to use urine dipsticks to monitor ketones while at home, the nurse provides instruction in their appropriate use.
Nurses instruct patients to notify their healthcare practitioner if they notice dark urine, bloody vomitus, abdominal pain, dehydration, lack of urine output for eight hours, positive ketones, or inability to keep food down for 24 hours.
CASE
Deanna is in the 10th week of her first pregnancy. She has come to the second prenatal visit stating she has many questions: “I thought you got bigger when you have a baby. I started out weighing 130 pounds, and on your scale I now weigh 121. Is it because of all the barfing?”
Deanna describes vomiting four to six times per day: in the morning as soon as she gets out of bed, sometimes after eating lunch, and after eating dinner. “If I’m not actually barfing, I can’t look at food because I feel like I will. My mom said its normal to have morning sickness, but it’s not called ‘all-day sickness,’ is it?”
Deanna’s urine is amber-colored. She has poor skin turgor, flaking skin over much of her body, and sticky mucous membranes. “My husband is really beginning to complain about my not cooking anything. But really, if I smell any food, everything I’ve eaten comes up. I spew like a volcano. My husband has taken to calling me Mt. Vesuvius.”
Discussion
Deanna should be assessed further for hyperemesis gravidarum. She has decreased turgor, dry skin, and sticky mucous membranes. Deanna reports constant nausea and frequent vomiting. Her weight loss is more than 5% of her prepregnancy weight, and her urine is concentrated. The nurse should work with Deanna on interventions for improving her intake and curtailing the symptoms of hyperemesis.
(Case study courtesy of Sharon Walker, RN, MSN.)
PREGNANCY-RELATED HYPERTENSIVE COMPLICATIONS
Gestational hypertension is defined as hypertension (systolic blood pressure ≥140 mmHg and/or diastolic blood pressure ≥90 mmHg) on at least two occasions at least four hours apart occurring for the first time at ≥20 weeks’ gestation. The diagnosis is characterized by a blood pressure that returns to normal by 12 weeks postpartum. Gestational hypertension is a provisional diagnosis; if the patient has proteinuria or new signs of end-organ dysfunction, then the diagnosis is instead preeclampsia. Gestational hypertension may also progress to preeclampsia (Melvin & Funai, 2022).
Preeclampsia is identified by the above gestational hypertension blood pressure parameters (or systolic blood pressure ≥160 mmHg or diastolic blood pressure ≥110 mmHg on one occasion) in the presence of protein in the urine (proteinuria) or end-organ dysfunction (characterized by low platelets, increased protein creatinine ratio, pulmonary edema, elevated liver function tests, visual changes, and headache) (August, 2022).
Eclampsia is the occurrence of generalized seizures in the presence of preeclampsia without other known cause for the seizures. Seizures can occur any time before, during, or after delivery of the fetus.
Chronic hypertension is defined by a systolic blood pressure ≥140 mmHg and/or diastolic pressure ≥90 mmHg on at least two occasions that is present prior to pregnancy, presents before the 20th week of pregnancy, or persists longer than 12 weeks postpartum.
Preeclampsia superimposed on chronic hypertension is diagnosed in a patient with chronic hypertension who develops worsening hypertension with new onset proteinuria or other features of preeclampsia (e.g., elevated liver enzymes, low platelet count) (August, 2022).
Pathophysiology
Vasospasm in the arterioles of patients with gestational hypertension causes increased blood pressure and a decrease in placenta and uterine perfusion. Renal blood flow is reduced, along with the renal glomerular filtration rate, which produces proteinuria. Headaches and visual disturbances are the result of cellular damage and cerebral edema caused by central nervous system changes in the presence of hypertension. Liver enlargement is the result of hepatic changes that lead to epigastric pain. Generalized vasospasm causes endothelial cell damage, which triggers coagulation pathways, and subsequently, abnormalities in bleeding and clotting can occur.
Maternal and Fetal Implications
Hypertension during pregnancy places patients and their fetuses at great risk for a variety of complications. Some of the most significant maternal complications of hypertension in pregnancy include cerebral vascular accident (CVA, or stroke), disseminated intravascular coagulation (DIC), and placental abruption from the elevated blood pressure.
Additionally, patients are at risk for the development of HELLP syndrome, likely a severe form of preeclampsia. Just as its name implies, HELLP syndrome causes great dysfunction within the body and requires immediate intervention. It is characterized by:
- Hemolysis of red blood cells, which leads to anemia
- Elevated liver enzymes, leading to epigastric pain
- Low platelets, which cause abnormal bleeding and clotting as well as petechiae
Patients with HELLP syndrome whose function continues to decline without intervention can develop eclampsia and are at risk for DIC, placental abruption, acute renal failure, pulmonary edema, liver hematoma/rupture, and retinal detachment (Sibai, 2022). Fetal complications derive from placental abruptions, intrauterine growth restriction, and preterm birth resulting from decreased placenta perfusion.
Medical Treatment
Medical treatment for patients with gestational hypertension greatly depends on the severity of hypertension and the gestational age of the fetus, as well as the potential risk to the patient and fetus.
During early pregnancy, outpatient management is usually appropriate; these patients are monitored at home for blood pressure, proteinuria, and other signs and symptoms of preeclampsia and may be prescribed oral antihypertensives. Regular fetal monitoring is necessary to evaluate fetal well-being.
Severe hypertension requires immediate intervention with intravenous medications such labetalol and/or hydralazine. Glucocorticoids may be administered to enhance fetal lung maturity. Low-dose aspirin started prior to 20 weeks’ gestation for patients with average or high risk of developing preeclampsia may be given to decrease the likelihood of developing preeclampsia or its subsequent placental and fetal effects (Melvin & Funai, 2022).
Magnesium sulfate (MgSO4) may be prescribed during labor and delivery to prevent seizures and for fetal/neonatal neuroprotection in pregnancies between 24–32 weeks’ gestation. Magnesium sulfate is not used to control hypertension. Magnesium sulfate is administered intravenously via an infusion delivery device during delivery and for 24 hours post delivery. Since MgSO4 can cause respiratory depression in the neonate, arrangements are made for specialized neonatal care.
Nursing Care
Gestational hypertension presents a great risk to patients and their fetuses. Therefore, it is the responsibility of the nurse to monitor the patient carefully for signs of a decline in health status. The nurse should immediately report increases in blood pressure, visual disturbances, severe headaches, epigastric pain, and oliguria to the appropriate healthcare practitioner.
In the presence of eclampsia, the nurse must be prepared to prevent injury to the patient during seizures and to monitor seizure activity. Bedside rails should be up and padded. Emergency equipment should be readily available, including oxygen, a nonrebreather face mask, and emergency medication.
In the event of a seizure, patients should be protected from injury. The nurse should note the beginning and ending of the seizure and ensure adequate oxygenation after seizure activity has ceased. The nurse should not attempt to insert any object into the mouth during a seizure. The patient should be placed in a lateral position if possible, or the head gently turned to the side to prevent the aspiration of mucus and emesis into the lungs during seizure activity. The nurse may provide oxygen by nonrebreather mask. The nurse obtains vital signs and monitors the fetus following the seizure.
Labor may progress rapidly during seizure activity. Sometimes newborns are delivered suddenly during a seizure. The nurse should be prepared for an imminent delivery in patients with preeclampsia and eclampsia.
Patient Teaching
Patients suffering from gestational hypertension who are being treated on an outpatient basis are taught to monitor themselves and their fetus for a decline in health status. Specifically, patients are taught to notify their healthcare practitioner if they experience symptoms suggestive of preeclampsia (headache, visual changes, epigastric or right upper quadrant pain). They are also instructed to perform daily fetal kick counts to monitor fetal well-being.
CASE
Eden, a 16-year-old, comes to the urgent care clinic because she is certain she has a respiratory illness. She is pregnant for the first time, with twins, and is in her 37th week of gestation. When her name is called, she rushes in to the examination room, saying, “I’m so glad to see you. I have this nasty cough, and I also feel like my head is going to explode. My face has gotten fat like my belly. I can’t wait for this whole thing to be over.”
Eden’s vital signs are temperature 98.2 °F, pulse 70, respirations 20, and blood pressure 150/98. Her urine is 2+ for protein. Pitting edema of +2 is noted bilaterally in the lower extremities. The fetal heart rates are in the 150s for both fetuses. She has a productive cough and crackles in the bases of both lungs. Eden’s mother usually attends prenatal appointments and has talked in the past about the seizures she experienced when she was pregnant with Eden.
Discussion
In addition to a respiratory workup, Eden is assessed thoroughly for complications associated with gestational hypertension. She has some risk factors and exhibits several symptoms. Eden is very young, is pregnant with twins, and has a family history of eclampsia. She has proteinuria, facial edema, and edema of the lower extremities.
Eden may be hospitalized on bed rest for evaluation of her condition. Her vital signs will be closely monitored, with attention to fetal well-being; urinary output; and reports of headache, visual disturbances, and epigastric pain. The goals of hospitalization for Eden include prevention of seizure and promotion of a safe delivery. Since Eden is so close to her due date, an induced delivery may be considered.
(Case study courtesy of Sharon Walker, RN, MSN.)
GESTATIONAL DIABETES MELLITUS (GDM)
Gestational diabetes mellitus occurs when a patient’s pancreatic function is not sufficient to overcome the insulin resistance associated with pregnancy. In pregnancy, glucose demands increase as the fetus grows. The “insulin-antagonistic” properties of placental hormones affect the patient by causing normal insulin resistance of pregnancy. This allows a proper supply of glucose for the growing fetus. In gestational diabetes mellitus, the pregnant patient is unable to process glucose sufficiently in the body and hyperglycemia occurs (Durnwald, 2022a).
Individuals who have had GDM are also more than nine times as likely to develop type 2 diabetes (Durnwald, 2022b).
Maternal and Fetal Complications
A variety of maternal and fetal complications are associated with GDM.
Infants born to patients with gestational diabetes mellitus are significantly more likely to be macrosomic (birthweight >4.5 kg). This occurs due to fetal hyperinsulinemia as a result of maternal hyperglycemia, which stimulates excessive growth. These large infants may have difficulty maneuvering the birth canal, and a cesarean section may be required. If vaginal delivery is attempted, the infant is at risk for shoulder dystocia and related birth injuries. Patients also have an increased frequency of gestational hypertension, preeclampsia, polyhydramnios, and stillbirth.
After delivery, the newborn infant’s blood glucose must be monitored regularly for hypoglycemia due to the sharp decrease in available glucose after the umbilical cord is cut. The newborn’s pancreas continues to produce insulin after delivery despite the decrease in serum glucose. This adds to the potential instability of the infant’s blood glucose. Infants are also at risk for hypocalcemia, hyperbilirubinemia, hypomagnesemia, polycythemia, cardiomyopathy, and respiratory distress syndrome as a result of gestational diabetes (Durnwald, 2022a).
PREEXISTING DIABETES MELLITUS
In addition to the risks associated with GDM, women with pregestational diabetes mellitus (type 1 or type 2) are at risk for their children to have congenital anomalies related to hyperglycemia during early pregnancy. It is advised to keep diabetes under control for at least three months before trying to conceive.
Medical Treatment
Pregnant patients are routinely screened for GDM at 24–28 weeks’ gestation. In order to diagnose gestational diabetes, patients drink 50 grams of oral glucose solution. After one hour, a blood sample is obtained and tested for glucose tolerance. A glucose level of ≥130–140 mg/dL is considered a positive screen, and further investigation is warranted. A three-hour glucose tolerance test (with a 100 gram oral glucose solution) is then typically performed.
Most patients with GDM are treated through diet and exercise. Patients are advised to eat a diet favoring fruit, vegetables, whole grains, and fish and low in red and processed meat, refined grains, and high-fat dairy. Some patients may require insulin or oral hypoglycemia agents to manage gestational diabetes mellitus.
Nursing Care
It is important for the nurse to monitor serum glucose levels throughout the pregnancy of patients with GDM. A referral to a dietitian may also be necessary. The nurse may also conduct regular fetal surveillance, including nonstress tests or biophysical profiles starting at 32–36 weeks’ gestation and until delivery.
Patient Teaching
The nurse working with patients diagnosed with GDM is often responsible for teaching the patient to self-monitor and record glucose at home. In addition, the nurse may teach patients about proper diet and safe exercise during pregnancy.
During prenatal visits, the nurse reviews the blood glucose and diet logs to make recommendations about monitoring, medication administration, and diet. Patients may also need to learn how to self-administer insulin. The nurse ensures that the patient can comfortably and appropriately check blood glucose levels and administer insulin by requesting a return demonstration.
It is imperative that the nurse teach patients with gestational diabetes the signs and symptoms of hypoglycemia, which include shakiness, anxiety, headache, hunger, cold, clammy skin, and tingling around the mouth. The patient is taught to closely monitor for hypoglycemia and to notify the healthcare practitioner immediately if signs and symptoms are noted.
Hypoglycemia in those with GDM is treated by immediately eating 10–20 g of a fast-acting carbohydrate snack. Eight ounces of skim milk may be used, as it tends to dampen the rapid elevation of glucose followed by rapid decline that can result in pregnant women with diabetes from consuming a pure simple sugar (Durnwald, 2022b).
Since the potential for developing diabetes is significant in patients with gestational diabetes, it is important that patients understand the need for follow-up evaluation after delivery. Patients should continue to watch for signs and symptoms of hypo/hyperglycemia and notify their healthcare practitioner if seen.
OBESITY IN PREGNANCY
The prevalence of obesity in those of reproductive age is 40%. One quarter of pregnancy complications (e.g., gestational hypertension, preeclampsia, gestational diabetes, large-for-gestational-age newborns, and preterm birth) are attributable to maternal overweight/obesity (Ramsey & Schenken, 2022). Given the magnitude of this issue, it is imperative that patients be educated about the benefits of diet and exercise during preconception counseling and during the pregnancy.
CASE
Agnes is a 31-year-old patient who is pregnant for the fourth time. She has one living child, born at 36 weeks’ gestation and weighing 11 pounds. Agnes also had a stillborn baby born at 36 weeks and one pregnancy loss. At her routine 28-week prenatal visit, she arrives early to drink a 50-gram dose of glucose cola and have blood drawn for the oral glucose challenge test. The results of the test are abnormal.
Discussion
Agnes shows signs of gestational diabetes mellitus, both currently and in her previous pregnancies. A macrosomic infant, a stillborn, and a pregnancy loss are indicative of GDM. The nurse teaches Agnes how to monitor her blood glucose levels and self-administer insulin. The nurse also stresses to Agnes the importance of proper diet and blood glucose control for her health and the health of her fetus.
(Case study courtesy of Sharon Walker, RN, MSN.)
AMNIOTIC MEMBRANE COMPLICATIONS
Prelabor rupture of membranes (PROM) (previously known as premature rupture of membranes) refers to the rupture of membranes one hour or more before the onset of labor. Labor may be medically induced to reduce the risk of chorioamnionitis (infection of the chorion and amnion of the placenta), which can be life-threatening for the patient and fetus.
Preterm prelabor rupture of membranes (PPROM) (previously known as preterm premature rupture of membranes) refers to the rupture of membranes at approximately 23–37 weeks’ gestation. PPROM is often associated with preterm labor and birth. The most common identifiable risk factor for PPROM is genital tract infection.
PPROM can cause a variety of problems, especially for the fetus. Without the protective barrier of the amniotic membrane, the fetus is at a greater risk for the development of infection and preterm delivery. The fetus is also at risk for becoming septic after delivery. Additionally, without the cushioning of the amniotic fluid, there is a higher probability of umbilical cord compression as well as cord prolapse.
Medical Treatment
The first step in determining the appropriate course of action for patients with possible PROM or PPROM involves distinguishing amniotic fluid from urine or other vaginal discharge. Often, patients complain of a “sudden gush” and/or a continuous or intermittent trickle of fluid from the vagina once the membranes have actually ruptured.
The healthcare practitioner performs a sterile speculum examination to look for pooling of amniotic fluid near the cervix. Fluid may be observed as pooling on a sterile speculum exam. It may also be tested using nitrazine paper as well as via microscopic examination for the presence of ferning (the appearance of a fernlike pattern in a dried specimen of cervical mucus or vaginal fluid, which would indicate the presence of amniotic fluid). Commercial tests, such as AmniSure, may also be used to test for ruptured membranes. Ultrasound examination may be performed to determine the amount of available amniotic fluid after the rupture of membranes.
Medical treatment for patients with PROM or PPROM depends on a variety of factors. Gestational age, fetal lung maturity, available amniotic fluid, and etiology must be considered before deciding on treatment. Patients near term whose labor does not begin spontaneously following the rupture of membranes may be induced if the cervix is ripe. For preterm patients, providers and patients may desire to prolong the pregnancy to promote fetal lung maturity; such patients may be prescribed corticosteroids to promote fetal lung maturity until delivery occurs or until there is a need to induce labor.
Nursing Care
As with medical treatment, nursing care greatly depends on whether the medical diagnosis is PPROM or PROM. However, nursing care typically involves assisting the healthcare practitioner to confirm the rupture of membranes, monitoring the patient for infection and the presence of uterine contractions, and monitoring the status of the fetus. It is imperative that the nurse change patient underpads frequently and avoid unnecessary vaginal examinations to help prevent infection (and with PPROM to avoid decreasing the time until delivery) (Duff, 2022).
When caring for a patient with PPROM and PROM, the nurse should be prepared to address cord prolapse and compression, which can occur as the umbilical cord slips down in the pelvis. This is a life-threatening situation for the fetus; therefore, the fetus must be monitored closely. In the event of cord prolapse and compression, the nurse attempts to relieve pressure on the umbilical cord and instructs the patient to quickly move into the knee-chest or Trendelenburg positions. Oxygen is administered, and the healthcare practitioner notified immediately. Emergency cesarean section is likely.
Patient Teaching
It is important for patients with PPROM to understand the signs and symptoms that suggest infection as well as preterm labor, which often follows PPROM. The patient is watched for any of the following signs and symptoms:
- Fever >100.4 °F (>38 °C)
- Foul-smelling vaginal discharge or other signs of infection
- Uterine contractions or cramping (including tightening of the abdomen)
- Decreased fetal movement
In addition, patients are encouraged to avoid activities or objects that might induce labor or cause infection by exposing the cervix to bacteria. These include sexual activity, orgasm, nipple stimulation, tampons, and douches. Some patients may be placed on bed rest and should be encouraged to follow this directive to prevent preterm labor.
CASE
Neema, a 26-year-old in the 30th week of her second pregnancy, has come to the clinic for an additional prenatal visit. She states, “I came in because I’m not sure what’s going on down there. It feels like I’m peeing on myself, but I don’t think I am.” A small amount of clear liquid is noted on Neema’s peri-pad. She continues, “It all started yesterday morning, and when I told my husband, he said I should stay home from work, relax, and take a nice hot bath.”
A sterile speculum was used to sample the fluid pooled near the cervix. When tested using nitrazine paper and examined microscopically, the fluid is alkalotic and shows ferning. The AmniSure test is positive. Neema is not experiencing any cramping or uterine contractions. Fetal heart tones are strong and regular, and all of Neema’s vital signs are within normal limits. Neema asks, “Does this mean I will have a dry labor?”
Discussion
Neema has preterm prelabor rupture of membranes (PPROM). Neema’s nurse will monitor Neema’s temperature and report a reading higher than 100.4 °F (38 °C). The nurse will also question Neema about uterine tenderness and uterine contractions and note offensive-smelling vaginal discharge. Neema should avoid activities or objects that might bring about labor or cause infection. She will be told to avoid taking baths. Neema should be informed that because amniotic fluid is constantly being formed, she will not experience a dry labor. Neema’s healthcare practitioner may put her on bed rest with bathroom privileges.
(Case study courtesy of Sharon Walker, RN, MSN.)
PRETERM LABOR AND BIRTH
Preterm labor refers to labor that occurs after 20 weeks’ but before 37 weeks’ gestation. Preterm birth, a consequence of preterm labor, refers to delivery prior to 37 weeks’ gestation. Preterm birth is a significant contributor to infant mortality rates.
Maternal and Fetal Implications
Preterm labor and birth present a unique challenge to patients and their fetuses. Although most of the implications apply to the fetus, patients may suffer from stress due to the diagnosis of preterm labor and birth as well as from the causative agent. Specifically, patients may be experiencing preterm labor and birth due to conditions such as sepsis or stress.
The fetus is at great risk for delivering early as a result of preterm labor. The effects of preterm labor and birth depend on the gestational age of the fetus at delivery. The immaturity of fetal lungs in the presence of preterm labor and birth is a significant concern.
Signs and Symptoms
Patients presenting with preterm labor and birth often complain of feeling pressure in the pelvic area, abdominal and/or uterine cramping or contractions, painful or painless contractions, feeling as though the fetus is “balling up,” and/or constant back pain. Amniotic membranes may rupture prematurely, and a sudden gush or constant trickle of vaginal fluid may be noted.
Medical Treatment
Clinical criteria for a diagnosis of preterm labor include:
- Persistent uterine contractions (≥4 every 20 minutes or ≥8 every 60 minutes) and
- Cervical dilation ≥3 cm or cervical length <20 mm on transvaginal ultrasound or
- Cervical length 20 to <30 mm on transvaginal ultrasound and positive fetal fibronectin
(Lockwood, 2022)
Medical treatment for preterm labor and birth depends on the gestational age of the fetus. Generally, healthcare practitioners seek to avoid delivery of patients prior to 34 weeks’ gestation to allow further maturation of the fetal lungs. Glucocorticoids (betamethasone) are often prescribed to increase fetal lung maturity, tocolytics to control uterine contractions and delay birth so that glucocorticoids can take effect, antibiotics for group B streptococcal chemoprophylaxis, and magnesium sulfate for neuroprotection in offspring born preterm (Lockwood, 2022).
Nursing Care
Nursing care for patients experiencing preterm labor includes administering prescribed medications such as antibiotics, glucocorticoids, magnesium sulfate, and tocolytics, and preparing the patient for possible delivery. While hospitalized, patients are monitored for signs and symptoms of infection, which can lead to preterm labor. Fetal tachycardia indicates possible infection and should be evaluated immediately. Vital signs, contractions, and fetal status are assessed as ordered or according to institutional policy.
When patients are faced with the possibility of delivering a preterm infant, the situation may quickly become overwhelming to them. Although preterm labor and birth can occur rapidly, it is imperative that nurses address the emotional issues of the patient. Generally, this will involve answering patient questions about the status of the fetus and preparing the patient for the care required to prevent delivery or the necessary preparation for preterm delivery.
Patient Teaching
The major goal of teaching patients with preterm labor is to help them become aware of factors that may cause premature labor and delivery. If the acute episode of preterm labor has passed, patients may be discharged and taught to:
- Continue activities of daily living, but do not lift anything >20 pounds and avoid recreational exercise.
- Consider avoiding sexual activity if they experience an increased frequency or intensity of contractions afterward. It is possible that orgasm and prostaglandins in semen can increase myometrial activity.
- Avoid returning to work if it involves >40 hours/week, night shifts, prolonged standing, or heavy physical work.
(Caritis & Simhan, 2022)
POST-TERM PREGNANCY
Just as preterm delivery comes with complications, a post-term delivery can lead to complications as well. A post-term pregnancy is defined as ≥42 weeks’ gestation. Due to placental insufficiency or excessive fetal growth, maternal, fetal, and neonatal complications can occur. These include macrosomia (and possible associated surgical delivery or birth injury), intrauterine malnutrition, and perinatal mortality. It is recommended to induce at 41 weeks’ gestation in order to decrease the likelihood of complications.
CASE
Ciara phones the perinatal clinic. She is 18 years old and in the 32nd week of her second pregnancy. Ciara’s first child was born at 36 weeks’ gestation.
Ciara is sobbing over the phone and keeps repeating, “I don’t want it to happen again.” The nurse asks Ciara to take a deep breath, sit down, and explain how she is feeling. After a short time, Ciara states that she is having uterine contractions that are occurring every 10 minutes and lasting for 1–2 minutes. The contractions started about three hours ago and did not stop when she tried to walk. Asked about a gush of water from the vagina, she denies it. Ciara says, “I still feel the baby kicking. That’s a good thing, isn’t it? Did I make this happen?”
After reviewing her patient record, the nurse discovers that there is a history of social service intervention. As a result of Ciara’s impoverished circumstances, Ciara and her 3-year-old child receive nutritional support through the WIC (Women, Infants, and Children) program and live in a shelter to escape from an abusive cohabiting male.
Ciara is told to have someone bring her to the hospital as soon as possible. She states that she already called for a ride and that she should be arriving at the hospital within 30 minutes. The nurse tells Ciara to lie down on her left side, drink plenty of fluids, and wait for her ride.
Discussion
Ciara may be in preterm labor. She has several risk factors, including low socioeconomic status, significant life events (separation), anxiety, a history of preterm labor and birth, and poor nutrition. Ciara will be assessed for the condition of her cervix and amniotic membranes upon arriving at the hospital. Vital signs, contractions, and fetal status will be evaluated. She will also be observed for signs of infection and dehydration. She is very anxious, and because she has had a previous preterm birth, Ciara may have feelings of guilt that require reassurance and psychological support. The goal of her hospitalization would be to avoid delivery.
(Case study courtesy of Sharon Walker, RN, MSN.)
POSTPARTUM COMPLICATIONS
Despite the normalcy of childbirth, complications may arise that will have detrimental effects on the postpartum patient. In the week after delivery, leading causes of death included high blood pressure, infection, and severe bleeding. About 33% of maternal deaths happen one week to one year postpartum (CDC, 2019b). Healthcare professionals working with postpartum patients must have a clear understanding of these complications, including the signs and symptoms, nursing interventions, and treatment.
Postpartum Hemorrhage (PPH)
Postpartum hemorrhage is one of the leading causes of death among postpartum women. Traditionally, PPH has referred to a blood loss of ≥500 mL after a vaginal birth and ≥1,000 mL after a C-section. In 2017, the American College of Obstetricians and Gynecologists revised their definition to be a cumulative blood loss ≥1,000 mL, or bleeding associated with signs/symptoms of hypovolemia within 24 hours of the birth process (ACOG, 2017).
Postpartum hemorrhage is categorized as early or late. Early refers to a hemorrhage occurring within the first 24 hours after birth, while late refers to a hemorrhage occurring 24 hours to 12 weeks after delivery. PPH affects approximately 3% of deliveries and is on the rise (Belfort, 2022).
CAUSES AND INTERVENTIONS
Late postpartum hemorrhage is often caused by diffuse uterine atony or subinvolution of the uterus (uterus not returning to its normal size) caused by retained placental fragments and/or infection that prevent the uterus from contracting. In the case of retained placental fragments, clots develop around the retained fragments and hemorrhaging can occur days later when the clots are shed. The certified nurse-midwife or physician is responsible for examining the placenta after delivery and ensuring that it is intact; therefore, a late PPH is usually preventable.
Assessment and manual expression of placental fragments by the physician or nurse-midwife can often alleviate the problem; however, surgical intervention, such as a dilation and evacuation (D&E), may be necessary. With subinvolution and a late PPH, fundal massage, in addition to medications may be used to minimize bleeding. (The California Maternal Quality Care Collaborative [CMQCC, 2022] has created the OB Hemorrhage Toolkit to assist providers and clinical staff in recognizing and responding to hemorrhage.)
Thrombophlebitis
Patients can suffer from thrombophlebitis as a result of venous stasis and the normal hypercoagulability state of the postpartum period. Thrombophlebitis is an inflammation of the blood vessel wall in which a blood clot forms and causes problems in the superficial or deep veins of the lower extremities or pelvis.
The blood clot that develops in thrombophlebitis can lead to a life-threatening pulmonary embolism as a result of the clot detaching from the vein wall and blocking the pulmonary artery. The major signs of pulmonary embolism include dyspnea and chest pain.
In monitoring postpartum patients for the development or presence of thrombophlebitis, nurses assess for the presence of hot, red, painful, or edematous areas on the lower extremities or groin area. An elevated temperature may also be present. It is contraindicated to assess for a thrombophlebitis by eliciting a Homan’s sign.
Interventions to treat thrombophlebitis depend on the severity of the thrombosis. Usually, for superficial thrombosis, analgesics, bed rest, and elevation of the affected limb are enough to alleviate the problem. However, in the presence of a DVT, anticoagulants may be necessary. In addition to using compression stockings and applying warm, moist heat, patients are instructed to keep their legs elevated and uncrossed and to ambulate only after symptoms subside.
Infections
Postpartum infections are infections accompanied by a temperature of 38 °C or higher on two separate occasions during the first 10 days postpartum, exclusive of the first 24 hours (when low-grade fever is common and self-limited) (Berens, 2022a). Postpartum patients are carefully monitored for signs and symptoms of infection during this period. Common infections that may occur during the postpartum period include mastitis, endometritis, wound infections, and urinary tract infections.
MASTITIS
Mastitis is a localized, painful infection of the breast, which can progress to an abscess if not treated properly. It typically presents as a red, painful, firm, swollen area of one breast with accompanying fever >38.3 °C. The patient may also complain of myalgia, chills, malaise, and flu-like symptoms (Dixon, 2022).
Mastitis is less likely to occur with complete emptying of the breast and good breastfeeding technique. Thus, it is crucial that postpartum nurses teach breastfeeding patients proper latch-on technique and that they stress regular breastfeeding and allowing the breast to empty completely. Breastfeeding patients are also encouraged to avoid missed feedings and allowing the breast to become engorged.
Treatment for mastitis typically involves antibiotic therapy and regular breastfeeding or pumping the breast. Nurses can encourage these patients to apply cold or warm compresses to ease discomfort and to take analgesics as needed. Mastitis usually resolves quickly as long as patients continue to breastfeed or pump regularly.
ENDOMETRITIS
Endometritis is an infection of the uterus characterized by postpartum fever, midline lower abdominal pain, and uterine tenderness. Purulent lochia, chills, headache, malaise, and/or anorexia may also be present (Chen, 2022).
Endometritis is usually treated with broad-spectrum intravenous antibiotics and rest. Blood cultures to identify the causative organism of endometritis are performed if the patient does not respond to empiric therapy. White blood cell (WBC) counts are monitored. However, it is important to remember that the white blood cell count is normally elevated after delivery for a short period; continued monitoring of the WBC count is required in identifying endometritis and is likely to show a left shift and increasing number of neutrophils.
WOUND INFECTIONS
Commonly affected wound sites during the postpartum period include the perineum due to lacerations and episiotomies, and C-section incisions. As with all infections, every patient is at risk.
Wound infections typically exhibit redness, warmth, poor wound approximation, tenderness, and pain. If untreated, these patients may develop a fever and other symptoms of an infection, such as malaise. Blood cultures may be obtained to isolate the causative organism. Antibiotics will typically be administered, and drainage of the wound may be necessary.
Patients are taught proper handwashing and encouraged to maintain adequate fluid intake and increased protein intake to assist in wound healing. Wound infections can be intensely painful, especially in the perineum. Therefore, the nurse assists these patients in managing pain through the use of analgesics and positioning.
URINARY TRACT INFECTIONS (UTIs)
The risk of developing a UTI is high during the postpartum period. A woman’s urethra and bladder are often traumatized during labor and birth due to intermittent or continuous catheterizations and the pressure of the infant as it passes through the birth canal. Additionally, the bladder and urethra lose tone after delivery, making the retention of urine and urinary stasis common. Women may also develop a UTI due to epidural anesthesia or vaginal procedures (Berens, 2022a).
Patients with urinary tract infections often complain of frequent, urgent, and/or painful urination with suprapubic pain. A low-grade fever and hematuria may also be present. Urinary tract infections are treated with antibiotics, and it is important that these patients drink adequate fluids to flush bacteria out of the system.
Postpartum Depression
Postpartum depression is a serious and debilitating depression that affects many women throughout the world. Postpartum depression occurs in approximately 9% of women after delivery.
Symptoms are generally noted within the first three months but may occur up to a year after delivery. They typically include changes in sleep, energy, appetite, weight, and libido. Other symptoms include lack of energy to the point of not getting out of bed for hours; but this should be distinguished from the normal lack of energy that results from sleep deprivation of caring for an infant. Additional symptoms include anxiety and panic attacks; irritability and anger; feeling inadequate, overwhelmed, or unable to care for the baby; and feelings of shame, guilt, and having failed as a mother (Viguera, 2022).
Adverse outcomes of postpartum depression can include impaired bonding, impaired infant and child development, interference in the relationship with one’s partner, suicidal ideation, and infanticide (Viguera, 2022).
It is the responsibility of nurses to assess postpartum patients for signs and symptoms of postpartum depression. Various assessment tools are available, including the Edinburgh Postnatal Depression Scale (EPDS). This tool is quick and provides a simple means to assess patients while at the hospital, during postpartum home visits, and during postpartum follow-up clinic visits. This tool can also be used to assess mothers at pediatric follow-up visits. (See “Resources” at the end of this course.)
After screening and assessment, women who are at risk for developing (or who are suffering from) postpartum depression can be referred to the appropriate healthcare professional for follow-up and treatment. Treatment may include a combination of psychotherapy, social support, and medication. Nurses can support these patients in the healing process at follow-up appointments and during home visits, including encouraging adequate nutrition, rest, relaxation, and exercise.
Hypertension
Postpartum hypertension has been seen in as many as 20% of all postpartum individuals. It can be prolonged gestational hypertension/preeclampsia or new onset (August, 2022). Postpartum treatment is similar to treatment during pregnancy with the use of antihypertensives and/or magnesium sulfate (in the setting of preeclampsia). Additionally, furosemide may be used.
Postpartum patients must be educated on the signs and symptoms of hypertension/preeclampsia including headaches and visual changes.
POSTPARTUM DISCHARGE INSTRUCTIONS
Postpartum patients and their families are instructed to call the healthcare provider if the patient experiences any of the following:
- Excessive postpartum bleeding (e.g., bleeding that saturates a peripad within an hour)
- Fever
- New or worsening perineal or uterine pain
- Dysuria
- High blood pressure and/or headache/visual changes
- Breast problems
- Dyspnea, chest pain, leg pain or swelling
- Significant mood disturbance (e.g., affecting relationships or normal activity)
(Berens, 2022b)
CONCLUSION
Pregnancy, labor, and birth are a wondrous time in the lives of many. However, this time can be clouded by a variety of complications that affect the patient and fetus. Fortunately, with early identification and treatment of complications and their side effects, patients and their infants have a greater chance of survival and the potential to thrive after delivery.
Nurses play a special role in ensuring the safety of the patient and fetus during all phases of pregnancy, delivery, and postpartum. They must be knowledgeable about complications that can occur and be ready to act on behalf of the patient and fetus. This is the responsibility and goal of the nurse.
Most hospitals and birthing centers provide evidence-based guidelines for nurses caring for patients experiencing complications during their pregnancies. Nurses must provide comprehensive care that follows the recommendations of their facilities.
RESOURCES
American Society of Reproductive Medicine
Association of Women’s Health, Obstetric, and Neonatal Nurses
Edinburgh Postnatal Depression Scale (EPDS)
Gestational diabetes (American Diabetes Association)
Gestational trophoblastic disease (National Cancer Institute)
Hyperemesis education and research (HER Foundation)
REFERENCES
NOTE: Complete URLs for references retrieved from online sources are provided in the PDF of this course.
American College of Obstetricians and Gynecologists (ACOG). (2017). Postpartum hemorrhage. Practice bulletin 183. https://www.acog.org
Ananth CV & Kinzler WL. (2022). Placental abruption: Pathophysiology, clinical features, diagnosis, and consequences. UpToDate. https://www.uptodate.com
August P. (2022). Treatment of hypertension in pregnant and postpartum patients. UpToDate. https://www.uptodate.com
Belfort MA. (2022). Overview of postpartum hemorrhage. UpToDate. https://www.uptodate.com
Berens P. (2022a). Overview of the postpartum period: Disorders and complications. UpToDate. https://www.uptodate.com
Berens P. (2022b). Overview of the postpartum period: Normal physiology and routine maternal care. UpToDate. https://www.uptodate.com
Berghella V & Hughes BL. (2022). COVID-19: Overview of pregnancy issues. UpToDate. https://www.uptodate.com
California Maternal Quality Care Collaborative (CMQCC). (2022). OB hemorrhage toolkit V3.0 Errata 7.18.22. https://www.cmqcc.org
Caritis S & Simhan HN. (2022). Management of pregnant women after resolution of an episode of acute idiopathic preterm labor. UpToDate. https://www.uptodate.com
Centers for Disease Control and Prevention (CDC). (2019a). Pregnancy-related deaths. https://www.cdc.gov
Centers for Disease Control and Prevention (CDC). (2019b). Pregnancy-related deaths happen before, during, and up to a year after delivery. https://www.cdc.gov
Chen KT. (2022). Postpartum endometritis. UpToDate. Retrieved from https://www.uptodate.com
Cunningham FG. (2022). Normal reference ranges for laboratory values in pregnancy. UpToDate. https://www.uptodate.com
Dixon JM. (2022). Lactational mastitis. UpToDate. https://www.uptodate.com
Duff P. (2022). Preterm prelabor rupture of membranes: Clinical manifestations and diagnosis. UpToDate. https://www.uptodate.com
Durnwald C. (2022a). Gestational diabetes mellitus: Screening, diagnosis, and prevention. UpToDate. https://www.uptodate.com
Durnwald C. (2022b). Gestational diabetes mellitus: Glucose management and maternal prognosis. UpToDate. https://www.uptodate.com
Kruskal JB. (2022). Diagnostic imaging in pregnant and nursing patients. UpToDate. https://www.uptodate.com
Lockwood CJ. (2022). Preterm labor: Clinical findings, diagnostic evaluation, and initial treatment. UpToDate. https://www.uptodate.com
Lockwood CJ & Magriples U. (2022). Prenatal care: Patient education, health promotion, and safety of commonly used drugs. UpToDate. https://www.uptodate.com
Lockwood CJ & Russo-Stieglitz K. (2022a). Placenta previa: Epidemiology, clinical features, diagnosis, morbidity and mortality. UpToDate. https://www.uptodate.com
Lockwood CJ & Russo-Stieglitz K. (2022b). Placenta previa: Management. UpToDate. https://www.uptodate.com
Melvin LM & Funai EF. (2022). Gestational hypertension. UpToDate. https://www.uptodate.com
Office on Women’s Health. (2021). Pregnancy complications. https://www.womenshealth.gov
Petersen EE, Davis NL, Goodman D, et al. (2019). Vital signs: Pregnancy-related deaths, United States, 2011–2015, and strategies for prevention, 13 states, 2013–2017. MMWR, 68(18), 423–9. https://www.cdc.gov
Prager S, Micks E, & Dalton VK. (2022a). Pregnancy loss (miscarriage): Management techniques. UpToDate. https://www.uptodate.com
Prager S, Micks E, & Dalton VK. (2022b). Pregnancy loss (miscarriage): Terminology, risk factors, and etiology. UpToDate. https://www.uptodate.com
Ramsey PS & Schenken RS. (2022). Obesity in pregnancy: Complications and maternal management. UpToDate. https://www.uptodate.com
Sibai BM. (2022). HELLP syndrome (hemolysis, elevated liver enzymes, and low platelets). UpToDate. https://www.uptodate.com
Smith JA, Fox KA, & Clark SM. (2022a). Nausea and vomiting of pregnancy: Clinical findings and evaluation. UpToDate. https://www.uptodate.com
Smith JA, Fox KA, & Clark SM. (2022b). Nausea and vomiting of pregnancy: Treatment and outcome. UpToDate. https://www.uptodate.com
Tulandi T. (2022a). Ectopic pregnancy: Choosing a treatment. UpToDate. https://www.uptodate.com
Tulandi T. (2022b). Ectopic pregnancy: Epidemiology, risk factors, and anatomic sites. UpToDate. https://www.uptodate.com
Tulandi T. (2022c). Ectopic pregnancy: Methotrexate therapy. UpToDate. https://www.uptodate.com
Viguera A. (2022). Postpartum unipolar major depression: Epidemiology, clinical features, assessment, and diagnosis. UpToDate. https://www.uptodate.com
Wolf LA, Delao AM, Zavotsky KE, & Baker, KM. (2021). Triage decisions involving pregnancy-capable patients: Educational deficits and emergency nurses’ perceptions of risk. Journal of Continuing Education in Nursing, 52(1). https://wispqc.org




Customer Rating
4.9 / 437 ratings