Obesity in America
Management and Treatment in Children, Adolescents, and Adults
Online Continuing Education Course
Course Description
The United States is in an obesity epidemic. This course focuses on prevention for overweight and obesity. Often, the disease starts in childhood, continues through adolescence, and remains prevalent in adulthood. This continuing education course highlights the comorbidities and consequences and explains the effects of anti-obesity stigma. Strategize with your patients to prevent, manage, and treat this condition successfully.
Note: This course is also available as part of a package. See Nursing CEU Bundle - 30 ANCC Hours
Course Price: $47.00
Contact Hours: 9
Pharmacotherapeutic Hours: 0.25
Course updated on
October 4, 2022
"Thank you for presenting this material with such compassion and deep knowledge of the plight and physical challenges of obese patients." - Barbara, RN in North Carolina
"Excellent information for me to share in both my professional and personal life. Thank you!" - Rebecca, RN in California
"Great course! Information I can use both professionally and personally." - Patricia, OT in Missouri
"This was extremely well presented, and I gained more understanding of the topic." - Elizabeth, RN in New Hampshire
Obesity in America
Management and Treatment in Children, Adolescents, and Adults
Copyright © 2022 Wild Iris Medical Education, Inc. All Rights Reserved.
LEARNING OUTCOME AND OBJECTIVES: Upon completion of this course, you will have increased your knowledge about obesity, including its prevalence, consequences, contributing factors, interventions, and approaches to prevention and treatment. Specific learning objectives to address potential knowledge gaps include:
- Describe the prevalence and impact of overweight and obesity in U.S. adults, children, and adolescents.
- Examine the pathogenesis and etiology of overweight and obesity.
- Discuss the comorbidities and consequences of obesity.
- Explain the psychosocial effects of stigma and weight bias.
- Describe components of assessment for overweight or obesity.
- Summarize strategies for management and treatment of overweight and obesity in adults, children, and adolescents.
- Discuss considerations in caring for the bariatric patient.
- Outline ways to prevent overweight and obesity in all age groups.
TABLE OF CONTENTS
- Introduction
- What Causes Obesity?
- Comorbities and Consequences of Obesity
- Assessing for Overweight and Obesity
- Management and Treatment of Obesity in Adults
- Management and Treatment of Obesity in Children and Adolescents
- Caring for the Bariatric Patient
- General Strategies for Overweight and Obesity Prevention and Advocacy
- Conclusion
- Resources
- References
INTRODUCTION
According to the World Health Organization (2022a), obesity has reached epidemic proportions around the globe, nearly tripling since 1975. Today, most of the world’s population lives in countries where being overweight or obese causes more deaths than being malnourished and underweight.
The fundamental cause of overweight and obesity is an energy imbalance that results from consuming more calories and expending less energy. Around the world there has been an increase in the intake of energy-dense foods and a decrease in physical activity due to the increasingly sedentary nature of many types of work, changing modes of transportation, and increasing urbanization.
These are often the result of environmental and societal changes associated with development and the lack of supportive policies in the areas of health, agriculture, transport, urban planning, environment, food processing, distribution, marketing, and education (WHO, 2022a). This global problem has profound social, economic, and health implications for individuals and communities.
Defining Obesity
Obesity is defined by the Obesity Medicine Association (2021) as “a chronic, relapsing, multifactorial, neurobehavioral disease, wherein an increase in body fat promotes adipose tissue dysfunction and abnormal fat mass physical forces, resulting in adverse metabolic, biomechanical, and psychosocial health consequences.”
The American Medical Association (2013) classified obesity as a disease after an overwhelming vote in favor and defined it as a state of excessive fat accumulation that presents a risk to health. Classifying obesity as a disease is the first step toward objectively assessing the factors that lead to it and working toward its prevention and treatment. Some have countered this by saying that obesity is a risk factor for disease but not a disease itself. By such reasoning, however, a condition such as hypertension should not be classified as a disease.
Arguments for why obesity is a disease and not merely an aesthetic issue include:
- Genes may play a role, as well as other diseases or disorders, such as hypothyroidism, Cushing’s disease, and polycystic ovarian syndrome.
- Taking certain medications for other health conditions can lead to weight gain (e.g., antidepressants).
- Each person has their own base metabolic rate, so for two people who are the same height and eat the same diet, one may be obese while the other is not.
- Some aspects of obesity are preventable; however, it is known that some people may make appropriate changes in diet and exercise yet still be unable to lose significant amounts of weight.
Arguments made by those who believe obesity is not a disease include:
- There is no clear way to measure obesity. Body mass index does not apply to everyone (e.g., endurance athletes and weightlifters).
- Obesity doesn’t always reflect poor health. It can be a risk factor but does not always cause negative effects.
- Defining obesity as a disease may foster a culture of personal irresponsibility.
- Defining obesity as a disease may increase discrimination for those with obesity.
Obesity is a complex, multifactorial disease scientifically shown to be brought on and sustained by many factors both within and beyond the individual’s control. Much research has been done and continues to be done into what has now been clearly identified as a major disease state involving personal, societal, and environmental factors. Attitudes must shift from solutions that emphasize an individual-oriented responsibility to include these factors, and healthcare professionals must strive to eliminate stigmatizing individuals with excessive weight and obesity in order to provide the healthcare they require.
HOW OVERWEIGHT AND OBESITY ARE DETERMINED
To determine whether an individual is overweight or obese, a common, inexpensive, albeit imperfect, measure of obesity is the body mass index (BMI), a person’s weight (in kilograms) divided by the square of their height (in meters). A person with a BMI ≥25 kg/m2 is considered overweight, ≥30 obese, and ≥40 severely (morbidly) obese (WHO, 2022a).
For example, a person who weighs 132 kg (291 pounds) and stands 1.83 meters tall (6 feet) has a BMI of 132 divided by 1.832, or 39.4 kg/m2, which is considered obese.
(See also “Body Mass Index” later in this course.)
Scope of the Problem
GLOBALLY
In 2020, there were an estimated 500 million adults in the world who were obese and nearly 1.8 billion adults 18 years and older who were overweight. In 2020, 39 million children under the age of 5 and over 340 million children and adolescents ages 5–19 were overweight or obese. It is estimated that if the issue is not adequately addressed, an estimated 1 billion adults will be obese by 2030.
In 2021, the small island nation of Nauru in the southwestern Pacific had a 61% obesity prevalence, the highest in the world; the country with the lowest prevalence (2%) was Vietnam (CDC, 2021a; WPR, 2021).
IN AMERICA
Obesity affects some groups in the United States more than others:
- By race/ethnicity, non-Hispanic Black adults had the highest age-adjusted prevalence of obesity, followed by Hispanic adults, non-Hispanic White adults, and non-Hispanic Asian adults.
- By age:
- More than 1 in 3 adults and about 1 in 5 children are considered to be obese.
- Obesity prevalence was 40% among adults ages 20–39 years, 45% among adults ages 40–59 years, and 43% among adults ages 60 and older.
- The obesity rate among youth ages 2–19 years is nearly 20%, or about 14.4 million in total.
- By sex:
- Overweight and obesity in adults have increased from 21% in men and 24% in women to almost 40% in both sexes in the past four decades.
- The percentage of men who are defined as overweight is higher than that of women, but the percentage of women who have severe obesity is higher than that of men with severe obesity.
- By educational level, men and women with college degrees had lower obesity prevalence compared with those with less education.
- By income:
- Among non-Hispanic White and Hispanic men, obesity prevalence was lower in the lowest and highest income groups compared with the middle-income group.
- Among non-Hispanic Black men, obesity prevalence was higher in the highest income group compared to the lower.
- Among non-Hispanic White, non-Hispanic Asian, and Hispanic women, obesity prevalence was lower in the highest-income group compared to the middle- and lowest-income groups.
- Among non-Hispanic Black women, there was no difference in obesity prevalence by income.
GEOGRAPHIC DISPARITIES IN OBESITY
Obesity prevalence varies across states and territories. Regionally, the Midwest and South have the highest prevalence of obesity, followed by the West and the Northeast.
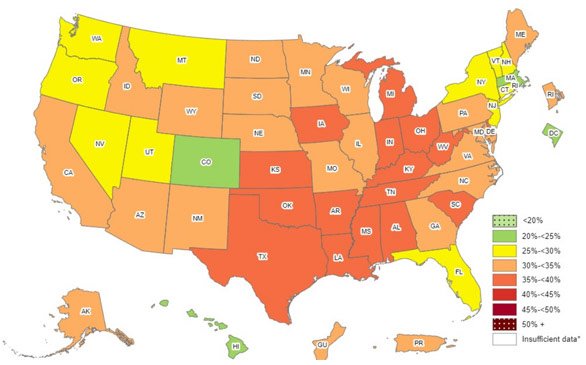
Prevalence of self-reported obesity among U.S. adults by state and territory. (Source: CDC, 2021c.)
ECONOMIC AND SOCIAL IMPACTS
Obesity and the associated health problems that develop as a result have a significant economic impact on the U.S. healthcare system, having risen to nearly $1.4 trillion and equaling 6.76% of the Gross Domestic Product (GDP) in 2018. This includes both direct and indirect costs. Direct costs may be incurred for preventive care services, diagnostic testing, and treatment. Indirect costs related to illness and death are estimated at over $1 trillion for lost workdays or decreased productivity at work.
In 2019 adult obesity was linked to $3,097 in excess annual costs per person, and childhood obesity was associated with over $100 per child. Healthcare expenditures for children with severe obesity have increased by $300 per year.
Obesity-related costs increase with age, starting at around age 30 and increasing until about age 65, at which point the gap between obesity and nonobesity begins to narrow. This is partly due to increasing costs as a result of aging among those with a normal weight and increased mortality among individuals with severe obesity.
Overall per capita spending is higher for adult women than adult men but lower for girls and boys. The highest estimated costs occur in 60- to 70-year-olds.
Medical expenses and lost workdays among obese individuals represent only a portion of obesity-related costs. Other related costs can include the necessity for informal caregivers and lost productivity.
In addition, there are social and emotional effects of obesity, including discrimination, lower wages, lower quality of life, and an increased risk for depression (Milken Institute, 2020; Ward et al., 2021).
OBESITY AND COVID-19
More than 900,000 adult COVID-19 hospitalizations occurred in the United States between the start of the pandemic and November 2020. Models estimate that 271,800 (30.2%) of those hospitalizations were attributed to obesity. Obese children diagnosed with COVID-19 have a 3-times higher risk of hospitalization and 1.5-times higher risk of severe illness when hospitalized.
(CDC, 2021b)WHAT CAUSES OBESITY?
The pathogenesis of obesity involves the regulation of energy utilization, appetite, physical activity, and complex interactions with underlying hereditary and environmental factors.
Basically, obesity results from a chronic positive energy balance regulated by a complex interaction between endocrine tissues and the central nervous system. Obesity is characterized by the accumulation of excessive body fat (adipose tissue) and a mild state of chronic inflammation of this tissue that leads to a defective hormonal and immune system.
Depending on location, types of adipose tissue are parietal or visceral. Parietal is located under the skin, and visceral surrounds the internal organs. Compared to subcutaneous fat, visceral fat is more likely to raise the risk for serious medical issues. Visceral fat manufactures more of the proteins that cause inflammation in tissues and organs and narrowing of blood vessels.
Adipose tissue has always been considered a passive fuel reservoir and protection for internal organs, but it is recognized now as an endocrine organ that secretes multiple bioactive substances, including adipocytokines and hormones. It represents the largest endocrine gland in the human body. Adipocytokines are mediators that exert pro-inflammatory or anti-inflammatory actions. They regulate energy balance, food intake and satiety, and metabolism of steroid hormones; are involved in insulin sensitivity and appetite; and play a role in blood coagulation. Ongoing investigations into the complexities of adipocyte metabolism has improved the understanding of the pathogenesis of obesity.
The most important adipose tissue hormone secreted is leptin, a negative feedback signal that acts on the hypothalamus to alter the expression of several neuroendocrine peptides that regulate energy intake and expenditure. Leptin controls appetite intensity by signaling the brain to stop eating and helps the brain regulate how much energy the body burns throughout the day. Central resistance to leptin results in a feeling of hunger all the time and is a prominent factor leading to obesity. The discovery of immunological abnormalities in obesity related to leptin has given a new perspective to the understanding of obesity (Vaskovic, 2021; Khana & Rehman, 2022; Saber, 2021a; Hamdy, 2022).
The factors that contribute to the pathogenesis of obesity are complicated and involve much more than simply eating more food than the body requires. This has been the prevailing belief in the past, but today researchers recognize the influence of many factors that are unique to each individual. Currently, these causative factors for obesity have been identified:
- Genetics
- Epigenetics and obesogens
- Endocrine diseases
- Inflammation and infection
- Stress
- Gut microbiota
- Prenatal factors
- Postnatal factors
- Ultraprocessed foods
- Medications
- Obesogenic environment
- Food availability and access
- Culture and ethnicity
- Parenting style
- Work environment and occupation
- Food marketing
- Sleep deprivation
- Circadian misalignment
Genetics
Twin and adoptee studies have demonstrated the heritability of obesity to be as high as 75%. These studies show that obese individuals who were raised separately followed the same weight pattern as that of their biological parents or their identical twin. A person’s metabolic rate, spontaneous physical activity, and thermic response to food appear to be heritable to some extent. A strong genetic component underlying the large variations in body weight also determines a person’s response to the environment.
Obesity is classified as monogenetic, polygenetic, or syndromic.
MONOGETIC OBESITY
Monogenetic obesity is caused by rare mutations of one gene, typically causing severe early-onset obesity with abnormal feeding behavior and endocrine disorders. Studies about common or polygenic obesity have found over 900 genetic variants associated with obesity. Some genes associated with monogenetic severe obesity are described below:
- Leptin (LEP) mutations cause rapid weight gain after normal birth weight as a result of intense hyperphagia (intense hunger and excessive eating).
- Leptin receptor (LEPR) can cause a phenotype similar to that of leptin deficiency.
- Proopiomelanocortin (POMC) is involved in appetite regulation.
- Melanocortin-4 receptor (MC4R) deficiency in children results in early-onset obesity with hyperphagia and food-seeking behavior in early childhood.
- PR proconvertase 1 (PCSK1) is involved in the regulation of food ingestion, glucose, and energy homeostasis.
- Single-minded 1 (SIM1) deletions or mutations are associated with hyperphagia and food impulsivity.
- Brain-derived neurotrophic factor (BDNF) is implicated in the regulation of food intake and body weight.
POLYGENETIC OBESITY
Polygenetic obesity (also referred to as common obesity) is associated with several variants of different genes. Many of these genes are involved in neurogenesis, in the development of the central nervous system, and in pathways such as appetite and food intake regulation. Some of them are related to synaptic function, neurotransmitter signaling, and energy homeostasis. Genes associated with polygenetic obesity include:
- Melanocortin-4 receptor (MC4R)
- Proopiomelanocortin (POMC)
- Fat mass and obesity associated gene (FTO) (the first gene found to be associated with obesity)
- Neurexin III (NRXN3)
- Niemann-Pick disease, type C1 (NPC1)
- Neuronal growth regulator 1 (NEGRI)
- Glucosamine-6-phosphate deaminase 2 (GNPDA2)
- Mitochondrial carrier 2 (MTCH2)
- ETS Translocation variant 5 (ETV5)
SYNDROMIC DISORDERS OF OBESITY
Syndromic disorders of obesity are different from common obesity. They are characterized by early-onset, severe obesity and often are associated with hyperphagia.
- Alström syndrome is a disorder caused by mutations in the ALMS1 gene. In addition to severe obesity beginning in early life, the disorder results in short stature in adulthood, progressive visual and auditory impairment, insulin resistance, type 2 diabetes, hyperlipidemia, and progressive kidney dysfunction.
- Bardet-Biedl syndrome results from mutations in multiple BBS genes in children ages 1–2 years, causing central obesity, intellectual disability, hypotonia, retinitis, polydactyly, glucose intolerance, deafness, and renal disease.
- Beckwith-Wiedemann syndrome (also known as Laurence-Moon-Biedl syndrome) is caused by multiple genetic mutations, resulting in hyperinsulinemia, hypoglycemia, hemihypertrophy, and intolerance of fasting.
- Carpenter syndrome results from a mutation in the RAB23 gene, causing central obesity, intellectual disability, short stature, brachycephaly, polydactyly, syndactyly of feet, cryptorchism, and hypogonadism in males.
- Cohen syndrome is caused by a mutation in the COH1 gene, resulting in mid-childhood central obesity, intellectual disability, microcephaly, small hands and feet, cryptorchidism, hypotonia, and long, thin fingers and toes.
- Prader-Willi syndrome is caused by a mutation in the NDN gene, resulting in generalized obesity in children age 1–3 years. It is characterized by faltering early growth followed by hyperphagia and increased weight gain by age 2–3 years. It also results in mild to moderate cognitive deficit, microcephaly, short stature, and delayed puberty.
- Down syndrome is caused by an extra chromosome and results in distinctive physical features, developmental challenges, and increased leptin levels, which correlates with obesity.
(Flores-Dorantes et al., 2020; Perrault & Rosenbaum, 2021; Schwarz, 2020)
Epigenetics and Obesogens
Environmental epigenetics looks at how chemicals or other environmental exposures can interfere with gene expression and thereby disrupt development. Epigenetics affects how genes are “read” by cells and subsequently how they produce proteins. Epigenetics is the study of gene expression, the switching on and off of gene action without causing a mutation (a change in the genetic code, or DNA). Gene expression signals the cells in the body on how and when to differentiate, a process through which a cell changes to become a more specialized type of cell.
When gene expression is altered—for example, by exposure to certain chemicals, radiation, or dietary nutrients—abnormal development of cells, organs, and systems can occur. Scientists recognize that these substances, referred to as obesogens, are endocrine disruptors that interfere with hormones that play a role in metabolism. Of particular importance, the critical window of exposure to obesogens is either during the prenatal or neonatal period, when the body’s weight-control mechanisms are being developed and can induce effects that manifest later in life.
Obesogens alter how fat cells develop, increasing the body’s fat cells. In some instances, these new cells become unusually large, allowing for fat to build up in the body, which leads to weight gain. These substances also may block fat-burning so that cells are unable to release stored fat. Obesogens can likewise alter appetite by affecting the hypothalamus, leading to a tendency to compulsively eat and not stop even if the person may no longer be hungry. Obesogens can also act indirectly to promote obesity by altering basal metabolic rate and gut microbiota to promote food storage (Brennan, 2021a; NIEHS, 2021a).
Chemicals that are classified as obesogens include:
- Cigarette smoke (nicotine, polycyclic aromatic hydrocarbons [PAHs], acrylamide). Acrylamide is also found in foods and can be formed as an unintentional byproduct of frying, baking, or roasting.
- Outdoor pollution:
- Byproducts of fossil fuel burning, including diesel exhaust
- Noxious gases (sulfur dioxide, nitrogen oxides, carbon monoxide, chemical vapors, etc.)
- Ground-level ozone (a highly reactive form of oxygen and a primary component of urban smog)
- Tributyltin (TBT), which is a chemical widely used as a fungicide and heat stabilizer in polyvinyl chloride (PVC) piping. Exposure can occur via diet (such as seafood contaminated by TBT used in marine shipping), surface disinfectants, laundering sanitizers, and rodent repellents. Placental TBT has been found to be associated with a trend toward higher weight gain, but only in the first three months of life. Prenatal exposure to TBT results in increased lipid accumulation, increased adipose tissue mass, and reduced muscle mass (Egusquiza & Blumberg, 2020).
- Flame retardants. There are hundreds of different flame retardants, which are grouped based on whether they contain bromine, chlorine, phosphorus, nitrogen, metals, or boron. These chemicals can get in the air, water, and soil during manufacture; can leak from products into dust and air and then get on hands and food; and can be found in some electronic waste. Children are particularly vulnerable to their effects and have been found to have higher concentrations of them in their bodies than adults. These chemicals do not break down easily and can remain persistent in the environment for years; they can also bioaccumulate (build up in people and animals over time) (NIEHS, 2021b).
- Phthalates are a broad class of chemicals that are added to many consumer products to make them softer and promote flexibility, such as in tubing and vinyl flooring. They can be present in cosmetics, wood finishes, blood bags, building products, food packaging, and children’s toys (NIEHS, 2021c).
- Bisphenol A (BPA), produced in large quantities and used primarily in the production of polycarbonate plastics and epoxy resins, is linked to childhood obesity. BPA is an ingredient in some food and drink packaging, such as water and infant bottles and coated metal products (food cans, bottle tops, and water supply pipes); medical devices; compact discs; and as a developer in cash register receipts. BPA is also used in some dental sealants and composites (Amato et al., 2021).
- Pesticides, including herbicides, insecticides, fungicides, disinfectants, and compounds used to control mice and rats. Less well known are attractants, plant defoliants, swimming pool treatment, and plant growth regulators (EPA, 2021a).
- Polychlorinated biphenyls (PCBs) are industrial chemicals used widely in the past in products such as paints, cements, fluorescent light ballasts, sealants, and adhesives. They were banned in 1970 but are still present in air, water, soil, homes, communities, and bodies, since they do not break down easily. Although it is illegal to manufacture PCBs, some continue to be produced in the process of making pigments (e.g., for paints, inks, cosmetics, etc.). Because PCBs build up in the fat of animals, a major exposure for many people comes from food, particularly meat, dairy, and fish. PCBs are also present in older buildings such as schools (Fox-Rawlings, 2022; EPA, 2021b).
Endocrine Diseases
Along with the hormones released from adipocytes, other hormones secreted by the endocrine system can be involved in conditions that result in obesity. These endocrine conditions can include:
- Hypothyroidism
- Polycystic ovarian syndrome
- Hyperandrogenism in females
- Cushing’s syndrome
- Hypothalamic disorders
- Hypogonadism in males
- Growth hormone deficiency
- Pseudohypoparathyroidism
The mechanisms for the development of obesity vary in accordance with the endocrine condition. Hypothyroidism, for example, involves an accumulation of fluid-retaining hyaluronic acid, resulting in excess retention of salt and water, which is associated with changes in body weight and composition. It also affects body temperature, energy expenditure, food intake, and glucose and lipid metabolism (ATA, 2022).
Polycystic ovarian syndrome interferes with the body’s ability to use insulin. High insulin levels increase the production of male hormones and obesity. Because it is triggered by male hormones, the weight gain is typically in the abdomen (Watson, 2020).
In Cushing’s syndrome, an interaction with thyroid and growth hormone increases the levels of cortisol in the body and plays an important role in increased adipocyte differentiation and adipogenesis. Increased levels of cortisol lead to a build-up of fat in characteristic sites such as the face, upper back, and abdomen (Mayo Clinic, 2021a).
Hypothalamic Obesity
Hypothalamic obesity is a rare syndrome caused by damage to the ventromedial or paraventricular region of the hypothalamus or the amygdala as a result of trauma, tumor, inflammatory disease, surgery in the posterior fossa, or increased intracranial pressure. These regions of the brain are responsible for the integration of metabolic information concerning nutrient stores with afferent sensory information about food availability. When this area is damaged, hyperphagia develops and obesity follows (Perreault & Bessesen, 2021).
Inflammation and Infection
Systemic inflammation makes the body more prone to insulin resistance, type 2 diabetes, and cardiovascular disease, which can lead to weight gain. The adipose tissue is known to be a storage place for various cytokines, especially interleukin 6 (IL6) and tumor necrosis factor (TNF). Chronic exposure to elevated IL6 is associated with the development of insulin resistance, metabolic syndrome, and type 2 diabetes.
A high-normal level of procalcitonin (PCT) reflects a state of inflammation and has been shown to be associated with central obesity but not with insulin resistance in obese patients.
There is also data suggesting that an infective cause may exist for obesity. Adenovirus-36 infection is associated with obesity in animal studies and in humans. The prevalence of this infection is 20% to 30% in people who are obese vs. 5% in people who are not. The role of infection in the pathogenesis of obesity, however, remains unclear (Hamdy, 2022; Lutz, 2020).
Stress
Research has shown that stress response may play a major role in the development and maintenance of obesity due to increased glucocorticoid exposure. There are many pathways that connect stress and obesity:
- Stress interferes with cognitive processes such as self-regulation abilities to control food intake.
- Stress can affect behavior by:
- Inducing overeating and consumption of foods that are high in calories, fat, or sugar
- Decreasing physical activity
- Shortening sleep
- Stress triggers physiological changes in the hypothalamic-pituitary-adrenal axis, reward processing in the brain, and possibly the gut microbiota.
- Stress can stimulate production of biochemical hormones and peptides such as leptin, ghrelin, and neuropeptide Y, all of which are involved in regulating food intake.
- Obesity itself can increase stress due to the high prevalence of stigmatization.
(Tomiyama, 2019)
Gut Microbiota
The human gastrointestinal tract is populated densely with bacteria, fungi, archaea, and viruses, collectively referred to as gut microbiota (GM). These microorganisms are important for body homeostasis. Because acids in the stomach and bile acids and pancreatic juice in the duodenum and jejunum can inhibit the growth of microorganisms, most inhabit the large intestine. Each person acquires their own unique microbiota, which begins to develop in infancy and is affected by the mother’s health, the type of delivery, breastfeeding history, age, use of antibiotics, geography, and diet—dietary habits being the main contributors to the diversity of the human gut microbiota.
GM influences how food is digested and absorbed and how dietary fats are stored. The microbiota may also impact the production of hunger hormones such as ghrelin. An unhealthy GM can increase inflammatory markers, which may result in weight gain and metabolic disease.
Endogenous microbiota can impact body immune response and metabolic homeostasis. Certain gut microbial strains have been shown to inhibit or attenuate immune responses related to chronic inflammation in experimental models, suggesting that specific species may play either a protective or pathogenic role in the progression of obesity. Obese patients have been found to have less diversity and richness in the bacterial component of their gut microbiota than normal-weight subjects and also show an increased ratio of Firmicutes to Bacteroidetes (the most common organisms in the fecal microbiota) regardless of dietary intake (Palmer, 2021).
Clinical trials are currently being conducted to verify findings obtain in studies using mice where fecal samples are transplanted from human twins, one obese and one lean into germ-free mice. The studies so far indicate that stool from the obese twin leads to increased mass in the mice, but does not when transplanting from the lean twin (NIH, 2021a).
Prenatal Factors
Intrauterine environment can shape the trajectory of weight gain and body fatness throughout the course of life. Three prenatal factors are the mother’s smoking habits, weight gain, and blood sugar levels during pregnancy.
MATERNAL PRENATAL SMOKING
Studies have shown a consistent connection between maternal smoking in pregnancy as well as exposure to secondhand smoke and an increased risk of children being overweight and obese by 3 years of age. In a meta-analysis of 14 studies, maternal smoking during pregnancy was associated with a 50% higher risk of childhood obesity. The mechanisms to explain the effect of smoking are not as yet understood but may result from fetal exposure to nicotine, which has a long-term effect on the control of food consumption and other appetitive behaviors, and carbon monoxide, which increases the risk of intrauterine growth retardation and low birth weight (Hollis & Robinson, 2022; Harvard T.H. Chan, 2022a).
MATERNAL WEIGHT
Increasing evidence implicates maternal obesity as a major determinant of health in offspring during childhood and later adult life. Children of pregnant women with obesity are at increased risk of developing obesity in childhood and as adults. Both prepregnancy obesity and maternal weight gain during pregnancy play important roles in determining birth weight with increased risk for a newborn who is large for gestational age.
Maternal obesity may affect long-term offspring outcomes as a result of epigenetic changes induced by fetal exposure to increased levels of glucose, insulin, lipids, and inflammatory cytokines during development. These in utero effects may cause permanent or transient changes in metabolic programming, leading to adverse health outcomes in adult life (Ramsey & Schenken, 2021).
MATERNAL BLOOD SUGAR LEVELS
One mechanism to explain the link between maternal obesity and excess fetal weight gain may be that the fetus is overnourished due to exposure to high maternal plasma concentrations of glucose, free fatty acids, and amino acids. In postnatal life there may be permanent consequences of prenatal overnutrition, which may include effects on control of appetite, neuroendocrine function, and energy metabolism, resulting in lifelong consequences for the child’s ability to regulate energy balance and body weight (Hollis & Robinson, 2022).
Gestational diabetes mellitus (GDM) subjects the fetus to periods of high blood glucose and elevated insulin, which can lead to increased body fat. Boys exposed to GDM have a more unfavorable fat distribution than those not exposed; however, no difference has been found in girls. Exposure to gestational diabetes, in particular prior to 26 weeks’ gestation, has been found to be associated with increased energy intake, increased reaction to food cues, increased waist-to-hip ratio, and as adults, metabolic syndrome (Lou et al., 2021).
Postnatal Factors
There are three postnatal factors during infancy that influence weight in later life. These include how rapidly an infant gains weight, how long an infant is breastfed, and how much an infant sleeps.
INFANT RAPID WEIGHT GAIN
Children who experience rapid weight gain postnatally have been found to have a significantly higher risk of being overweight or obese at preschool and school age, regardless of its occurrence at any time interval before the age of 2 years (Li et al., 2020).
BREASTFEEDING
Breastfeeding initiation and duration may influence obesity in later life. In two meta-analyses of breastfeeding vs. bottle feeding, breastfeeding was associated with a 13% and a 22% reduced risk of obesity in later life. Another analysis of 17 studies of breastfeeding duration found that each additional month that infants were breastfed was associated with a 4% lower risk of obesity later in life. However, it is not clear that breastfeeding itself actually prevents obesity, as both breastfeeding and obesity may be influenced by similar socioeconomic and cultural factors (Harvard T.H. Chan, 2022a).
MODERN HISTORY OF BREASTFEEDING
Historically, breastfeeding in America has been heavily influenced by culture and the manufacture of formulas, which began at the turn of the century. Manufacturers promoted baby formulas and suggested that their use was an improved, modern way to feed babies. This commercialization and also the medicalization of infant care established an environment that encouraged bottle feeding as the best and most necessary way to feed infants. By 1950 more than half of the babies in the United States were fed some form of baby formula (Apple, 1987).
By the 1970s, however, years of research showed that breast milk was best, and the pendulum began to swing back toward breastfeeding. The American Academy of Pediatrics now recommends that infants be exclusively breastfed for about the first six months, with continued breastfeeding alongside the introduction of complementary foods for at least one year. Among infants born in 2017, 84% were breastfed, 58% were breastfed at six months, and 35% were still being breastfed at one year (CDC, 2021d).
INFANT SLEEP DURATION
It has been found that infants who slept fewer than 12 hours a day had double the odds of being overweight by the age of 3 years, compared with infants who slept more than 12 hours a day. Factors that were associated with shorter sleep duration included maternal depression during pregnancy, early introduction of solid foods (before four months), and television viewing (Harvard T.H. Chan, 2022b).
Ultraprocessed Foods
The increase in obesity around the world appears to be linked to changes in the global food system, leading to replacement of traditional meals with those that are made up of ultraprocessed foods. Scientific studies published between 2010 and 2020 and carried out in the United States, Canada, United Kingdom, France, Spain, Australia, Japan, Taiwan, Chile, Colombia, Argentina, Mexico, Brazil, and other countries consistently show that higher consumption of ultraprocessed food is associated with a reduction in diet quality and with an increased incidence of obesity and other chronic noncommunicable conditions and diseases such as diabetes, hypertension, heart disease, some cancers, and earlier mortality (Monteiro & Jamie, 2020).
Unprocessed or minimally processed foods represent a small proportion of, or are even absent from, the list of ingredients of ultraprocessed foods. Ultraprocessed foods are those that include formulations of ingredients typically created by a series of industrial techniques and processes. Ultraprocessed foods are made possible by the use of many types of additives, including those that imitate or enhance palatability. They typically contain little or no intact foods and are ready to drink, eat, or heat up. These foods have a poor nutrient profile, including high salt content or added sugar; unhealthy fats; and low dietary fiber, micronutrients, and phytochemicals. The processing itself makes these foods nutritionally unbalanced.
By design, these products are highly palatable, cheap, ubiquitous, and contain preservatives that offer a long shelf life. The convenience and attractiveness of these foods and their aggressive marketing are two reasons why they now amount to more than half of the total dietary energy consumed in high-income countries. In the United States, 67% of calories consumed by children and adolescents in 2018 came from ultraprocessed foods. At the same time, the consumption of unprocessed or minimally processed foods had decreased to 28% (Wang et al., 2021).
The NOVA classification system developed by researchers at the University of Sao Paulo, Brazil, places all foods into four groups:
- Group 1: Unprocessed or minimally processed foods (e.g., fresh or frozen fruits and vegetables)
- Group 2: Processed culinary ingredients (e.g., salt, sugar, molasses, syrup, honey, starch)
- Group 3: Processed foods (e.g., breakfast cereals, cheese, bread, meat products)
- Group 4: Ultraprocessed food and drink products:
- Sodas and sweetened drinks, including energy drinks
- Sweet or savory packaged snacks
- Confectionery and industrialized desserts
- Mass-produced packaged breads and buns
- Cookies, pastries, cakes, and cake mixes
- Margarine and other spreads
- Sweetened breakfast cereal
- Fruit yogurt
- Preprepared meat, cheese, pasta, and pizza dishes
- Packaged meatballs
- Poultry and fish nuggets and other reconstituted meat products
- Meat products that contain preservatives other than salt
- Frozen or shelf-stable instant meals
- Instant noodles and instant or canned soups
- Baby formula and other baby food products
- Weight-loss products such as meal replacement shakes and powders
Additionally, there are many other ready-to-consume formulations of several different ingredients. Besides large amounts of salt, sugar, oils, and fats, these foods include substances not commonly used in food preparation, such as modified starches, hydrogenated oils, protein isolates, and classes of additives whose purpose is to imitate sensorial qualities of unprocessed or minimally processed foods and their cooking preparations or to disguise undesirable qualities of the final product (Wang et al., 2021; Monteiro et al., 2019).
MAKEUP OF HOMEMADE VS. ULTRAPROCESSED FRENCH FRIES
Homemade french fries contain three ingredients: potatoes, oil, and salt. The following is a list of ingredients that make up the ultraprocessed french fries from McDonald’s:
- Potatoes
- Vegetable oil (canola oil, corn oil, soybean oil, hydrogenated soybean oil)
- Dextrose
- Sodium acid pyrophosphate (to maintain color)
- Salt
- Natural beef flavor made from:
- Beef amino acids
- Hydrolyzed wheat (emulsifier)
- Hydrolyzed milk (milk-based formula in which milk proteins are broken down into smaller pieces)
- Starch hydrolysate (a mixture of sugar alcohols, a type of sugar substitute)
- Citric acid
The effects of ultraprocessed foods on health are likely due to the synergistic effects of many compounds and components in these types of foods.
The ultraprocessed foods in the Western diet have presented a major challenge to gut microbiota, negatively impacting human digestive physiology, which may result in pathogenic effects on the immune system, which is mediated by gut microbiota. Common food additives such as salt, emulsifiers, stabilizers, bulking agents, sweeteners, and food coloring may disrupt gut bacteria. Metal and compounds found in the food packaging may trigger intestinal permeability and increase inflammatory markers (Olmo et al., 2021).
ULTRAPROCESSED FOOD AND NEUROLOGIC AFFECTS
The changes in gut microbiota as a result of high consumption of ultraprocessed foods can lead to inflammation and oxidative changes, which have been found to be tightly correlated with cognitive impairments and neurogenerative diseases. Systemic and metabolic inflammation leads to increased blood-brain barrier permeability, which then leads to neuroinflammation and neurodegeneration. Considerable evidence has shown that the ultraprocessed foods in the Western diet can enhance or induce Alzheimer’s disease’s pathological features in the brain and can impair cognition, learning, and memory both in rodents and humans (Więckowska-Gracek et al., 2021).
Addictive Potential of Processed Foods
One contributing factor to overweight and obesity is that certain foods have been shown to be capable of triggering an addictive response in some individuals. Human bodies are biologically “wired” to seek out high-fat, high-salt, and high-sugar foods. Sugar, salt, and fat have been so important in human evolution that the brain responds to these nutrients much like it does to other additive substances by “rewarding” individuals with the release of “feel-good” chemical messengers such as dopamine and an increased desire for more. In combination, these nutrients act synergistically and are far more addictive than any one alone.
For those people who are more predisposed to addiction, these foods can overpower other signals from the brain that tell them they are satiated, resulting in a cycle of overeating. And just as with other addictive substances, over time a tolerance to these foods may develop and more must be eaten to provide the same level of pleasure.
Others have proposed that people experience a “process addiction” rather than a true addiction to food. People become dependent on the process that happens—the good, soothing feelings and pleasure that occur with eating—rather than to the food itself.
The foods found to be most likely to lead to compulsive overeating have one thing in common: a strong combination of carbohydrates, salt, and fat. This combination is difficult to find in nature, but the processing of foods can mix ingredients and chemically exaggerate flavors to create tastes that are very agreeable and hard to resist (Cleveland Clinic, 2021).
SALT
Throughout evolutionary history, salt has been a vital necessity for survival, and it has been a very rare resource. As a consequence, humans have evolved neuronal pathways for a habitual salt craving, which cannot be controlled. The importance of salt to overall health may explain why salty foods are so tasty and “you can’t eat just one.” Sodium appetite is an important instinctive behavior with high survival value, as there are many physiologic and cellular functions that depend on salt.
Neuronal mechanisms help drive the lust for salt. Neurons in the central amygdala become highly active when salt is being consumed. This area of the brain controls many innate and conditioned behaviors, including appetite-related and feeding behaviors. When salt is ingested, the central amygdala is activated, and the endogenous mu-opioid receptor signaling within this region promotes sodium intake. The reward results in craving more salt, resulting in the response of overeating (Research Features, 2021).
Monosodium glutamate (MSG) is a form of concentrated salt added to foods to enhance flavor; it contains about one third the sodium of table salt. This salt product may interfere with appetite suppression and cause hunger even after eating a large amount of food (Cardiff, 2021).
INDUSTRIAL SEED OILS
Traditional fats are olive oil, coconut oil, butter, ghee, and lard. Industrial seed oils are highly processed oils extracted from soybeans, corn, rapeseed (source of canola oil), cottonseed, and safflower seed. Industrial seed oils were originally used in the soapmaking process. It was discovered that these oils could be chemically altered by hydrogenation to turn into a solid cooking fat that resembled lard; this product was named shortening.
These industrial seed oils are used extensively in the making of processed foods; and foods rich in fat are hyperpalatable, which can lead to consumption in excess amounts.
The 11 criteria for substance use disorders as described in the DSM-5 can be applied to individuals with addiction to lipid-dense foods (especially trans and saturated fats). The interactions between fatty acids and specific receptors in taste bud cells elicit physiologic changes that are implicated in dietary fat preference through activation of the tongue-brain-gut axis (Sarkar et al., 2019).
The opioid and endocannabinoid systems play a crucial role in this process. The opioid system is connected to hedonic food properties and modulates the release of dopamine when food is consumed. The endocannabinoid system is more closely connected to homeostatic control of intake and positive feedback to the consumption of high-fat foods rather than carbohydrates or sugar (Blanco-Gandia et al., 2020).
SUCROSE AND HIGH-FRUCTOSE CORN SYRUP
Some 200 years ago, Americans ate about two pounds of sugar per year. Today, however, they consume on average more than 120 pounds per year. Some of this increase is thought to have occurred in the early 1990s when food makers began adding more sugar to improve their products’ flavor when simultaneously removing fat in order to label these products “fat free.” Since then, it has been found that added sugars in our food, mainly in the form of fructose, have contributed to high levels of obesity and chronic diseases such as diabetes and liver disease (Pfizer, 2022).
Sucrose, broadly known as granulated sugar, comes from cane or beets. It is made up of two molecules: glucose and fructose. The glucose molecule provides fuel and suppresses the hunger hormone ghrelin, which then stimulates leptin production. Leptin then tells the brain that we are full and decreases appetite. Fructose is a sugar found naturally in fruit, honey, and fruit juice. Unlike glucose, fructose does not trigger satiating hormones. While glucose is metabolized in every cell in the body, the fructose molecule is only metabolized by the liver.
Fructose corn syrup adds unnatural amounts of fructose to the diet, which the human body has not evolved to handle well. Fructose does not stimulate insulin secretion or enhance leptin production like glucose does. It also converts to fat more readily than any other sugars. Fructose has no effect on the hunger hormone ghrelin and can interfere with leptin levels, leading to overeating. High-fructose corn syrup (HFCS) is a highly processed syrup sweetener derived from cornstarch. The syrup is widely added to many kinds of processed foods, including soft drinks, breads and cereals, processed meats, dairy products, condiments and sauces, processed fruits and vegetables, crackers, candy, and jam and jellies.
HFCS increases appetite and contributes to diabetes, inflammation, and obesity. When sugar and HFCS are consumed to a specific threshold, the brain’s neurochemistry is altered. HFCS affects central appetite regulation by altering specific components of the endocannabinoid system. Sugar and HFCS have been implicated in food addiction because their intense sweetness elicits a dopamine rush in the brain that triggers cravings for more. Twenty minutes after drinking a soda containing HFCS, blood sugar spikes, causing an insulin burst. The liver responds by converting any sugar into fat. Forty-five minutes later, the body increases dopamine production, stimulating the pleasure centers of the brain. It has been demonstrated that the effects of sugar addiction, withdrawal, and relapse are similar to those of drugs of abuse (Mohiuddin, 2020).
CASEIN
Casein is a protein naturally found in milk and used in producing fast-food items, such as french fries, buns, milkshakes, creamy salad dressings, whipped toppings, and more. Over the last 30 years, casein has been used in foods to enhance physical properties such as whipping and thickening and to enhance nutritional value.
Casein in often called the “nicotine of fast food.” It naturally occurs in milk, but in fast food, it is transformed to a refined and concentrated form created by adding calcium hydrogen phosphate to concentrated milk solids. Casein is the addictive property in cheese.
Casein contains opiates, and as it is digested, it breaks apart to release tiny opiate molecules called casomorphins. One of these compounds has about one tenth the opiate strength of morphine. Casomorphins can attach to dopamine receptors, causing a dopamine “hit” of pleasure or reward. The addicting power of cheese, for example, may be caused by adding calcium hydrogen phosphate to remove water, lactose, and whey products, which then concentrates the casein. Because of the reward received from eating products containing casein, overconsumption is encouraged (Clark, 2021; Arakelyan, 2020).
PROCESSED FOODS CONTAINING CAFFEINE
The combination of sugar and caffeine in beverages raises the risk of being overweight. Children who drink one or more 12-ounce sweetened soft drink daily have a 60% higher chance of becoming obese. Young people consume the largest quantities of caffeinated sugar-sweetened beverages and have experienced the greatest relative gains in obesity. Evidence of the addictive properties of both caffeine and sugar have been documented, and abruptly stopping caffeine may cause withdrawal symptoms in those who consume a lot of it. A single energy drink may contain as much as 500 mg of caffeine, which is the same amount as in about 14 cans of soda.
Caffeine is also found in chocolate, coffee ice cream or frozen yogurt, and iced tea, which can contain as much sugar and caffeine as soda (Falbe et al., 2019; Morin, 2022).
Medications
Certain medications can cause individuals to gain weight. Described below are some medications that can affect the body’s metabolism and slow calorie burning, stimulate appetite, cause water retention, or alter how the body stores and absorbs sugars and other nutrients.
- Drugs for diabetes (e.g., insulin, thiazolidinediones, sulfonylureas)
- Antipsychotic drugs (e.g., haloperidol, clozapine, risperidone, olanzapine, quetiapine, lithium)
- Antidepressant drugs (e.g., amitriptyline, imipramine, paroxetine, escitalopram, citalopram, mirtazapine, sertraline)
- Drugs for epilepsy (e.g., valproate, divalproex, carbamazepine, gabapentin)
- Steroid hormone drugs (e.g., prednisone, birth control pills)
- Blood pressure–reducing drugs (e.g., beta-blockers)
It is important to note that not all medicines of these types cause weight gain. For example, metformin for diabetes and topiramate for seizures and migraines may cause weight loss instead of weight gain (URMC, 2022).
Physical Activity
Physical activity refers to any body movement that burns calories, whether for play or for work. Exercise, a subcategory of physical activity, refers to planned, structured, and repetitive activities with the goal of improving physical fitness and health.
Regular physical activity is a vital necessity for good health. Physical activity helps to reduce blood pressure; reduce risks for type 2 diabetes, heart attack, and stroke; relieve symptoms of depression and anxiety; and maintain a healthy weight.
Research has indicated that physical activity prevents obesity in the following ways:
- By increasing total energy expenditure, decreasing fat around the waist as well as total body fat, and slowing abdominal obesity development
- By building body mass through muscle-strengthening activities and thus increasing the energy the body burns even at rest
- By reducing depression and anxiety, which may boost motivation to maintain an exercise regimen
(Harvard T.H. Chan, 2022c)
The “energy out” side of the energy balance equation has tilted severely toward weight gain. The more active people are, the more likely they are to maintain a steady weight. The more sedentary, the more they are likely to gain weight over time (PCSFN, 2021).
Globally, people are less active than they were in the past due to economic growth, technological advancements, and social changes. In just a generation, the number of students who walk and bike to school each day has declined dramatically, while the childhood obesity rate and physical inactivity have climbed.
The good news is that the number of Americans who engaged in physical activity rose steadily from 2010 to 2019, and the number of fitness centers and health clubs also experienced a near continual increase between 2009 and 2019. Statistics also indicate an increase in outdoor activities since 2008, with the most popular being running, jogging, and trail running (Lange, 2021).
Despite this increase in physical activity, however, recent statistics show that:
- Only 1 in 3 children are physically active every day.
- Less than 5% of adults participate in 30 minutes of physical activity each day.
- Only 35%–44% of adults 75 years or older are physically active, and only 28%º–34% of adults ages 65–74 are physically active.
- More than 80% of adults do not meet the guidelines for both aerobic and muscle-strengthening activity.
- More than 80% of adolescents do not get enough aerobic physical activity to meet the guidelines for youth.
- Children now spend more than seven and a half hours a day in front of a screen (e.g., TV, video games, computer).
- The average amount of time spent on sports, exercise, and recreation in the United States is 20 minutes per day.
(RXResource, 2022; Lange, 2021)
EFFECT OF COVID-19 PANDEMIC ON PHYSICAL ACTIVITY
The COVID-19 pandemic resulted in a significantly reduced level of physical activity during the social-distancing period. Prior to the pandemic, 69% of a select group of volunteers were classified as very active, and during the social-distancing period, this percentage dropped to 39% (Pucinelli et al., 2021).
Obesogenic Environment
An obesogenic environment is the sum of influences that the surroundings, opportunities, or conditions of life have on promoting obesity in individuals and populations. This includes the physical surroundings as well as the conditions in which an individual lives or works. These factors influence the development of a person or a group of persons and how they feel or function (Kaczynski et al., 2020).
BUILT ENVIRONMENT
The built environment underwent changes beginning early in the 20th century when motor vehicles began to take over the streets. As a result, many aspects of today’s built environment—housing, roads, walkways, population density, transportation, shops, parks, and public spaces—do not encourage walking, biking, or other physical activities. Many communities are built in ways that make it difficult or unsafe to be physically active. It may be hard for families to get to parks and recreation centers, and public transportation may not be available.
Zoning laws have separated residential, commercial, and industrial uses and have increased the distances between homes, jobs, and shops. Many towns and cities have become spread out along roads, making it necessary for people to drive just about everywhere. It has been hypothesized that this “urban sprawl” and lack of mixed land use are associated with overweight or obesity more than any other physical environmental factor (Lam et al., 2021).
Recreational and transport physical activity are driven by the features of the built environment. Physical activity is promoted by the built environment through walkable neighborhoods, presence of sidewalks, walking paths and bike paths, and recreational and sports infrastructure, including parks, pools, playgrounds, and sport clubs.
ENCOURAGING PHYSICAL ACTIVITY
Communities around the country are making efforts to encourage walking, biking, and other forms of physical activity.
- After the city installed a new bike lane in New Orleans, the number of cyclists increased by 22%.
- People who used outdoor fitness equipment in Los Angeles parks exercised 46% more frequently than those who did not.
- In five states, walking and biking to school increased by 37% after sidewalks and crosswalks were improved.
- In Houston, the number of children walking or biking to school increased by 125% after schools began participating in a “walking school bus” program, which involves a group of children walking to school together with one or more adults.
(Physiopedia, 2022)
“SCREEN TIME”
Screens are ubiquitous in today’s environment, and almost everyone’s daily routine includes them, including children. Children ages 8–10 spend an average of six hours per day in front of a screen, kids ages 11–14 spend an average of nine hours per day in front of a screen, and youth ages 15–18 spend an average of seven and a half hours per day in front of a screen (OSF HealthCare, 2020). It has been shown that screen time greater than two hours per day is associated with increased rates of obesity and that teens who spend five hours or more watching TV are five times more likely to become overweight. This increased risk for obesity occurs because:
- Screen time is a sedentary activity (i.e., time spent not being physically active).
- Screen time, particularly within 4 hours of bedtime, leads to poor sleep.
- TV commercials and other screen ads can lead to unhealthy food choices.
- Screen time is associated with “mindless” eating behaviors and intake of sugar-sweetened beverages.
More than two hours of daily screen time is also associated with decreased executive function, decreased inhibition, increased impulsivity and inattention, cognitive changes associated with ADHD, binge eating, and loss of eating behavior control (Bleistein, 2022; NIH, 2021b).
FOOD AND NUTRITION ENVIRONMENT
What people choose to eat plays a large role in determining risk of overweight or obesity. People’s choices are shaped by the world in which they live. In the United States, physical and social surroundings influence what one eats and can make it difficult to choose healthy over unhealthy foods. The food and nutrition environment includes all the factors involved in the ability to access foods: the availability of foods, culture and ethnicity, parenting, marketing, and other significant factors.
Food Availability and Access
Availability and access to foods that support healthy eating patterns is a major issue in the domain of neighborhood/built environment, and studies show there is a relationship between access to food and rates of obesity. People living in neighborhoods with fewer fresh produce sources and plentiful fast-food restaurants and convenience stores are at a higher risk for obesity compared to at-risk rates found in areas with increased access and higher density of full-service restaurants and grocery stores.
In addition, the food environment surrounding schools has been found to impact children and adolescents. Students whose schools were within a half mile of a fast-food restaurant were more likely to be overweight or obese than students whose schools were farther away from such restaurants.
Transportation and distance impact low-income and rural communities. Individuals without a vehicle or access to convenient public transportation, or who do not have food venues with healthy choices within walking distance, have limited access to foods that support healthy eating patterns.
Studies have provided evidence that neighborhoods with a high proportion of low-income or minority residents have fewer supermarkets but more convenience stores relative to more advantaged areas. People in predominantly Black low-income neighborhoods live an average of 1.1 miles farther from the closest supermarket than people living in predominantly White low-income neighborhoods.
Another barrier to accessibility of healthy food choices is the “food desert,” where food sources are lacking or limited. These often occur in low-income areas that are more likely to have a high share of convenience stores and small food markets, which tend to carry foods of lower nutritional quality compared to large chain supermarkets.
Affordability also influences access to nutritious foods. Research has shown that low-income groups tend to rely on foods that are less expensive and convenient to access, but are low in nutrient density. In those areas without supermarkets, people face higher prices for many healthy foods because small stores typically charge more for foods such as fresh produce. Conversely, studies have shown that price reductions for healthier foods contribute to increased purchasing of these foods (ODPHP, 2022).
An estimated 1 in 8 Americans lack access to enough food. Children from food-insecure households have been found to have higher BMI and waist circumference and greater odds of being classified as overweight or obese. They consume more sugar from sugar-sweetened beverages and less frequently eat breakfast and dinner with family compared to children from food-secure households.
Those in food-insecure homes obtain a higher portion of their energy needs from fat and carbohydrates; eat less protein and fewer fruits and vegetables; and eat irregular meals or skip breakfast. Girls in food insecure homes have a greater risk for weight gain and overweight than boys. Evidence supports a link between food insecurity, stress, and compromised mental health among females in high-income countries (Au et al., 2019).
Culture and Ethnicity
Culture affects the circumstances in which we eat, the types of food we eat, whom we eat with, the times of the day that we eat, and the quantities we eat. Food is culture and presents an everyday actualization of one’s ethnic identity. Food contains childhood memories, religious meaning, and connections to one’s origins.
Ethnic minority groups living in developed countries have higher rates of obesity. In the United States, they initially have lower BMI than U.S.-born individuals. However, this advantage erodes over time as they become acculturated, adhering less to traditional diets and engaging in less physical activity.
Social isolation, depression, and stress related to immigration influence the development of obesity. Among some populations, eating is also a culturally sanctioned form of stress reduction, leading to overconsumption.
Obesity disproportionately affects ethnic minority children. Research has found acculturation to be linked with rapid weight gain in infancy due to more acculturated mothers formula-feeding their infants rather than breastfeeding them. And among many cultures, there is the cultural belief that a chubby baby is proof of good parenting.
Parental feeding practices that may contribute to obesity include urging children to eat until they are “stuffed” or pressuring children to “clean” their plates. Conversely, some parents closely monitor their children’s food intake, restrict unhealthy food and snacks, and require scheduled meal times, which are protective factors against obesity.
Another protective influence commonly found among some cultures and ethnic groups is the theme of family, specifically family meals. Having such meals as infrequently as one to two times a week has been found to be protective against overweight and obesity. Another protective influence is parents who express disappointment and frustration that their children prefer processed, fast food, and continue cooking traditional foods despite their children’s preferences.
According to some research, the most prominent belief about physical activity across ethnic groups is that it should simply be a part of daily life as it was in their country of origin. This research found that most ethnic minority families valued sedentary activities, especially watching television. Migrant farmworkers often believed that too much physical activity can be unhealthy. Every ethnic group studied mentioned weather as a barrier to physical activity; it was either too hot or too cold (Gale, 2019; Chatham & Mixer, 2019).
Parenting Style
Parental feeding style affects children’s eating behaviors. Three negative feeding styles have been found to be linked to overweight and obesity. These include:
- Authoritarian style makes high demands and shows low responsiveness to the child’s wishes. It involves low support for child autonomy in eating and shows little trust in a child’s hunger/satiety signs. Example: A child cleans her plate even though she is full in order to please her parents. Effect: Ignoring a child’s appetite may lead to loss of ability to regulate internal hunger and fullness cues.
- Permissive/indulgent style involves making few demands, having very few rules, catering to the child’s food preferences, and providing low control. This style is often linked with high intake of sweets and high-fat foods. Example: A child has eaten a cookie for dessert and demands more. The parent’s response is, “Okay, you can have as many as you want.” Rewarding is another example of an indulgent style. Example: A parent tells a child at the dinner table, “If you eat all your broccoli, I’ll take you out for ice cream.” Effect: The child tends to become out of touch with what and how much to eat.
- Uninvolved/neglectful style includes low demands and low responsiveness to the child, lack of support, and lack of structure and control. Parents show low sensitivity to their child’s needs and fail to plan and prepare food in a regular, reliable manner, considering food and feeding to be a low priority. Example: A child is hungry, but there is no response from the parent to provide a regular meal because they consider food and feeding to be a low priority, they have not gone shopping, and therefore no one prepares a meal. Effect: The child becomes preoccupied with food, worried, and anxious, causing over- or under-eating.
A positive parental feeding style is authoritative, meaning that it makes high demands but is also highly responsive to the child. This style of feeding includes:
- Age-appropriate monitoring of eating and food purchasing behaviors
- Appropriate portion sizing
- Limiting snacking
- Allowing the child to contribute ideas for meals and snacks and showing respect for the child’s food choices
- Modeling healthy eating behaviors
- Establishing food routines, an appropriate feeding environment, and regular family meals
- Avoiding the purchase of unhealthy foods and dining at unhealthy restaurants
(Chen, 2020; Alahmadi, 2019)
WORK ENVIRONMENT AND OCCUPATION
The type, hours, and place of work have been recognized as sources of adverse environmental exposures that can lead to overweight and obesity.
- Long working hours are associated with risk of a shift from a normal weight to overweight but not from overweight to obese. Mechanisms may include lack of exercise, unhealthy diet, and extended periods of sitting. People working long hours may not have the resources, time, or remaining energy to engage in a healthy lifestyle (Virtanen et al., 2020).
- Rotating shift work has been identified as a risk factor for overweight or obesity. Shift workers have 1.5 times higher odds of being overweight/obese. The more years of exposure increases the risk, with the strongest relationship among those working shifts for more than 20 years (Hulsegge et al., 2020).
- Night shift work influences BMI and the risk of obesity due to changes in metabolism, insulin sensitivity, and appetite, and a reduction in energy for physical activity secondary to disrupted or insufficient sleep. An unhealthy diet and irregular eating patterns are also linked to weight gain and risk of obesity (Myers et al., 2021).
- Blue-collar workers (which may include machine operators, construction workers, public safety workers, and sales/office workers) have a higher risk of obesity. This may be due to a variety of mechanisms, such as low access to and participation in wellness programs; exposure to environmental hazards; and adverse working conditions, such as a “fire station eating culture,” answering night calls and related sleep interruption, sedentary work, and stressful supervisor leadership (Myers et al., 2021).
- Stress among those with low control and low autonomy in their work can relate to anxiety in relation to job insecurity. This stress often leads to making “comfort food” choices and could affect behaviors such as alcohol consumption and sedentary leisure activities. It also may result in modification of endocrine factors related to weight gain (Elhussiney & Mahfouz, 2020).
FOOD MARKETING
Advertisements for unhealthy foods are everywhere, and marketing to young people to “hook” them on food manufacturers’ products presents a very profitable investment. Food marketing is highly effective at stimulating and reinforcing food consumption, particularly for energy-dense foods. To date, food advertising almost exclusively promotes ultraprocessed food and beverage products high in fats, sugars, and sodium.
Studies have found that one effect of unhealthy food marketing is increased saliva secretion and uptake of appetite-stimulating hormones such as ghrelin and insulin. This leads to increased appetite and increased food intake that then reinforces reactivity to food cues. This reaction to food cues is known as the incentive-sensitization process (Folkvord & Hermans, 2020).
Children are constantly exposed to advertisements (just as are adults), coming into contact with ads in many different ways every day through television and product placement in movies, websites, games, at supermarkets, and even in schools.
A study of the most popular YouTube videos for children and the advertisements shown before and during those videos found that 72% of ads were for food and beverages, with over half of those for foods eaten for fun rather than for nutritional value. Another study of children 4 to 6 years of age found that they believed a food product packaged with a cartoon character or collectible toy tasted better than the same food in a package without the character or toy.
Researchers have calculated that the average child ages 5 to 8, who watches about 80 minutes of television each day, is exposed to at least 827 advertisements on television each year. Only 16 countries have regulations on food marketing to children, and the United States is not one of them (Barber, 2020; OEH, 2021).
SLEEP DEPRIVATION
Sleep deprivation or deficiency is a state in which the person cannot make up lost hours of sleep, which increases the risk of obesity and other chronic health conditions. A nurses’ health study found an association between those who slept the least (5 hours or less a night) and those having the highest BMI and greatest weight gain. One reason may be a disruption in appetite and satiety hormones. With lack of sleep, ghrelin levels rise, while leptin levels drop. This can result in a higher calorie consumption and trigger the “reward” area in the brain to increase a preference for foods high in fat and carbohydrates.
Contrary to expectations, however, due to fatigue, sleep deprivation does not result in any increases in physical activity. Less physical activity combined with increased calorie intake increases obesity risk. Other effects include increased fat storage in the abdominal area, higher body mass index, poorer-quality diet, and decreased insulin sensitivity (Harvard T.H. Chan, 2022c).
Short sleep duration is a risk factor or marker of the development of obesity in infants, children, and adolescents. National Sleep Foundation guidelines are given in the table below.
| Age | Duration (hours) |
|---|---|
| (NSF, 2020a) | |
| Newborns (0–3 months) | 14–17 |
| Infants (4–11 months) | 12–16 (including naps) |
| Toddlers (1–2 years) | 11–14 |
| Preschool-aged children (3–5 years) | 10–13 |
| School-aged children (6–13 years) | 9–11 |
| Teenagers (14–17 years) | 8–10 |
| Adults (18–64 years) | 7–9 |
| Older adults (65 and over) | 7–8 |
CIRCADIAN MISALIGNMENT
The circadian rhythm is the natural cycle of physical, mental, and behavior changes a body goes through over a 24-hour period of time. These rhythms are mostly the result of exposure to light and darkness, and they affect sleep, body temperature, hormone production, appetite, and other body functions. The circadian cycle can be disrupted by such things as:
- Shift work
- Inconsistent sleep and wake times
- Lack of bedtime routine
- Insufficient light exposure during the day and bright light exposure at night (blue light having the strongest impact)
- Drinking caffeine or alcohol too close to bedtime
- Using smartphones/computers late at night
- Jet lag
- Some medications (e.g., corticosteroids, beta blockers)
Studies show that mistimed eating, such as eating at night when the body should be sleeping, can also alter the circadian rhythm of various tissues. Metabolically active, insulin-sensitive tissues, such as the liver and adipose tissue, are particularly affected. Eating out of sync with the internal clock increases the risk of obesity, metabolic syndrome, and type 2 diabetes (Tuvia et al., 2021; NIH, 2021c; NSF, 2020b).
COMORBITIES AND CONSEQUENCES OF OBESITY
Adult obesity is associated with a notable reduction in life expectancy and an increased rate of death from all causes. In addition to increased mortality, obesity and increased central adiposity are associated with increased morbidity. Obesity has now surpassed smoking as the number one cause of preventable disease and disability, and studies have found that the risk of developing a chronic disease increases with increasing body mass index (Perrault & Laferrère, 2020).
In Adults
DISEASES AND HEALTH CONDITIONS
People with obesity are at increased risk for many serious diseases and health conditions, including:
Metabolic
- Type 2 diabetes mellitus
- Insulin resistance with hyperinsulinemia
- Dyslipidemia
Cardiovascular
- Essential hypertension
- Coronary artery disease
- Left ventricular hypertrophy
- Cor pulmonale (right-sided heart failure)
- Myocardial steatosis (excessive lipid accumulation in the myocardium)
- Atrial fibrillation (significantly greater risk in those with metabolic syndrome)
- Accelerated atherosclerosis
- Pulmonary hypertension of obesity
- Deep vein thrombosis and pulmonary embolism
Gastrointestinal
- Gallbladder disease (cholecystitis and cholelithiasis)
- Non-alcoholic steatohepatitis (NASH) (the severe form of nonalcoholic fatty liver disease)
- Gastroesophageal reflux disease (GERD), erosive esophagitis, esophageal adenocarcinoma, and gastric cancer
Respiratory
- Obstructive sleep apnea
- Obesity hypoventilation syndrome (Pickwickian syndrome) caused by a reduced capacity of the respiratory system due to obesity
- Increased incidence of bronchial asthma (risk may be greater for nonallergic rather than allergic asthma)
Infection
- Increased susceptibility to infections, including postoperative nosocomial, respiratory, skin, and soft tissue infections
Central nervous system
- Stroke
- Idiopathic intracranial hypertension, which produces papilledema and vision loss
- Meralgia paresthetica (tingling, numbness, and burning pain in the outer part of the thigh caused by entrapment of the lateral femoral cutaneous nerve [LFCN])
Musculoskeletal
- Osteoarthrosis (noninflammatory joint disease)
- Osteoarthritis (inflammatory joint disease)
- Coxa vera (a deformity of the hip)
- Chronic lumbago (pain in the muscles and joints of the lower back)
- Gout related to the influence of BMI on hyperuricemia
Reproductive
- Anovulation and irregular menses
- Infertility
- Increased risk for maternal and perinatal complication
- Disorders of sexual arousal and orgasm in females
- Erectile dysfunction due to hormonal imbalance, endothelial dysfunction, insulin resistance, physical activity
- Hyperandrogenism and polycystic ovaries in women
- Hypogonadotropic hypogonadism in men
Genitourinary
- Glomerulosclerosis and obesity-related glomerulopathy
- Chronic kidney disease related to decreased filtration rate and albuminuria
- Nephrolithiasis (kidney stones)
- Stress incontinence in females
Cutaneous
- Intertrigo (bacterial and/or fungal inflammation caused by skin-to-skin friction)
- Acanthosis nigricans around neck, axilla, knuckles, and extensor surfaces related to hyperinsulinemia
- Hirsutism in females related to increased production of testosterone associated with visceral obesity
- Skin infections, e.g., cellulitis and carbuncles
- Striae distensae (stretch marks)
Malignancies
- Some cancers (endometrial, prostate, breast, colon, gallbladder), which may be due to alterations in sex hormone metabolism, insulin and insulin-like growth factor levels, and adipokine pathways
Extremities
- Venous varicosities
- Lower extremity venous and/or lymphatic edema
Psychological
- Mental illness such as chronic depression, anxiety, and other mental disorders
- Social stigmatization
- Low quality of life
Miscellaneous
- Reduced mobility
- Difficulty maintaining personal hygiene
(Hamdy, 2022; CDC, 2021e; Perreault & Laferrère, 2020; Brennan, 2021b)
COGNITIVE EFFECTS
Scientists have found that increased BMI, waist-hip ratio, and waist size are associated with lower cerebral blood flow, and that a 1 cm increase in waist size produces the same reduction in blood flow as one year of aging.
Obesity promotes the development of vascular cognitive impairment and also increases the incidence of Alzheimer’s disease. Studies indicate that aging and obesity exert synergistic negative effects on cognition, and that early midlife obesity is associated with impaired memory and executive function later in life (Knight et al., 2021).
Recent evidence has shown multiple underlying mechanisms for this development, including inflammation, hyperinsulinemia/insulin resistance, and disruption at the microbiota-gut-brain axis. These are seen to bring about pathophysiologic insults at the level of blood vessel endothelium, an early event in the development of cognitive impairment and dementia. Increasingly, evidence that both aging and obesity cause structural and functional impairment in the cerebral microcirculation play a role in the pathogenesis of both vascular cognitive impairment and Alzheimer’s disease (Balasubramanian et al., 2021).
The blood-brain barrier (BBB) is vital for maintenance of proper neuronal function and both aging and obesity promote BBB disruption. This disruption precedes and activates neuroinflammation and neurodegeneration, causing declines in microvascular integrity, leading to cognitive decline (Olsthoorn et al., 2021).
Both aging and obesity are also associated with altered gut microbiome, which has been linked to impaired cerebral blood flow, BBB impairment, and cognitive dysfunction. Adipose tissue dysfunction with its heightened inflammatory status also contributes significantly to systemic inflammation in obesity, playing an important role in impaired neuronal function and the pathogenesis of both vascular cognitive impairment and Alzheimer’s disease (Balasubramanian et al., 2021).
MOTOR EFFECTS
In adults, obesity contributes to bone and joint damage, which can increase the risk for accidents and personal injury. These may include:
- Osteoarthritis
- Disc herniation
- Spinal disorders
- Back pain
- Obesity-caused pseudotumor cerebre (“false brain tumor”) associated with confusion, disorientation, headache, and visual problems
(ASMBS, 2021a)
For both men and women, the risk of developing a walking disability rises with increasing weight status. Older people who are obese have an accelerated risk of developing a walking disability (GWU, 2019).
In Children and Adolescents
Obesity affects children and adolescents across all age groups, and the increasing prevalence of childhood and adolescent obesity is associated with a rise in comorbidities previously considered “adult diseases.” In the United States, close to one third of children over age 2 are overweight or obese, and for the first time since the 1900s, life expectancy for children is eroding because of obesity (Martinelli, 2022).
DISEASES AND HEALTH CONDITIONS
Endocrine
- Prediabetes (increases the risk for developing type 2 diabetes mellitus)
- Type 2 diabetes mellitus (leads to more rapid progression of diabetes-related complications in later life)
- Metabolic syndrome (a cluster of risk factors for type 2 diabetes and atherosclerosis, which includes abdominal obesity, hyperglycemia, dyslipidemia, and hypertension)
- Hyperandrogenism in females and risk for early-onset polycystic ovary syndrome characterized by hirsutism, menstrual irregularities, and dermatologic problems
- Accelerated linear growth and bone age associated with marked hyperinsulinemia
- Gynecomastia in males related to the stimulating effects of fat on estrogen production
- Early onset of sexual maturation
Cardiovascular
- Essential hypertension, best assessed using ambulatory blood pressure monitoring rather than casual office BP measurement
- Dyslipidemia, particularly in those with central fat distribution and increased adiposity, including elevated concentrations of LDL cholesterol and triglycerides and decreased concentration of HDL cholesterol
- Alterations in cardiac structure and function similar to those seen in middle-aged adults, including increased left ventricular mass, increased left ventricular and left atrial diameter, greater epicardial fat, and systolic and diastolic dysfunction
- Premature atherosclerotic cardiovascular disease with endothelial dysfunction of the blood vessels, aortic intima-media thickening, development of early aortic and coronary arterial fatty streaks and fibrous plaques, and increased arterial stiffness
Gastrointestinal
- Nonalcoholic fatty liver disease, the most common cause of liver disease in children, resulting in fatty infiltration and inflammation of the liver
- Cholelithiasis (gallstones), with obesity being the most common cause in children (greater for girls than boys) without predisposing conditions, the risk increasing with increasing BMI
Pulmonary
- Obstructive sleep apnea (complete obstruction of the upper airway during sleep and cessation of air movement despite ongoing respiratory effort)
- Obesity and alveolar hypoventilation syndrome (Pickwickian syndrome) during wakefulness, a rare but life-threatening disorder that requires prompt diagnosis and therapy
- Hypoventilation during sleep in the absence of airway obstruction, possibly due to the restrictive ventilator defect caused by abdominal distribution of fat
- Increased predisposition for respiratory infections and bronchial asthma
Orthopedic
- Slipped capital femoral epiphysis, typically occurring in early adolescence, related to increased shear forces at the capital femoral growth plate
- Idiopathic genu valgum (commonly called “knock-knees”), characterized by deviation of the knees toward the midline of the body
- Tibia varus (Blount disease), characterized by progressive bowing of the legs and tibial torsion as a result of excessive abnormal weight bearing, more commonly among individuals with darkly pigmented skin
- Fractures, since bone development is not always able to compensate for excess weight, with the resulting imbalance putting undue stress on developing bones
- Increased risk for joint damage or osteoarthritis in adulthood
Neurologic
- Idiopathic intracranial hypertension (pseudotumor cerebri), which presents with signs and symptoms of a brain tumor and can result in severe visual impairment or blindness
Dermatologic
- Intertrigo (an inflammatory rash caused by skin-to-skin friction in warm, moist areas of the body)
- Furunculosis (boils), or small abscesses involving hair follicles
- Hidradenitis suppurative, or inflammatory nodules or deep fluctuant cysts in the skin of the axillae and groin
- Acanthosis nigricans, or areas of dark velvety discoloration in body folds and creases, particularly the armpits, groin, and neck, associated with insulin resistance
- Striae distensae (stretch marks) caused by mechanical factors, possibly acting in concert with hormonal factors such as high levels of adrenocorticosteroids
(Skelton & Klish, 2021; Kansra et al., 2021)
COGNITIVE EFFECTS
Excess visceral adipose tissue can exceed metabolic dysregulation and affect cognitive function and brain health. In children with obesity, the level of intelligence can be affected. Significant impairments in cognitive functions, especially executive, attention, retention, intelligence, and cognitive flexibility, have been observed.
Overweight children have spatial cognitive task problems, with differences for motor ability and mental rotation accuracy, a function of visual representation. Adolescents who are obese have been found to have lower learning achievement compared to teens who are of normal weight. The relationship between compromised executive function and obesity may be partly explained by BMI-associated reduced cortical thickness in the prefrontal cortex of the brain (Ghosal et al., 2021; Alam et al., 2020; Ronan et al., 2019).
MOTOR EFFECTS
Childhood obesity and overweight are associated with the appearance of coordination deficit disorder and can cause impaired motor performance, altered postural control, and modification of motor coordination.
Childhood obesity can result in vitamin deficiencies, hormonal imbalances, and increased stress and tension that can affect bone growth and overall musculoskeletal health, causing deformity, pain, limited mobility, and diminished quality of life.
Obese children often have difficulties with coordination, including:
- Clumsiness
- Problems with gross motor coordination (jumping, hopping, balancing on one foot)
- Problems with visual or fine-motor coordination (e.g., writing, tying shoelaces)
These problems may impair or limit a child’s ability to exercise, potentially resulting in more weight gain (Barros et al., 2022; AAOS, 2019).
Psychological and Psychosocial Effects of Overweight and Obesity
Psychological effects refer to an individual’s thoughts, emotions, and behaviors; and psychosocial effects refer to the interactions and relationships between an individual, family, peers, and community.
Overweight and obesity psychological effects can include:
- Depression (adults have a 55% higher risk of developing depression over their lifetime)
- Anxiety
- Stress
- Eating disorders, including bulimia nervosa (BN), binge-eating disorder (BED), night-eating syndrome (NES), and anorexia nervosa (AN)
- Substance abuse
- Sleeping disorders, including insomnia and restless leg syndrome (Willis-Ekbom disease) associated with depression or anxiety
- Increased incidence of:
- Bipolar disorder
- Panic disorder
- Agoraphobia
Psychosocial issues affecting individuals with overweight/obesity include:
- Quality of life problems related to physical and occupational functioning. Persons with obesity may be unable to physically attend fun activities or events, travel, or visit with friends and family, which can result in social isolation, loneliness, and more difficulty coping with problematic situations.
- Weight bias/discrimination, one of the biggest challenges for those with overweight/obesity issues, is widespread and can lead to discriminatory behavior affecting a person’s self-esteem, schooling, employment opportunities, and the quality of healthcare they receive (see below).
- Adverse outcomes for overweight females and males in comparison to their non-overweight peers include having completed less schooling, having earned less money, and having less likelihood of getting married.
- Internalization of society’s negative views of obesity, which causes embarrassment and dissatisfaction with their appearance, and may cause anxiety over being judged for how they look.
(Vafiadis, 2021; Schwarz, 2020)
Children and adolescents experience increased risk of social isolation and poorer peer relationships, discrimination, harassment, and poorer self-esteem in comparison with their normal-weight peers. These factors can worsen the quality of life for a child or adolescent with obesity, with the potential for long-lasting ramifications, as obesity in childhood often results in obesity in adulthood.
In a recent study, children and adolescents with obesity, along with their parents and caregivers, reported decreased emotional and social quality of life compared with healthy nonoverweight children and adolescents. Those with severe obesity reported diminished quality of life similar to that reported by children and adolescents with cancer (Mazurak et al., 2021; Vafiadis, 2021).
WEIGHT BIAS AND STIGMA
Prejudice against “fat” people is one of the deepest and most widely shared prejudices the public holds. The pervasively hostile, discriminating environment that marginalized people find themselves in is a source of constant physical and psychological stress.
Stigmatization is mostly based on a misunderstanding of the complex causes of obesity, with people attributing weight gain to personal responsibility, resulting in blaming obese individuals for their condition and enabling the negative stereotyping of them as lazy and lacking in willpower (Schwarz, 2020).
Microaggressions against obese people are so pervasive and normalized that people often do not recognize them as stigmatizing. In fact, these negative attitudes are so embedded that many obese individuals are complicit in their own stigmatization, believing they deserve it or that those expressing prejudice are simply stating a fact. Studies show that obesity is generally viewed as a self-inflicted condition and is under the individual’s control.
Studies have confirmed that even at a very young age, children contribute to the stigmatization of overweight individuals. Weight stigma has been shown already to be developed in children from age 3 and becomes significantly stronger in children by age 5. These children have described overweight people as ugly, unpopular, lazy, liars, cheats, dirty, and stupid. Girls display stronger weight stigma than boys (Jenull et al., 2021; Skelton & Klish, 2021).
Weight Stigma in Education
Weight stigma in the educational environment is very common and is one of the major reasons for victimization. Weight stigma in these settings comes from different sources. Students aren’t just victimized by their peers, but their teachers (particularly, but not exclusively, physical education teachers) can be common perpetrators.
Weight stigma can prevent students from moving into higher education settings such as master’s and doctoral programs, as they are significantly less likely to be accepted to colleges or universities following an in-person interview. Those that do get accepted are likely to receive less financial support than normal-weight peers (World Obesity, 2019).
Weight Stigma in the Workplace
Stigma is present at every point in the employment process. This includes career counseling, interviewing and hiring practices, salary disparities, fewer promotions, harsher disciplinary actions, and higher termination rates. Workers with obesity are less likely to work in a sales or customer-facing position and are paid less than their normal-weight counterparts for the same work. This is more pronounced for women than men.
Though it is illegal to discriminate in employment based on sexual identity or orientation, pregnancy, race, national origin, religion, or disability, it is still legal to discriminate because of weight. Currently, there are no federal laws protecting an individual from weight-based workplace discrimination. Throughout the country, only one state (Michigan) has a law protecting potential employees from bias based on weight (World Obesity, 2019; Sherrell, 2021).
Weight Stigma in Close Relationships
Close relationships, including spouses/partners, children, parents, and siblings, have been found and documented to be the most common source of stigmatizing comments. In some cases, this source of stigma generates the most harmful stigmatizing encounters.
Parents of children with obesity may experience weight stigma by association, which may have direct repercussions for them, their children, and the parent-child relationship (World Obesity, 2019; Lee et al., 2021).
Weight Stigma in the Media
Weight prejudice is apparent in almost all forms of media, including children’s shows, in which characters with obesity are often stereotyped as clumsy, lazy, without friends, and present for comic relief. On television and in the movies, thin people are shown to be healthier, more successful, more likeable, and more likely to find love.
Fat people are often used for motivation. In such examples, a fat person loses weight and becomes a thin, successful and happier person. Before-and-after weight-loss photos are often posted on social media, which is also a major promoter of disordered diet trends and unproven “health tips.”
Magazines, blogs, and news publications mostly use images of thin people and run stories about weight loss and the dangers of fat. These publications also glorify restrictive eating patterns and promote harmful diet trends (World Obesity, 2019).
THE BODY POSITIVITY MOVEMENT
Body positivity has its roots in the fat acceptance movement of the late 1960s, which focused on ending fat-shaming and discrimination against people based on their size or body weight. In 2012, the movement emerged in its current form and focused on challenging unrealistic female beauty standards. As this movement has grown, the message has become “all bodies are beautiful.” The movement works to address issues that contribute to poor body image and reduce the negative effects on mental and physical health by promoting acceptance of all body shapes, sizes, genders, and skin tones. Despite its goals, this movement has been criticized because it ignores the health risks of obesity, lacks diversity, and perpetuates the focus on appearance (West, 2022).
Weight Stigma in Healthcare Settings
Medical professionals in all areas, nurses, and students in healthcare have been found to express both explicit and implicit bias toward overweight and obese individuals. Physicians generally have lower levels of respect for those with higher BMIs and generally spend less time during an office visit with them compared to their healthy-weight counterparts. Physicians can also be a direct source of stigmatizing comments. It has been found that 53% of people with overweight and obesity reported having been a recipient of inappropriate comments about their weight from their doctor.
Physicians view persons with obesity as less compliant, less motivated, less disciplined, less adherent to medications, less trustworthy, and more annoying. Additionally, as a patient’s BMI increases, physicians report less patience, less desire to help the person, less respect for the patient, and a greater perception of the patient as a waste of time.
Studies of self-reported attitudes among nurses indicated:
- 31% “would prefer not to care for individuals affected by obesity”
- 24% agreed that individuals affected by obesity “repulsed them”
- 12% “would prefer not to touch individuals affected by obesity”
In addition to stigma arising from the clinician-patient relationship, many people with obesity report a stigmatizing physical healthcare environment, which can include gowns, blood pressure cuffs, chairs, and examination tables that are unable to accommodate people with obesity (OAC, 2022; Fulton & Srinivasan, 2021; World Obesity, 2019).
When weight stigma is experienced in healthcare settings, it can result in avoidance of future care, reduced adherence to services, lower trust and communication with healthcare professionals, thereby resulting in reduced quality of care and exacerbated health disparities.
About 52% of women who are overweight or obese say their weight has been a barrier to receiving appropriate healthcare. These women are less likely to receive recommended health screenings. Obese patients are more likely to cancel or delay appointments and preventive healthcare services. They are also more likely to avoid seeking healthcare altogether. The long-term effect of avoiding healthcare services is that people with obesity may present with more advanced conditions that are then more difficult to treat (Villines, 2021).
BULLYING AND WEIGHT
Bullying is a pervasive societal issue consistently linked to negative outcomes that are emotionally, socially, behaviorally, and medically related. Most youth will encounter this negative event in their childhood either through being a perpetrator, being victimized, or witnessing others being bullied.
Characteristics of bullying include:
- Intent to harm
- Repetition over time or across environments
- Imbalance of power between perpetrator and victim
Bullying is defined as any unwanted aggressive behavior(s) by family members, other youth, a group of youths who are not siblings, or current dating partners; and it involves an observed or perceived power imbalance, is repeated multiple times, or is highly likely to be repeated. There are four types of bullying: physical, verbal, social or relational, and electronic. Most bullying incidents occur in the presence of bystanders, leading researchers to believe that bullying is a group phenomenon (Damme, 2019).
Among children and adolescents, weight stigma is primarily expressed through teasing and bullying. Adolescents identify weight as the primary reason for harassment among their peers. Youth who are overweight and obese are more likely to experience bullying victimization, including relational, verbal, and physical, than their average-weight counterparts.
In general, females are at greater risk of psychological distress and internalizing disorders, including generalized anxiety and major depression as a result of bullying. Social and emotional consequences are worse and occur at lower BMIs for girls/women than for boys/men (Patte et al., 2021).
CASE
Stigmatization
At the Longview Bariatric Center, in order for the bariatric team to better understand the issues of stigma and discrimination, a group counseling session was offered to participants willing to talk about their experiences of being overweight. The session was scheduled to last 90 minutes and was headed by Bria, a bariatric nurse practitioner. Seven individuals were enrolled, four women and three men between the ages of 23 and 42.
Following introductions, Bria explained the purpose of the session and asked the participants to describe some of their experiences of interactions socially, at work, in education, and in healthcare. Initially, people were reluctant to share these feelings because, as one participant, Sheila, said, “It’s so hard to talk about.”
Bria asked Sheila to explain, and she replied, “Well, I know people look at me and think, ‘She’s fat and ugly.’ It’s written on their faces—a look of pity or disgust. They don’t say it, but it’s obvious.” Another member of the group, Rick, added, “Sometimes they don’t even try to hide it.”
Everyone in the group described how their social interactions were impacted, with the strongest impact being on the younger women in the group. “People just don’t want to spend time to get to know you when you’re big,” said Latoya.
Among the group, many had experienced discrimination in looking for employment as well as in their workplaces. Helene reported that when she had applied for a job once, “they said they couldn’t employ me because I was too big to sit at their reception desk. I didn’t project the image they wanted for the company. I felt mortified.”
In the area of schooling, Latoya said, “I remember getting teased in school about my weight and coming home every day in tears. Sometimes the other kids would call me ‘rhinoceros’ or ‘tubby.’ I would hide in the bathroom at lunchtime so I didn’t have to go to the playground.”
When Bria asked the group about their experiences with healthcare professionals and in medical settings, it led to a vigorous discussion. The majority in the group said they didn’t like having their doctors bring up their weight because they didn’t have any useful advice and didn’t say anything they did not already know.
Sheila: “Oh, they say, ‘You just have a virus, and maybe you should lose some weight.’”
Rick: “Yeah, you go in because you’ve got a bad headache, and the doc says, ‘It’s because you’re overweight.’”
Latoya: “They think you’re stupid! They say, ‘You need to stop eating so much. You need to get out and be more active. You should do this … you should do that’ … stuff all of us already know. Get this! I went to my doctor a while back for a prescription for birth control pills, and he looked at me and said, ‘You mean you’re having sex?!’”
Logan: “Oh, yeah, people look at us like we’re some kind of asexual creature.”
Mason: “I was in the hospital two months ago for surgery on my foot. The hospital gowns were too small, and the bed was too small!”
As Bria listened, many of the participants expressed how they felt judged and thought of as being lazy and stupid. They expressed negative feelings about average-weight people, and Jenny said, “Don’t you just hate them!” Bria understood those statement to be an indication of the severity to which the participants felt victimized and judged by others.
At the end of the 90 minutes, Bria thanked them all for their willingness to talk about their experiences and offered to meet with them again should they wish to do so.
(Adapted from Hayden et al., 2010)
ASSESSING FOR OVERWEIGHT AND OBESITY
Nurse practitioners, office and clinic nurses, school nurses, hospital nurses, physical therapists, and occupational therapists, among others, all play a role in the assessment and treatment of children, adolescents, and adults for overweight or obesity. Assessment guidelines include:
- Body mass index or other screening or diagnostic tool measurement
- Classification of overweight and obesity
- Past medical history
- Family history
- Social history
- Review of systems
- Physical examination
- Diagnostic testing for comorbidities
Body Mass Index (BMI)
The primary way a person is categorized as overweight or obese is by calculating body mass index, which expresses the relationship (or ratio) of weight to height. BMI is calculated as:
(Weight in pounds ÷ height in inches2) x 703
or
Weight in kg ÷ height in meters2
BMI continues to be used as a screening tool because it is inexpensive and easier than other methods and does not require technical equipment and training. However, BMI can be misleading because it does not directly calculate body fat and is not, therefore, diagnostic (CDC, 2021f).
Certain factors that affect BMI inaccuracy include:
- Biological and genetic differences among racial and ethnic groups are not taken into account.
- Athletic individuals tend to have a higher percentage of lean muscle mass and lower percentage of fat mass, which might place them incorrectly in the overweight category.
- Two people can weigh the same and have the same BMI, but risk for disease might not be the same depending on how the weight is distributed. BMI does not include waist circumference.
- BMI in the high-normal to overweight range in older adults may be protective against developing certain diseases and dying early.
(Cleveland Clinic, 2022)
BMI AND WEIGHT STATUS FOR ADULTS
BMI for adults 20 years and older is interpreted using standard weight status categories. These categories are the same for men and women of all body types and ages. The standard weight status categories are shown in the table below.
| BMI | Weight Status |
|---|---|
| (CDC, 2021f; WHO, 2022b) | |
| <18.5 | Underweight |
| 18.5–24.9 | Normal or healthy weight |
| 25.0–29.9 | Overweight (preobesity) |
| ≥30.0 | Obese |
| ≥40 | Severely (morbidly) obese |
BMI AND WEIGHT STATUS FOR CHILDREN
BMI is interpreted differently for children and teens even though it is calculated in the same manner as adult BMI. The BMI in children and teens needs to be age- and sex-specific since the amount of body fat changes with age and differs between boys and girls. All children older than 2 years should have their BMI calculated at least annually from measured height and weight.
After BMI is calculated for children and teens, it is expressed as a percentile. The percentile can be obtained from either a graph or a percentile calculator, which expresses a child’s BMI relative to other children of the same age and sex. BMI-for-age percentile growth charts are the most commonly used indicator to measure the size and growth patterns of children and teens in the United States.
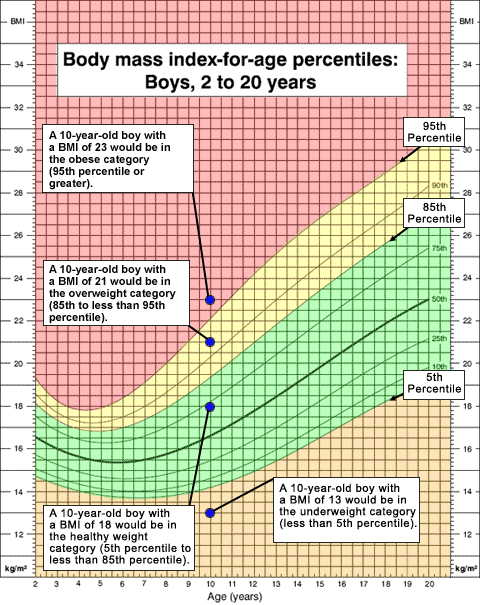
Example of BMI growth chart. (Source: CDC, 2021f.)
| BMI Percentile | Weight Status |
|---|---|
| *For children under 2 years of age, consult WHO Child Growth Standards. (CDC, 2021f) |
|
| <5th percentile | Underweight |
| 5th to <85th percentile | Normal or healthy weight |
| 85th to <95th percentile | Overweight |
| ≥95th percentile | Obese |
OBESITY CLASSIFICATIONS
There are several classifications for degrees of obesity, with the most widely accepted being those from the World Health Organization (WHO) based on BMI (see table below).
| BMI | Classification |
|---|---|
| (WHO, 2022b) | |
| 25–29.9 | Grade 1 overweight |
| 30–39.9 | Grade 2 overweight (commonly called obesity) |
| ≥40 | Grade 3 overweight (commonly called severe or morbid obesity) |
Other Screening and Diagnostic Tools
BMI has long been used as a way to define obesity in the United States, but experts are becoming increasingly critical of the approach, saying it does not paint a full picture of our health. Other tools are available, and the choice of the method for measuring weight or body fat composition depends on whether it is being obtained for clinical purposes or research and what degree of precision is required.
Other options that can be used to determine overweight or obesity include the following:
- Skinfold thickness uses calipers to determine how much body fat sits on top of muscle. It is a useful way of determining where the biggest fat deposits are, but it requires significant training to perform it properly and retraining to ensure healthcare workers continue to perform it correctly. If done correctly, skinfold thickness can be up to 98% accurate in determining body fat.
- Dual energy X-ray absorptiometry (DXA body scan) is more accurate than BMI but also much more expensive. It is generally the preferred method in a clinical setting when a more rigorous determination of body composition is needed. It uses a very low dose of radiation and is fairly simple for an operator to perform. Two beams are used to scan the body. One beam is absorbed more by fat than the other, so the computer can differentiate fat from other tissues, providing a percentage of body fat. It is widely considered the gold standard for measuring body tissue, bone, muscle, and fat.
- Waist circumference measurement has been found to be a useful (although not a completely accurate) predictor of obesity-related health risks. The National Heart, Lung, and Blood Institute recommends that waist circumference be <40 inches for men and <35 inches for women.
- Waist-to-hip ratio (waist circumference divided by hip circumference) is a measure of fat distribution. Those with abdominal adiposity are at increased risk of comorbidities. Men with a waist-hip ratio of 0.95 or more and women with a ratio of 0.85 or more are considered to be at increased cardiovascular risk.
- Bioelectrical impedance analysis is simple and widely used and relies on an electrical current to measure the fat and fat-free mass of the body. Accuracy in placement of electrodes is essential, as variations can result in large errors. Impedance is measured by applying electrodes to one arm and one leg or by having the individual stand on the foot plates of a special scale.
- CT or MRI imaging techniques can reliably determine patterns of body fat distribution. It is possible to obtain an accuracy of <1% margin of error using a series of scans.
- Nuclear magnetic resonance spectroscopy is similar in technology to MRI but is capable of discerning fat and glycogen within tissues as well as fat and lean mass overall.
- Hydrodensitometry (underwater weighing) is based on the fact that lean body tissue is denser than fat. This technique involves weighing a person on dry land and again while completely submerged under water. Underwater weighing was long considered to be the gold standard for determining body composition but has largely been replaced by newer methods. Equipment for hydrodensitometry is usually only available in research facilities.
- Whole-body plethysmography uses air displacement rather than water displacement. The person is placed sitting inside a special enclosed chamber after being weighed on a scale to determine mass measurement, and sensors determine the amount of air displaced by the person’s body. Body fat and lean muscle mass can then be calculated. This method works well in adults, school-aged children, and infants (using a device specifically designed for this age group) (Perreault, 2021a; Phillips & Shulman, 2021).
- Relative fat mass index (RFM) is a newer, better measure of body fatness than many indices currently in use, including BMI. RFM closely matches results obtained by DXA body scan. RFM is obtained simply by measuring height and waist circumference and plugging the figures into the following formula:
- Men: 64 – (20 x height/waist circumference) = RFM
- Women: 76 – (20 x height/waist circumference) = RFM
| Classification | Females (% fat) | Males (% fat) |
|---|---|---|
| (MDApp, 2020) | ||
| Essential fat | 10–13 | 2–5 |
| Athletes | 14–20 | 6–13 |
| Fitness | 21–24 | 14–17 |
| Average | 25–31 | 18–24 |
| Obese | ≥32 | ≥25 |
Past History
Determining a patient’s past history is focused on investigating the cause of obesity or overweight and should include:
- Age of onset of weight gain. The risk for any given degree of obesity seems to be greater in patients whose obesity begins before the age of 40 years, allowing a longer time period over which comorbid conditions can develop. Children with a low birth weight and those whose weight rises more rapidly in their first 10 years are at high risk for diabetes as adults. Children with obesity at age 7 and continue with obesity throughout puberty will almost certainly have it as adults. Even very modest weight gain after age 18 is also important, increasing the risk of cardiovascular disease and type 2 diabetes at all levels of initial BMI.
- Family history. The risk of comorbidities of obesity is greatly influenced by family history. Obesity in one or both parents is a predictor for the persistence of a child’s obesity into adulthood. Family history should include information about obesity in first-degree relatives (parents and siblings) and common comorbidities of obesity in first- and second-degree relatives (grandparents, uncles, aunts, half-siblings, nephews, and nieces).
- Developmental history. For children it is important to include history of growth delay and pattern of weight gain, as well as history of asthma or childhood cancers, both of which may contribute to the development of childhood obesity.
- History of weight-loss attempts can provide relevant insights into current weight-loss management strategies as well as evidence of eating disorders such as bulimia nervosa and binge eating.
- Dietary history includes an assessment of eating patterns (timing, content, and location of meals and snacks) and identification of foods that should be reduced, eliminated, or replaced.
- Eating disorders are present in almost 30% of patients who are obese. Identify bingeing, purging, lack of satiety, food-seeking behavior, night-eating syndrome, and other abnormal feeding habits.
- History of physical activity includes an assessment of frequency, duration, and intensity of physical activities such as formal exercising, transportation, occupation, household tasks, recreation, and time spent in sedentary activities. In addition, for children and adolescents, this history includes identification of barriers to walking or riding a bike to school, evaluations of time spent in play, school recess, physical education, and after-school and weekend activities, including frequency and intensity.
- Current and past medications. Medication-related weight gain is not uncommon, especially with certain types of drugs, including some diabetic medications, antipsychotics, antidepressants, and antiepileptics.
- Current health habits, including tobacco use and drug and alcohol use.
- History of smoking cessation. Cigarettes reduce appetite, and nicotine speeds up metabolism, increasing the number of calories used. On average, people gain 5 to 10 pounds in the months after they give up smoking.
(Perreault, 2021b; Vorvick, 2020; Klish, 2020; Hamdy, 2022)
Review of Body Systems
An inventory of body systems is completed in order to identify signs or symptoms a person may be experiencing or has experienced related to overweight and obesity, including:
- Obesity secondary to genetic syndromes, hormonal disease, iatrogenic medications
- Polycystic ovary syndrome (oligomenorrhea or amenorrhea)
- Low testosterone level, low sex drive, or erectile dysfunction in men
- Obstructive sleep apnea, hypoventilation syndrome
- Osteoarthritis in adults
- Foot, hip, or knee pain (orthopedic issues, slipped capital femoral epiphysis in children)
- Urinary stress incontinence
- Abdominal pain (gastroesophageal reflux disease, gallbladder disease, pancreatitis)
- Disability/immobility
- Blurred vision, history of glaucoma, diabetic retinopathy
- Psychological disorder and/or stigmatization, anxiety, depression, ADHD, PTSD, social isolation
- Medications being taken for depression or anxiety
- Polyuria, polydipsia, polyphagia (type 2 diabetes mellitus)
- Headaches (idiopathic intracranial hypertension, aka pseudotumor cerebri)
- Obesity secondary to genetic syndrome
(AACE, n.d.)
Physical Examination
Physical examination includes obtaining vital signs, height, weight, and BMI, and a complete head-to-toe examination in order to rule out any medical conditions that can be the cause of obesity and to assess for comorbid conditions.
General
- Sex, race, body build
- Obvious dysmorphic or distinguishing features that may suggest a genetic syndrome
- State of development in relation to chronological age (especially important in childhood and adolescence regarding evidence of secondary sex characteristics)
- Functional mobility, posture, gait
- Hygiene
Vital Signs
- Blood pressure. Elevated blood pressure may be a sign of Cushing’s syndrome. Normal blood pressure in adults ranges from 110/75 to 130/85. Pediatric blood pressure levels are interpreted based on sex, age, and height. Normal blood pressure values for children and adolescents are shown in the table below:
NORMAL BLOOD PRESSURE IN CHILDREN
(in mmHg)Age (years) Boys Girls (Mattoo, 2021) 1 98/52 98/54 3 101/58 102/60 5 103/63 104/64 7 106/68 106/68 9 107/70 108/71 11 110/74 111/74 ≥13 120/80 120/80
Head, Eyes, Ears, Nose, and Throat
- Microcephaly, a feature of Cohen syndrome (aka Pepper syndrome)
- Poor linear growth in children, which may be due to hypothyroidism, Cushing’s syndrome (high levels of cortisol), or Prader-Willi syndrome (a rare disorder present at birth)
- Papilledema, an optic disc swelling secondary to elevated intracranial pressure seen in patients with pseudotumor cerebri
- Nystagmus or visual complaints, which may be related to hypothalamic-pituitary lesion
- Clumps of pigment in the peripheral retina, which may indicate retinitis pigmentosa (Bardet-Biedl syndrome)
- Tonsillar enlargement secondary to sleep apnea
- Erosion of tooth enamel resulting from self-induced vomiting in those with an eating disorder
Skin and Hair
- Acanthosis nigricans, seen in those who have diabetes or prediabetes (children with acanthosis nigricans being at high risk of developing type 2 diabetes later in adulthood)
- Hirsutism and excessive acne, which may be related to polycystic ovary syndrome
- Skin tags, seen commonly with insulin resistance
- Purple striae on the abdomen, lower flank, breasts, hips, buttocks, shoulders, upper thighs, upper arms, and axillae, which is caused by rapid weight gain due to Cushing’s syndrome
Cardiac and Respiratory
- To exclude cardiomegaly and respiratory insufficiency
Abdomen
- Abdominal tenderness, which may be related to gallbladder disease, GERD, or nonalcoholic fatty liver disease
- Hepatomegaly and hepatic tenderness due to nonalcoholic fatty liver disease
Genitourinary
- Undescended testicles, small penis, or scrotal hypoplasia, which can occur in children with Prader-Willi syndrome
- Small testes, which may suggest Bardet-Biedl syndrome
- Delayed or absent puberty
- Precocious puberty
Extremities
- Limited hip range of motion, which could suggest a slipped capital femoral epiphysis
- Lower-leg bowing caused by Blount disease, in which the medial side of the tibia, immediately distal to the knee joint, fails to develop normally
- Pes planus (flat feet) and pronation of the feet, common in obese children
- Dorsal finger callouses, which may indicate self-induced vomiting
- Malformed or misshapen body parts (extra digit next to the fifth digit may present in Bardet-Biedl syndrome, small hands and feet in Prader-Willi syndrome)
- Evidence of osteoarthritis
(Burridge et al., 2022)
Laboratory Studies
ADULTS
Standard laboratory studies in the evaluation of an adult patient with obesity include:
- Fasting lipid panel. At minimum, fasting cholesterol, triglycerides, and high-density lipoprotein cholesterol (HDL-C) levels should be done. Increased low-density lipoprotein cholesterol (LDL-C) and normal or marginally increased total cholesterol are not uncommon among obese individuals.
- Liver function studies results are normal in most obese patients. However, elevated transaminase levels may indicate nonalcoholic steatohepatitis (NASH) or fatty infiltration of the liver.
- Thyroid function tests. Although hypothyroidism itself rarely causes more than mild obesity, these tests can rule out primary hypothyroidism. Screening with a serum thyrotropin level is recommended as adequate. TSH levels are commonly elevated in persons with obesity.
- Glucose and insulin studies. All patients with obesity should be screened for diabetes and prediabetes, including a fasting glucose and hemoglobin A1C (HbA1C).
Other laboratory tests should be done as indicated by clinical findings and suspicions. When Cushing’s syndrome or other hypercortisolemic states are suspected, a 24-hour urinary free-cortisol test should be included (Hamdy, 2022).
CHILDREN AND ADOLESCENTS
Laboratory evaluation for children with obesity is focused on identification of any genetic or hormonal disorder that may be a cause of obesity in a child. The following is the suggested routine screening:
- Fasting lipid panel, done once between the ages of 9–11 and again between 17–21 for detection of dyslipidemia
- Glucose and insulin studies, including serum hemoglobin A1C level as well as fasting and two-hour glucola glucose and insulin levels for evaluation of glucose tolerance and insulin resistance
- Thyroid function tests
- Liver function studies to screen for non-alcoholic fatty liver disease
In addition to the above, the following studies are included based on history and physical examination:
- Serum leptin level (recognizing that a genetic mutation lowers leptin level leading to decreased satiety)
- Adrenal function tests (recognizing that cortisol levels are commonly elevated in patients with obesity) to assess possibility of Cushing’s syndrome
- Karyotype with florescence in situ hybridization (FISH) for Prader-Willi syndrome
- Growth hormone secretion and function tests
- Assessment of reproductive hormones, including prolactin
- Serum calcium, phosphorus, and parathyroid hormones to evaluate for suspected pseudohypoparathyroidism
- MRI of the brain, with focus on the hypothalamus and pituitary
(Schwarz, 2020; AACC, 2022)
CASE
Kevin, Age 7
Kevin was screened for overweight and obesity at school. He and his parents were referred to the nurse practitioner for assessment because he had a steadily increasing BMI over the past six months. At the initial appointment, height and weight were obtained, and BMI was calculated and added to his current chart. He is now in the 92nd percentile, which classifies him as overweight.
In taking a family history, the nurse practitioner learned that Kevin’s mother, age 32, has always been overweight and is constantly dieting to maintain her weight. She is also taking medication for hypertension. Kevin’s father is 33 years old. His weight has been normal all his life and his blood pressure is also normal. Kevin’s maternal grandmother, age 57, is overweight and has type 2 diabetes. His maternal grandfather is 58 and of normal weight; he recently suffered a stroke. Both paternal grandparents are in their late 50s and are of normal weight. The grandfather suffers from angina pectoris. Grandmother is in good health. The nurse discussed Kevin’s increased risk for obesity and comorbidities based on this history.
A review of systems reveals that Kevin enjoys school and has a number of friends he plays with both at school and after school. His mood is most often upbeat. He has no symptoms of diabetes and denies headache or breathing difficulties. He sleeps 8 to 10 hours every night. Kevin denies any abdominal discomfort and reports he has regular bowel movements. He denies any foot, hip, or knee pain. Kevin has no allergies to medications and is currently on no medications.
On physical examination Kevin is a White, well-developed, overly nourished, smiling young boy with a small frame and normal musculature, round trunk, and protruding abdomen. There are no obvious dysmorphic features. He has a normal gait, erect posture, and shows good hygiene.
- Vital signs: within normal limits, BP 105/65
- HEENT (head, ears, eyes, nose, throat): face symmetrical with no abnormalities; eyes, PERRLA, no papilledema; no tonsillar enlargement; thyroid normal; lungs, normal breath sounds; teeth in good condition
- Skin: overall even color; no areas of hyperpigmentation, growths, or striae; normal hair distribution
- Heart: normal heart sounds, regular rhythm, no murmurs
- Lungs clear to A and P
- Abdomen: presence of excess adipose tissue, normal bowel sounds, no evidence of discomfort or tenderness to palpation, no hepatomegaly
- Genitalia: normal for age penis, both testes descended, no hernias
- Extremities: no edema, normal pulses, no deformities, no gait deviations observed
Because Kevin is in the 92nd percentile for BMI and has risk factors (maternal overweight and hypertension and family history of stroke, cardiovascular disease, and type 2 diabetes mellitus), a fasting lipid panel and glucose levels were obtained. Liver function studies were deferred at this time. Fasting blood glucose was 80 mg/dl, cholesterol 150 mg/dl, and LDL 100 mg/dl, all of which were in the normal range.
MANAGEMENT AND TREATMENT OF OBESITY IN ADULTS
Effective management, as with all chronic medical conditions, must be based on a partnership between a highly motivated patient and a team of health professionals, which may include a physician, psychologist, psychiatrist, advanced practice nurse, social worker, case manager, pharmacist, physical therapist, occupational therapist, dietitian, and other specialists, depending on the person’s comorbidities. Scientific evidence indicates that multidisciplinary programs reliably produce and sustain modest weight loss between 5% and 10% for the long-term.
Management strategies include:
- Lifestyle interventions using diet and physical activity
- Behavioral therapy, including assessing readiness for change
- Pharmacotherapy
- Surgery
Lifestyle Intervention for Adults
Initially, management requires the recognition that medical advice to “just eat less and exercise more” is not effective for patients to succeed at losing weight and maintaining that weight loss. Most individuals who are overweight or obese have already tried self-help approaches well before medical intervention is considered.
The patient’s weight management history can be a starting point in determining the choice of a treatment plan, which should begin with comprehensive lifestyle management, including diet, physical activity, and behavior modification. This plan should include:
- Self-monitoring of caloric intake and physical activity
- Goal setting
- Stimulus control
- Nonfood rewards
- Relapse prevention
WEIGHT-LOSS GOALS
An individual’s body weight and body fat are steadfastly regulated, and this is the basis of the challenge in losing weight and maintaining weight loss. Because of this, current thinking in the medical management of obesity has moved from a goal of massive weight loss to one of eliminating obesity-related comorbidities or reducing them to a minimum. Data previously suggested that approximately 10% of body weight loss in persons who are obese is associated with substantial health benefits. Newer guidelines indicate that clinically meaningful health improvements can be seen with weight loss in the range of 2% to 5% (Hamdy, 2022).
The weight-loss goal for each patient must be individualized; however, a reasonable goal in the setting of a medical treatment program is approximately 1 to 2 pounds per week. Factors that are considered in setting a weight-loss goal include the weight of other family members as well as the patient’s cultural, ethnic, and racial background. There is evidence that greater weight loss can be achieved with a culturally adapted weight-loss program than with a more general health program.
DIET
Current findings indicate that many types of diet can be successful in losing weight. The best predictor of success is dietary adherence. Therefore, providers are advised to recommend diets to improve adherence according to patient preference.
Diet composition is important, but the key factor in promoting weight loss is a negative energy balance. Conventional diets can be classified broadly into two categories: 1) balanced, low-calorie diets (or reduced portion sizes) and 2) diets with different macronutrient compositions such as low-fat, high-protein, or low-carbohydrate diets (Perreault & Delahanty, 2021).
Low-Calorie and Reduced-Portion Diets
Balanced, low-calorie diets and reduced-portion diets are those that dietitians and other weight-management professionals most commonly recommend. These diets underlie most of the commercial weight-loss programs, such as Weight Watchers, Take Off Pounds Sensibly (TOPS), and Overeaters Anonymous (OA). They are useful for short-term weight loss, but none of them are associated with reliable sustained weight loss. Diet-induced weight loss can result in increased levels of hormones that increase appetite. After successfully losing weight, these circulating levels of hormones do not decrease to levels prior to the weight loss, thus requiring long-term strategies to prevent obesity relapse.
Low-calorie diets involve reducing daily caloric intake by 500–1,000 kcal/day to a level of 800–1,800 kcal/day. They are associated with a mean weight loss of 1 to 2 pounds per week. A low-calorie diet may consist of a mix of meal replacements and regular foods divided among three or more meals throughout the day. Alcohol, sodas, most fruit juices, and highly concentrated sweets are generally prohibited or reduced to a minimum (Hamdy, 2022).
Potential complications of these diets can include:
- Vitamin deficiency
- Starvation ketosis
- Electrolyte derangements
- Cholelithiasis
Low-calorie versions considered healthy include:
- Mediterranean diet:
- High level of monosaturated fat, such as olive oil
- Fish
- Nuts
- Moderate consumption of alcohol, mainly as wine
- High consumption of vegetables, fruits, legumes, beans, and grains
- Moderate consumption of milk and dairy products, mostly cheese
- Low intake of meat and meat products
- Dietary Approaches to Stop Hypertension (DASH):
- 6–8 servings of grain/day
- 4–5 servings of fruit/day
- 4–5 servings of vegetables/day
- 2–3 servings of fat-free or low-fat dairy/day
- 6 or fewer 1-ounce servings/day of lean meats, poultry, and fish
- 4–5 servings of nuts, seeds, and legumes per week
- 2–3 servings fats and oils/day
- <5 servings per week of sweets and added sugars
- Less than 25% dietary intake from fat
Reduced-portion diets may be based on regular, everyday foods; by participation in a structured weight-loss program (e.g., Jenny Craig, Nutrisystem); or by incorporating products such as meal-replacement shakes, prepackaged meals, and frozen entrees (e.g., Lean Cuisine, Healthy Choice). These have adequate amounts of major macronutrients based on the food pyramid from the USDA and recommended daily allowances (RDAs). Alcohol, sodas, most fruit juices, and highly concentrated sweets are calorie dense and nutrient deficient and are generally prohibited or reduced to a minimum (Hamdy, 2022).
Very low-calorie diets (VLCDs) are those with energy levels between 200 and 800 kcal/day, while those below 200 kcal/day are termed starvation diets. Although once popular, starvation diets are not recommended for treatment of obesity. Very low-calorie diets should only be undertaken under a doctor’s supervision and paired with specialty foods to prevent nutrient deficiencies.
VLCDs are associated with profound initial weight loss of up to 3 to 5 pounds per week, much of which is from loss of lean tissue mass in the first few weeks, and have been shown to be superior to conventional diets for long-term weight loss. Most VLCDs use meal replacements such as formulas, soups, shakes, and bars instead of regular meals in order to ensure adequate intake of nutrients. VLCDs are “drastic measures” recommended only for adults who are obese and need to lose weight quickly for health reasons. However, if prescribed for children, adolescents, or elderly patients, special precautions should be taken. The use of VLCDs is contraindicated in the following settings:
- Pregnancy
- Protein-wasting states
- Clinically significant cardiac, renal, hepatic, psychiatric, or cerebrovascular disease
- Any other chronic diseases
VLCDs are often used before weight-loss surgery and are only recommended for a period of up to 12 weeks. Compliance beyond a few weeks is poor, and close supervision is required. Adverse effects can include hair loss, skin thinning, hypothermia, cholelithiasis, ketosis, vitamin deficiency, electrolyte derangement, and emotional problems.
Diets with Different Macronutrient Compositions
Macronutrients refer to carbohydrates, fats, and proteins. Some diets emphasize manipulation of these macronutrients in order to promote weight loss. There is moderately certain evidence that, over six months, most macronutrient diets result in modest weight loss and substantial improvements in cardiovascular risk factors. At 12 months, the effects on weight reduction diminishes and blood pressure improvements largely disappear (Long et al., 2020).
Low-Carbohydrate Diets
While all low-carbohydrate diets reduce the overall intake of carbohydrates, there is no clear consensus on what defines a low-carb diet. However, a daily limit of 20–57 grams of carbohydrates is typical with a low-carb diet.
Low-carbohydrate approaches to weight loss are based on the hypothesis that lowering insulin, a critical hormone that produces an anabolic, fat-storing state, improves cardiometabolic function and results in weight loss. Studies thus far have shown low-carb diets, and specifically ketogenic diets, to be superior to other dietary approaches in producing rapid weight loss for the first 6 to 12 months. A low-carbohydrate diet includes:
- Lean meats, such as sirloin, chicken breast, or pork
- Fish
- Eggs
- Nonstarchy vegetables, e.g., leafy green vegetables, cauliflower, and broccoli
- Nuts and seeds, including nut butter
- Oils, such as olive, coconut, and rapeseed
- Some fruits, such as apples, blueberries, and strawberries
- Unsweetened dairy products, including plain whole milk and plain Greek yogurt
When there is a lower intake of carbohydrates, the intake of fat and protein generally increases to compensate for the reduction. It is believed that low-carb diets produce rapid weight loss compared to other diets because fats and protein increase satiety and produce less accompanying hypoglycemia, which reduces hunger and overall food intake.
Types of popular-named, low-carbohydrate diets include:
- Atkins Diet
- Low-carb Paleo
- Whole30
- Low-carb Mediterranean
- South Beach
- The Zone
The ketogenic diet, a specific version of low-carb and high-fat diet, restricts carbohydrates to induce nutritional ketosis (but does not produce metabolic ketosis) and typically limits carbs to 20–50 gm/day. Restricting carbs to under 50 gms induces glycogen depletion and ketone production from the mobilization of fat stored in adipose tissue. Side effects of this type of diet include:
- Constipation due to low fiber intake
- Muscle cramps
- Halitosis (bad breath)
- Risk of “keto flu,” which may include headaches, fatigue, brain fog, irritability, lack of motivation
(Oh et al., 2021)
Low-Fat Diets
Low-fat dietary guidelines recommend a reduction in daily intake of fat to less than 30% of energy intake per day, and very low–fat diets provide less than 10% to 15%. The main premise behind this recommendation is that fat provides a higher number of calories per gram (9) compared to proteins and carbs (4). People who reduce their calorie intake by eating less fat do lose weight, and although the average loss is small, it is considered relevant for health. A low-fat diet may consist of:
- Whole grains, vegetables, and fruit at every meal
- Beans, peas, lentils
- Limited intake (6 ounces per day) of lean meat, fish, poultry without skin, and egg whites
- No more than 3 teaspoons of fat per day (vegetable oils)
- Low-fat or fat-free sweets and snack foods in moderation
- Fat-free or low-fat dairy
(Perreault & Delahanty, 2021)
Restricting fat too much can lead to health problems in the long term, as fat plays a key role in the production of hormones, nutrient absorption, and cell health. Consequences of low-fat eating can include:
- Flaky, dry skin
- Mood imbalances
- Hormone imbalances
- Constant hunger and cravings
- Poor vitamin absorption
- Very low-fat diets have been linked to a higher risk of metabolic syndrome
Types of popular-named low-fat diets include:
- Ornish diet
- Therapeutic Lifestyle Changes (TLC) diet
- Engine2
(Long et al., 2020)
High-Protein Diets
High-protein diets have been recommended for obesity treatment because they can help build lean muscle (which increases the number of calories burned throughout the day) and are more satiating and stimulate thermogenesis. High-protein diets may also improve weight maintenance. Like low-carbohydrate diets, high-protein diets can produce a state of ketosis. Some high-protein foods include:
- Legumes
- Dried beans
- Salmon
- Potatoes
- Meat
- Fish
- Eggs
- Dairy
- Peanut butter
- Tofu
(Perreault & Delahanty, 2021)
Popular-named high-protein diets include:
- Protein Power diet
Intermittent Fasting
Intermittent fasting is an eating plan that cycles between periods of fasting and eating on a regular schedule. There are many different intermittent fasting schedules one can follow, such as eating only during an eight-hour period each day and fasting for the remainder. Or, it may involve eating only one meal a day two days a week. After hours without food, the body exhausts its sugar stores and starts burning fat. During times when the person is not eating, water and zero-calorie beverages are permitted.
It is recommended that individuals who are undertaking intermittent fasting for weight loss use the Mediterranean diet as a guide for the types of foods to be eaten.
Research to date has found that intermittent fasting:
- Boosts working and verbal memory
- Improves blood pressure and resting heart rates
- Improves physical endurance
Intermittent fasting is not recommended for:
- Children and teens under age 18
- Women who are pregnant or breastfeeding
- People with diabetes or blood sugar problems
- Those with a history of eating disorders
(Johns Hopkins Medicine, 2022)
PHYSICAL ACTIVITY
Physical inactivity is a primary contributor to obesity and is often targeted for intervention because it is modifiable at the individual level. Creating a negative energy balance by decreasing calorie consumption and increasing activity is a common strategy in the management of overweight and obesity. Physical activity is an important lifestyle behavior associated with long-term weight loss and prevention of weight gain following initial weight loss.
Weight loss by diet without physical activity, especially in older people, can increase frailty due to age-related losses in bone density and muscle mass. Adding aerobic and resistance activity counters such loss.
Physical activity prevents obesity by:
- Increasing total energy expenditure
- Decreasing fat around the waist and total body fat
- Slowing the development of abdominal obesity
- Helping build muscle mass, which increases energy burned even when at rest
- Reducing depression and anxiety, which can help with motivation
(Harvard T.H. Chan, 2022a)
The U.S. Department of Health and Human Services makes the following recommendations for physical activity:
- Moderate-intensity aerobic activity: 150 minutes per week of moderate activity or 75 minutes per week of vigorous activity. This can be spread out over the course of the week in sessions at least 10 minutes long.
- Strength training: At least twice a week, no specific amount of time is specified.
- Moderate-to-vigorous physical activity: 60 minutes or more daily for children and adolescents ages 6–17 years.
(CDC, 2019; CDC, 2020)
For those who are keeping track of calories taken in and expended, it is helpful to know approximately how many calories are burned during a chosen activity in 30 minutes (see table below).
| Activity | 125-pound person | 155-pound person | 185-pound person |
|---|---|---|---|
| (Harvard Medical School, 2021) | |||
| Sleeping | 19 | 22 | 26 |
| Sitting/Reading | 34 | 40 | 47 |
| Cooking | 57 | 70 | 84 |
| Food shopping | 85 | 106 | 126 |
| Low impact aerobics | 165 | 198 | 231 |
| High impact aerobics | 210 | 252 | 294 |
| Walking 3.5 mph | 107 | 133 | 159 |
| Hiking cross country | 170 | 216 | 252 |
| Biking 12–13 mph | 210 | 252 | 294 |
| Running 5 mph | 240 | 288 | 336 |
| Swimming | 180 | 216 | 252 |
THE ROLE OF PHYSICAL THERAPY
Physical therapists are an important part of the multidisciplinary team working with individuals with obesity. Physical therapists assist patients to become more physically active by teaching ways to exercise without causing pain and that are enjoyable. Therapists determine an appropriate treatment program for each individual that includes aerobic exercise and strength training.
Physical therapists also help patients explore the underlying reasons for their behaviors and to identify barriers to developing more healthy habits. They work with the patient to set individualized, realistic goals and assist the patient to stay with the program. The following are ways in which physical therapists work with bariatric patients:
- Pain reduction. By designing a personalized exercise program, the therapist can help with the performance of activities with the least amount of pain. Although the person may experience pain with activity, the activity itself may help reduce pain.
- Cardiovascular health. Physical therapists develop aerobic exercise programs that are heart-healthy, elevate metabolism, and burn more calories.
- Movement. Physical therapists work with patients to help restore normal range of motion of the joints, progressing from passive exercises to active exercises.
- Muscle strength. Physical therapy helps to improve muscle strength by addressing muscle weakness and developing gentle and low-impact resistance forms of weight training to improve overall strength and relieve joint discomfort. Because muscle burns more calories than other body tissues, muscle-building exercises can benefit weight-loss efforts.
- Flexibility and posture. The physical therapist works with patients to gently stretch tight major muscles and to improve and maintain proper posture, which is essential in performing difficult activities with ease, less discomfort, and respiratory function.
(APTA, 2021)
Behavioral Modification
Changing behavior—especially long-term, habitual patterns—and getting oneself to do something different even when it is known to be the best thing to do, depends on an individual’s mindset. Mindset refers to the belief in one’s limitations. A fixed mindset focuses on what is known and the belief that basic abilities and talents are fixed traits that cannot be changed. A growth mindset focuses on improving what and how one does things. In order to lose weight and keep it off, people often must learn to think differently about what they eat, when they eat, and how they eat.
ASSESSING READINESS TO CHANGE
Efforts aimed at behavioral change begin with the clinician’s determination of a patient’s readiness to change as well as the readiness of parents and families of obese children and adolescents to change. One model for assessing such readiness is the Transtheoretical Model, which explores the individual’s feelings, awareness, judgments, perceptions, and behavior, and describes the process of change using five stages.
- Precontemplation. Individuals in this stage have no intention of changing or taking action within the near future. People are often uninformed about the consequences of overweight and obesity, they may have failed in the past to make changes or lose weight, or they may avoid seeking any information that would help change behavior. People in this stage often underestimate the pros and place more emphasis on the cons of changing behavior.
- Contemplation. The person is considering making changes within the next 6 months and is aware of both the positive effects of making change and the negative effects of failing to change. Even with this recognition, people may still feel ambivalent toward making changes.
- Preparation (Determination). An individual in this stage of readiness is determined to take action within the next month and has usually begun to prepare a plan of action, such as a weight-loss or exercise program. At this stage they believe changing their behavior can lead to a healthier life. Individuals in this stage require assistance in the development and implementation of specific action plans and in setting realistic goals.
- Action. The person in this stage of readiness has made significant modifications in behavior and lifestyle over the past 6 months or longer and intends to keep moving forward. Assisting a person can include providing problem-based learning experiences, support, and feedback.
- Maintenance. The person has made significant modification in behavior and lifestyle and has actively worked to prevent a relapse for more than 6 months. The individual is confident that change can be maintained. At this stage, it is important to continue to provide support, assist with problem-solving, positively address slips and relapses, and employ reminder systems or performance support tools.
(LaMorte, 2019)
INTERVENTION STRATEGIES
Interventions aimed at behavioral modification are considered essential in the management of the patient who is overweight or obese. Behavioral modification methods can be used either alone or in conjunction with other treatments, working to create goals, helping to maintain goals that have already been achieved, preventing possible relapses, and managing difficult situations.
Behavioral modification interventions include face-to-face contact and are often conducted in group sessions, which may be available at local hospitals, through commercial programs, or in office settings. While some patients might prefer individual therapy, the group setting may be more cost effective, and there is insufficient evidence to conclude that one is better than the other. All interventions use similar strategies, which include the following elements:
- Collaborative setting of realistic and achievable goals, which is meant to increase motivation and adherence. These goals are Specific, Measurable, Achievable, Reasonable, and Time-bound (SMART) and should be within a patient’s control.
- Self-monitoring of food intake, weight, and activity, which is the most important step in successful behavior therapy. Self-monitoring slows down decision-making, allowing time to make healthier choices and alerting the individual about overconsumption and nutritional content of foods. Tools for self-monitoring can include keeping food diaries and activity records, internet applications, smartphone applications, and digital scales for self-weighing and recording.
- Stimulus control, which alters the person’s environment to help make better choices. Participants are educated in selecting fresh fruits and vegetables; preparing easy-to-eat, lower-calorie foods; placing them prominently in the refrigerator or on the counter; and removing less-healthy foods from the home. Stimulus control also includes setting the environment so the individual can concentrate on eating.
- Eating style, which involves slowing down the eating process to give time for physiologic signals for fullness to arise. Practicing “mindful eating” allows one to concentrate on tastes and textures of food and savor what is being eaten by chewing more slowly. Other techniques might involve leaving the table briefly during a meal and drinking water between bites or just prior to the meal.
- Portion control and meal planning, which provide a defined meal structure and can result in greater weight loss than the absence of such a structure. Use of portion-control plates or meal replacement are examples.
- Regular weighing as a self-monitoring strategy. This has been recommended in some studies. Concerns have been raised that regular weighing might lead to anxiety and weight regain, but this has not been observed in a systematic literature review.
- Increasing physical activity. Along with self-monitoring, increasing physical activity is a key element in successfully losing weight.
- Nutrition education and meal planning with a registered dietitian for assessment of knowledge and preferences.
- Social support enhancement to improve long-term weight loss. Behavioral programs that include strong family support provide both short- and long-term benefits.
- Other behavioral tools may include:
- Cognitive restructuring, such as changing self-talk (see below)
- Problem-solving, such as managing food intake in difficult situations
- Assertiveness training, such as learning to say “no”
- Stress reduction, by identifying and reducing stressors that are triggers for eating
MOTIVATIONAL INTERVIEWING (MI)
While behavioral interventions provide a variety of strategies for change, motivational interviewing addresses the specific challenges of motivation, confidence, treatment readiness, ambivalence, and resistance. It is an approach that has also been shown to be successful for individuals with substance abuse disorders.
MI assumes that behavior change is affected more by motivation than by information and that no lasting change will be achieved unless the patient sees the need to change. MI is person-centered and goal-directed, and it increases the person’s motivation for commitment to behavioral change. The hallmark of MI is working with and through a person’s ambivalence about making a change and recognizing that it is the patient who decides whether and how to change.
The core principles of MI are:
- Expressing empathy
- Supporting the person’s self-efficacy
- “Rolling” with resistance
- Developing discrepancy
MI has four fundamental processes that describe the flow of interaction. These include:
- Engaging: Establishing a productive working relationship
- Focusing: Both patient and practitioner agree on a shared purpose (negotiating/collaborating)
- Evoking: Exploring and assisting the patient to find their own “why” of change
- Planning: Providing support and exploring the “how” of making change
MI requires four communication skills that support and strengthen the process of eliciting “change talk.” Change talk are statements that the person makes that indicate being in favor of change. These skills include:
- Asking open-ended questions
- Affirming
- Reflective listening, mirroring
- Summarizing
(MINT, 2021; Ingersoll, 2022)
(See also the “Case” on motivational interviewing later in this course.)
TECHNOLOGY AND BEHAVIORAL CHANGE
Technology can also be enlisted to enhance the success of behavioral change efforts. One example, Mobile health (mHealth), with its portable, easily accessible, and ubiquitous nature, is used to monitor and promote weight loss by changing behavioral factors that contribute to a healthy lifestyle. It is supported by devices such as phones, tablets, personal computers, personal digital assistants, biosensors, and others to track and monitor diet and physical activity. Text messages are used to provide reminders or encourage certain behaviors.
MHealth has shown positive results in both adult and childhood obesity. Use of this technology provides education, clinical decision support, health promotion and awareness, remote monitoring and data collection/analysis, and integrated care and diagnostic support.
Another example, eHealth, involves internet-based programs such as web-based interactive voice response systems, a virtual world, and internet-based virtual coaching to provide an interactive platform for communication and education on diet, physical activity, and exercise.
The type of technology used has been found to be associated with weight loss. MHealth shows more instances of statistically significant association with weight loss, as compared to telehealth/telemedicine and eHealth (House et al., 2019).
THE ROLE OF OCCUPATIONAL THERAPY
Occupational therapists treat patients for the prevention and management of obesity, including helping with weight-loss efforts and adaptations for occupational challenges caused by obesity. Occupational therapists assist patients who are obese in making necessary lifestyle changes by focusing on health promotion, disease prevention, remediation, adaptation, and maintenance. Outcomes often include increased participation, increased ease when performing activities of daily living and instrumental activities of daily living that require physical activity and endurance, improved self-esteem, and decreased symptoms of depression and anxiety.
Occupational therapists enhance the person’s functional abilities in the following areas and manner:
- Activities of daily living, including strategies for maintaining good hygiene
- Supporting increased physical endurance
- Offering strategies for safe mobility in the home and in the community
- Teaching ways to conserve energy and to simplify work
- Instructing in the use of proper body mechanics to avoid injury
- Monitoring and maintaining skin integrity
- Recommending and assisting with adaptive equipment and methods to facilitate instrumental activities of daily living
- Home modification to promote participation in activities, improve environmental access, and ensure safety
- Assisting with setting routines for healthy food selection, shopping, and meal preparation
- Assisting with the establishment of sleep routines, relaxation, and positioning to increase comfort and promote adequate rest
- Providing wellness groups for patients and families to facilitate health promotion and social support
- Teaching coping strategies for management of pain, stress, and anxiety
- Addressing sexual health concerns
- Assisting individuals to participate in the community by identifying appropriate businesses and social gatherings
- Assisting individuals in making task and environmental modifications to maintain participation in roles and occupations at current body weight, and to accommodate weight management
(Dieterle, 2018)
Pharmacology
There are only a few drugs available for the treatment of obesity, and their effectiveness is limited to palliation rather than cure. Benefits fade when they are discontinued. All medications carry more risks than diet and physical activity interventions, and medications are used only in those patients for whom the benefit justifies the risk. They are not used during pregnancy or when breastfeeding.
Weight-loss drugs are considered for patients with a BMI >30 or a BMI >27 with a serious medical condition related to obesity (e.g., diabetes, hypertension).
Weight-loss drugs may not be effective for everyone. When used as part of a diet and exercise plan, typical weight loss is 5%–10% of body weight over a 12-month period.
Currently, there are three major categories of drugs used to manage obesity:
- Anorexiants are drugs that act on the brain to suppress appetite. They have a stimulant effect on the hypothalamic and limbic regions of the brain that control satiety.
- Stimulants are drugs that increase dopamine, which accelerates the autonomic nervous system and results in an increased energy expenditure.
- Lipase inhibitors impair the gastrointestinal absorption of ingested fat, which is then excreted in the stool.
| Drug | Category | Common Side Effects |
|---|---|---|
| *Approved for long-term use. (Perreault, 2022; Hamdy, 2022; Mayo Clinic, 2020a; Anderson, 2021) |
||
| Phentermine (Adipex, Lomaira) | Anorexiant and stimulant | Increased blood pressure and heart rate, insomnia, nervousness, restlessness, dependence, abuse or withdrawal with long-term use |
| Diethylpropion | Anorexiant and stimulant | Constipation, restlessness, dry mouth |
| Gelesis100 (Plenity)* | Absorbs water, increases fullness. Considered a medical device but functions as a medication | Diarrhea, abdominal distension, infrequent bowel movements, constipation, abdominal pain, flatulence |
| Phentermine and topiramate ER (Qsymia)* | Anorexiant, decreases binge eating behaviors | Constipation, restlessness, dry mouth, increased blood pressure and heart rate, insomnia, nervousness, restlessness, dependence, abuse or withdrawal with long-term use |
| Liraglutide subcutaneous injection (Saxenda)* | Anorexiant, increases satiety | Nausea, vomiting, diarrhea, constipation, headache, heartburn, fatigue, dizziness, stomach pain, gas, dry mouth, low blood sugar in type 2 diabetes, increased lipase |
| Buproprion and naltrexone (Contrave)* | Anorexiant, decreases cravings | Nausea, vomiting, headache, fatigue, constipation, dizziness, insomnia, dry mouth, diarrhea, increased blood pressure, anxiety, tremor, hot flush, unusual taste |
| Orlistat (Alli OTC, Xenical)* | Lipase inhibitor | Oily spotting, flatulence, fecal urgency, soft stools, fecal incontinence; vitamin A, D, E, and K deficiency |
| Semaglutide (Wegovy)* subcutaneous injection | Anorexiant, increases satiety | Nausea, abdominal pain, diarrhea, vomiting, constipation, headache, fatigue, dizziness, bloating, belching |
| Setmelanotide (Imcivree)* | Anorexiant, for patients 6 years and older with obesity due to three rare genetic conditions | Injection site reactions, skin hyperpigmentation, headache, gastrointestinal side effects, spontaneous penile erections in males and adverse sexual reactions in females, depression and suicidal ideation |
| Phendimetrazine (Bontril PDM) | Anorexiant | Dizziness, dry mouth, difficulty sleeping, irritability, nausea, vomiting, diarrhea, constipation |
Medical Devices
Considered medical devices, hydrogels are orally administered products. These are taken twice daily prior to meals, and expand in the stomach and intestines to create a sensation of fullness. They are not systematically absorbed and are eliminated in the stool. Hydrogels are indicated for use as weight management aids for adults with a BMI of 25–40 and are to be used in conjunction with diet and exercise. There is no restriction on how long the product can be used for weight management (Perreault & Apovian, 2021).
Weight Loss Surgical Procedures
Bariatric surgical procedures are increasingly common around the world. It is estimated that there were 394,432 bariatric procedures performed worldwide in 2018, the majority of which were performed in the United States and Canada. Surgical procedures for obesity are major, life-changing events. An individual who is considering bariatric surgery must undergo an evaluation to determine if the health benefits of surgery outweigh the potentially serious risks, and if the person is medically and psychologically able to undergo such procedures.
Candidates for bariatric surgery must meet at least one of the following criteria:
- BMI ≥40 or ≥100 pounds overweight
- BMI ≥35 and at least one obesity-related comorbidity (type 2 diabetes, hypertension, sleep apnea, other respiratory disorder, nonalcoholic fatty liver disease, osteoarthritis, lipid abnormality, gastrointestinal disorder, heart disease)
- Inability to achieve a healthy weight loss sustained for a period of time with prior weight loss efforts
It is recommended that surgery be performed by a board-certified surgeon with specialized experience/training in bariatric and metabolic surgery and at a center that has a multidisciplinary team of experts for follow-up care (ASMBS, 2022a).
Bariatric surgical procedures are contraindicated in those with:
- Untreated major depression or psychosis
- Uncontrolled and untreated eating disorders
- Current drug and alcohol abuse
- Severe cardiac disease with prohibitive anesthetic risks
- Severe coagulopathy
- Inability to comply with nutritional requirements, including lifelong vitamin replacement
Bariatric surgery in patients over 65 years is controversial but is considered when comorbidity is severe. Bariatric surgery for patients younger than 18 years is becoming more common for severe obesity (Lim, 2022).
TYPES OF BARIATRIC SURGERY
Bariatric surgical procedures cause weight loss by restricting the volume of food the stomach can hold, by causing malabsorption of nutrients, or by a combination of the two. They are performed with small incisions using minimally invasive surgical techniques (laparoscopic and robotic surgery). These advancements result in a better overall experience with less pain, fewer complications, shorter hospital stays, and a faster recovery. The operations are extremely safe, with complication rates that are lower than more common operations such as cholecystectomy, hysterectomy, or hip replacement.
The goal of the surgical procedures is to modify the stomach and intestines in order to treat obesity and related diseases. The operations may make the stomach smaller and also bypass a portion of the intestine. This results in less intake of food and changes how the body absorbs food for energy, resulting in decreased hunger and increased satiety.
After bariatric surgery, around 90% of patients lose 50% of excess body weight and keep this extra weight off long-term. In large, scientific studies of hundreds of thousands of patients, weight-loss surgery has been shown to lower a person’s risk of death from any cause by over 40% (ASMBS, 2020).
Gastric Bypass (Roux-en-Y)
The gastric bypass combines both restrictive and malabsorption approaches. The surgically created stomach pouch is smaller and able to hold less food, which means fewer calories are ingested. Also, the food does not come into contact with the first portion of the small intestine, and this results in decreased absorption.
The operation involves sealing off the upper section of the stomach from the lower section and then connecting the upper stomach directly to the bottom end of the small intestine. The procedure is completed by connecting the top portion of the divided small intestine to the small intestine further down so that stomach acids and enzymes from the passed stomach and first portion of the small intestine will eventually mix with the food.
Gastric bypass (Roux-en-Y). (Source: National Institutes of Health.)
With this procedure, weight loss usually exceeds 100 pounds or about 65%–70% of excess body weight and about 35% of BMI. Weight loss generally levels off in one to two years, and a regain of up to 20 pounds from the weight loss nadir to a long-term plateau is common. Gastric bypass is considered irreversible but has been reversed in rare cases.
Advantages:
- Reliable and long-lasting weight loss
- Effective for remission of obesity-associated conditions
Disadvantages:
- Technically more complex procedure and difficult to reverse
- More vitamin and mineral deficiencies than other procedures
- Risk for small bowel complications and obstruction
- May increase the risk of alcohol disorder
- Risk of developing ulcers, especially with NSAID or tobacco use
A significant risk for this procedure is dumping syndrome, which involves food emptying too rapidly from the stomach into the intestines before it is properly digested. Approximately 85% of people who have this procedure develop some dumping. Symptoms include nausea, bloating, pain, sweating, weakness, and diarrhea, and are often triggered by sugary or high-carbohydrate foods (Saber, 2021b; NIH, 2020).
Laparoscopic Adjustable Gastric Band
This is a restrictive procedure that involves the placement of an adjustable silicone band with an inner inflatable balloon around the top of the stomach, creating a small pouch that allows for a full feeling after eating a small amount of food (approximately one ounce). The balloon is filled with sterile saline solution, and the size of the opening from the pouch to the rest of the stomach can be adjusted as needed to reduce side effects and improve weight loss by injecting or removing the saline through a plastic tube that runs from the balloon to a small port placed under the skin.
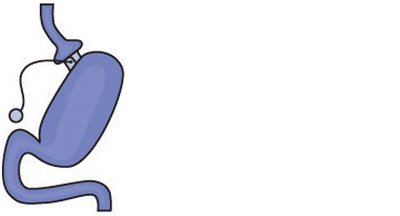
Gastric banding. (Source: National Institutes of Health.)
Advantages:
- Lowest rate of complications early after surgery
- Done laparoscopically
- No diversion of stomach or intestines
- Patients go home the day of surgery
- The band can be removed if needed
- Has the lowest risk for vitamin and mineral deficiencies
Disadvantages:
- Band may need several adjustments and monthly office visits during the first year
- Slower and less weight loss than with other surgical procedures. (The impact on obesity-related diseases and long-term weight loss is less than with other procedures, and its use, therefore, has declined over the past decade.)
- Risk of band slippage or damage to the stomach over time (erosion)
- Requires a foreign implant to remain in the body
- Has a high rate of need for re-operation
- Can result in swallowing problems and enlargement of the esophagus
(Saber, 2021b; NIH, 2020)
Gastric Sleeve
Gastric sleeve, also known as vertical sleeve gastrectomy, involves removal of 80% of the stomach, leaving a narrow tube or sleeve the size and shape of a banana, which is then connected to the intestines. This restricts the amount of food that can fit in the stomach, creating a feeling of fullness. Removal of part of the stomach also affects gut hormones and other factors such as gut bacteria that may affect both appetite and metabolism. This surgical procedure is not reversible.
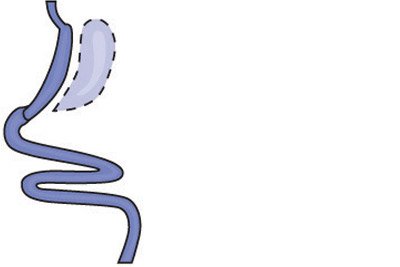
Gastric sleeve. (Source: National Institutes of Health.)
Advantages:
- Technically simple, with shorter surgery time
- Can be performed in certain patients with high-risk medical conditions
- May be performed as the first step for patients with severe obesity
- May be used as a bridge to gastric bypass or SADI-S procedures
- Offers effective weight loss and improvement of obesity-related conditions
Disadvantages:
- Nonreversible
- May worsen or cause new-onset reflux and heart burn
- Has less impact on metabolism compared to bypass procedures
- Risk of long-term vitamin deficiencies
(Saber, 2021b)
Biliopancreatic Diversion with Duodenal Switch (BPD-DS)
This is a malabsorption procedure with two components: 1) a surgery similar to the gastric sleeve creates a small tubular stomach pouch, and 2) the duodenum is divided just past the outlet of the stomach. A segment of the distal small intestine is then brought up and connected to the outlet of the newly created stomach pouch, so that when the person eats, food passes through the tube and empties directly into the last segment of the small intestine. This second surgery redirects food to bypass roughly three quarters of the small intestine. The bypassed section is then reattached to the first part of the small intestine, allowing bile and pancreatic enzymes necessary for the breakdown and absorption of protein and fat to mix with food.
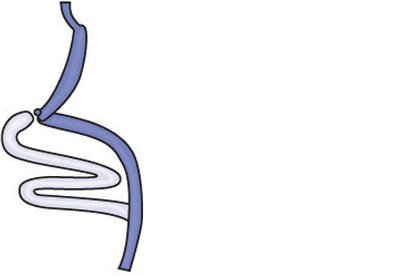
Biliopancreatic diversion with duodenal switch. (Source: National Institutes of Health.)
This procedure is more involved than a gastric bypass but can result in even greater and more rapid weight loss. Much of the stomach is removed. However, what remains is larger than the pouches formed during gastric bypass or banding, and larger meals may be eaten with this surgery. The BPD-DS is considered to be the most effective approved metabolic operation for the treatment of type 2 diabetes.
Advantages:
- Among the best results for improving obesity
- Affects bowel hormones to cause less hunger and more fullness after eating
Disadvantages:
- Slightly higher complication rates than other procedures
- More complex surgery, requiring more operative time
- Highest malabsorption and greater possibility of vitamin and micronutrient deficiencies
- Reflux and heart burn can develop or worsen
- Risk of looser and more frequent bowel movements
(Saber, 2021b; ASMBS, 2021b)
Single Anastomosis Duodenal-Ileal Bypass with Sleeve Gastrectomy (SADI-S)
SADI-S is the most recent procedure to be endorsed by the American Society for Metabolic and Bariatric Surgery. It is similar to BPD-DS, but the SADI-S is simpler and takes less time to perform, as there is only one surgical bowel connection.
The operation begins the same way as the sleeve gastrectomy, making a smaller tube-shaped stomach. The first part of the small intestine is divided just after the stomach, and a loop of intestine is measured several feet from its end and is then connected to the stomach.
When the patient eats, food goes through the pouch and directly into the latter portion of the small intestine. Food then mixes with digestive juices from the first part of the small intestine, allowing enough absorption of vitamins and minerals to maintain healthy levels.
Advantages:
- Offers good weight loss with less hunger, more fullness, blood sugar control, and diabetes improvement
- Simpler and faster to perform than gastric bypass or BPD-DS
- Excellent option for a patient who already had a sleeve gastrectomy and is seeking further weight loss
Disadvantages:
- Vitamins and minerals are not absorbed as well as in sleeve gastrectomy or gastric band
- Newer operation with only short-term outcome data
- Potential to worsen or develop new-onset reflux
- Risk of looser and more frequent bowel movements
(ASMBS, 2021a)
OTHER SURGICAL INTERVENTIONS
Intragastric Balloon Systems
These temporary devices are saline-filled silicone balloons that limit how much the stomach can hold, making the person feel fuller faster. There are three FDA-approved systems available. Two of these devices are placed endoscopically, while the other is swallowed. All three are removed endoscopically in six months.
An intragastric balloon may be an option for a person who:
- Has a BMI of 30–40 and one or more obesity-related comorbid conditions
- Has failed weight reduction with diet and exercise alone
Side effects and adverse events include nausea, vomiting, reflux, balloon migration, balloon intolerance, balloon leak, and intestinal or stomach perforation.
Balloons are typically filled with saline that is dyed blue, so if the patient’s urine turns blue or green, a leak should be suspected. This requires immediate medical attention, as the balloon would then be at risk for migrating and causing an intestinal obstruction. One of the devices (ReShape) is a two-balloon device so that if one breaks, the second balloon can prevent migration (Perreault & Apovian, 2021; Lim, 2022).
BARRIERS TO BARIATRIC SURGERY
Bariatric surgery is expensive. Even though patients may spend only two days in the hospital, these operations require the use of expensive, high-technology equipment as well as advanced nursing and surgical training. The average cost of gastric bypass surgery in the United States from 2020–2022 was $24,288, but there is a big cost difference between the states, ranging from $15,300 in Arkansas to $57,500 in Alaska.
| Type of Procedure | Average Price without Insurance |
|---|---|
| Gastric bypass | $24,288 |
| Laparoscopic adjustable gastric band | $15,180 |
| Gastric sleeve | $19,228 |
| Gastric balloon | $8,248 |
| Duodenal Switch | $27,324 |
The decision to pursue a surgical solution for treatment of obesity is often one taken by middle- to upper-income patients, since most low-income people cannot pay the cost for these procedures.
Many disabled obese patients have their healthcare coverage through Medicare. Obesity-related illnesses are primary reasons for disability coverage under Medicare. Medicare officials are very aware of the increased cost of treating all of the comorbid illness associated with obesity. Up until recently, Medicare had a clause stating that “obesity is not an illness” in their policy statement. This clause was recently deleted, with the implication that obesity therefore must be considered an illness.
Nearly all private insurance carriers in the past accepted the guidelines for weight-loss surgery. However, the recent explosion in the number of surgical procedures has resulted in many carriers adding qualifiers, such as 6 or 12 months of a continuously medically supervised diet. Most patients seeking weight-loss surgery have experienced years of failed diet treatments, but these attempts are rarely associated with written documentation and therefore do not qualify.
Precertification has become a complicated, long-term process often requiring a full-time staff person. Because bariatric surgical procedures are complex and associated with potentially serious complications, malpractice coverage has been increasingly difficult to obtain and very expensive. This increased overhead has driven many surgeons to drop out of HMOs and accept only patients with out-of-network coverage. These patients, however, are likely to pay a portion of the surgeon’s fee out-of-pocket.
After-surgery costs must also be considered. Nutritionist appointments are often out-of-pocket or negotiated before surgery. These can range from $50 to $100 per visit. Also, gastric bypass patients typically lose weight very fast and must be prepared to purchase new clothing. Long-term costs include lifelong nutritional supplements which can total $50/month (Obesitycoverage, 2020; PMPH, 2022).
THE ROLES OF OCCUPATIONAL AND PHYSICAL THERAPY IN BARIATRIC SURGERY
Occupational therapists provide lifestyle modification interventions to reduce weight before surgery and improve postsurgical outcomes. Occupational therapists also assist patients with occupational changes following surgery, including new habits and routines required when eating much smaller quantities of food, taking supplements, building and maintaining strength through physical activity, and social eating. Occupational therapy lifestyle interventions are also beneficial for patients who experience weight gain after the initial loss (Dieterle, 2018).
Physical therapists assist in the management of patients who are candidates for bariatric surgery. Therapists help prepare patients for the surgery and recovery by developing and instructing them in individualized preoperative and postoperative programs. Preoperatively, therapy may involve strength training and aerobic conditioning. Postoperative programs often begin with deep breathing and lower-extremity exercises to gently increase strength and aerobic conditioning. Physical therapists help to minimize pain, regain motion and strength, and return to normal activities as soon as possible (APTA, 2021).
CASE
Eric, Age 63
Eric is a 63-year-old man with type 2 diabetes who is referred by his primary care physician to the Kensington Bariatric Center for evaluation for bariatric surgery. The bariatric center is staffed by a team of obesity specialists that includes internists, registered dietitians, nurses, and a psychologist, all of whom are involved in a comprehensive evaluation of the patient.
Eric’s medical history indicates that his current medications include 70 units of NPH insulin before breakfast and 70 units before dinner, Metformin 850 mg twice a day, atorvastatin, nifedipine, aspirin, and allopurinol. He has sleep apnea but is not currently using his continuous positive airway pressure (CPAP) machine. His reported morning glucose levels are between 100–130 mg/dl, hemoglobin A1C level is 6.1% (within normal limits), and his triglyceride level is 201 mg/dl. He weighs 342 pounds, is 5 feet 6 inches tall, and has a BMI of 55.2.
Eric reports that he became obese as a child and that he has gained weight every decade since. He is currently at his highest adult weight, and there are no indications that medications or medical complications contribute to his obesity. His family history reveals that his father, two of his sisters, and one of his daughters are also obese.
Eric describes his past weight-loss to have included both commercial and supervised medical weight-loss programs. He has been unable to sustain any weight he lost on these programs after a few months of discontinuing them. He has been to weight-loss sessions with a registered dietitian and has also taken part in a hospital-based, dietitian-led, group weight-loss program, where he lost weight. But again, he regained it all. He has been on many self-directed diets throughout the years but has never lost any significant weight while on them, and whatever weight he did lose, he once again regained.
A food intake history reveals that Eric eats three meals a day, with dinner being the largest. He sometimes eats between meals, especially if there is food available at his workplace. He eats a snack before bedtime to avoid hypoglycemia. He eats in restaurants once or twice each week but does not frequent any fast-food places. He does not drink alcohol. He admits to binge eating on occasion, even when not hungry, and attributes this to stress.
Eric is a widower who recently began a new relationship. He and his girlfriend have known each other for many years, and she is normal weight. He reports that both he and his girlfriend are concerned about his weight and his diabetes, and he is now willing to consider weight-loss surgery.
Following his evaluation, it is determined that Eric meets the criteria for surgery according to current clinical guidelines because he has clinical severe obesity (BMI ≥40 with comorbid conditions), has failed with less invasive methods of weight loss, and is at high risk for obesity-associated morbidity/mortality. He is found to have no contraindications for surgery.
Eric attends an orientation session where he learns about his surgical options, is given a description of the procedures, including their risks and possible complications, and is encouraged to ask questions. He is referred to the surgeon for evaluation, and it is decided that he will pursue the Roux-en-Y gastric bypass. He is set up for a surgical date and also encouraged to lose weight before the surgery.
Eric does well after surgery, eats without difficulty, and reports feeling no hunger. At two months post surgery, his fasting and pre-dinner blood glucose levels have been consistently less than 120 mg/dl, with no other diabetes medications required.
One year following surgery, Eric’s weight is 254 pounds, a loss of 88 pounds, and he continues to lose weight at approximately 1 to 2 pounds each month. His diabetes, sleep apnea, and hypercholesterolemia are resolved, and his blood pressure is controlled.
MANAGEMENT AND TREATMENT OF OBESITY IN CHILDREN AND ADOLESCENTS
Management of obesity in children and adolescents requires family-centered communication and family-based interventions rather than those focused on the patient (child or adolescent) alone. Targeting a parent as an important agent of behavior change, either with or without the child, is more effective for long-term weight management than targeting only the child without parental participation. Any therapeutic intervention without the understanding, approval, and active participation of family members is unlikely to succeed (Skelton, 2021; Schwarz, 2020).
Effective approaches should be collaborative rather than prescriptive, with the clinician engaging the family in selecting specific behaviors to change. The child should be directly involved in decision-making as appropriate for his or her age. Any intervention is likely to fail if it does not involve active participation and support of family members. Because the child may be one of many family members who have obesity, successful treatment often requires a change in the entire family’s approach to eating. In some cases, family therapy may be advised. An intensive group therapy approach has been found to be superior to standard, family-based therapy in achieving lifestyle changes and reducing the BMI of overweight adolescents.
A team approach to management includes nurse educators, nutritionists, exercise physiologists, and counselors, as well consultations with pulmonary medicine specialists, orthopedists, and/or gastroenterologists as appropriate. In addition, any acute or chronic complications of obesity are managed and psychiatric assistance obtained for eating disorders or severe depression (Schwarz, 2020).
The Staged Approach
The staged approach to addressing obesity is determined by multiple factors, including age, BMI, and previous weight-management history. Management to address overweight or obesity is divided into stages that represent degrees of supervision, counseling, and intervention. The American Academy of Pediatrics recommends a four-stage approach to treatment of childhood obesity:
- Stage 1 (Prevention-Plus Protocol) can be implemented in primary care for children ≥2 years old with BMI ≥85th percentile, with recommendations for improving the diet, increasing physical activity, modifying family behaviors or environments, monthly follow-ups, and advancement to stage 2 if BMI does not improve in 3 to 6 months.
- Stage 2 (Structured Weight Management Protocol) for children ≥6 years old consists of more structure and supervision in a primary care office and includes stage 1 guidelines plus increased structure and education, follow-up as often as needed, and advancement to stage 3 if BMI does not improve in 3 to 6 months.
- Stage 3 (Comprehensive Multidisciplinary Intervention) for children ≥6 years old with severe obesity (BMI ≥35) can be implemented in a primary care office and includes stage 2 guidelines, increased structured dietary program, plus a multidisciplinary team and outside facilities, such as a pediatric obesity treatment clinic for structured physical activity.
- Stage 4 (Tertiary Care Intervention) is implemented if a patient has a BMI ≥95th percentile, significant comorbidities, and has not responded to stages 1 through 3, or has a BMI 99th percentile and has shown no improvement in stage 3. This is carried out in a pediatric weight management center with a multidisciplinary team with expertise in pediatric obesity, and includes stage 3 recommendations, medications, extremely structured dietary regimens, or bariatric surgery.
(Skelton, 2021; Johnson, 2021)
Lifestyle Interventions for Children and Adolescents
Research has indicated that lifestyle interventions incorporating a dietary component along with an exercise and/or behavioral therapy component are effective in treating childhood and adolescent obesity. Lifestyle modification therapy is essential for pediatric obesity treatment and should be used as the first-line therapeutic option. Many treatment programs apply strategies such as dietary modification, increasing physical activity, and behavioral changes, including self-monitoring, stimulus control, positive reinforcement, social support, and cognitive behavior therapy.
Successful pediatric obesity management requires consideration of both the patient and family’s readiness. Setting a combination of short-term attainable goals and realistic long-term goals can help with participant motivation. Identifying what internally drives patient/family motivation for behavior change is an important element in making lifestyle changes (Sease et al., 2021; Chung & Rhie, 2021).
WEIGHT-LOSS GOALS
Weight-loss goals are based on the child’s age and degree of overweight or obesity. For children and adolescents who are overweight or mildly obese, the goal of maintaining current body weight is appropriate, as this will lead to a decrease in BMI as the child grows taller. If a child is in a phase of rapid linear growth, simply slowing weight gain is more realistic and often improves weight status. For adolescents who have completed linear growth, healthy behaviors, positive body image, and a long-term goal of gradual weight reduction should be the focus.
At high degrees of obesity, however, gradual weight loss is safe and appropriate depending on the child’s age and degree of obesity. For children between 2 and 11 years with obesity as well as comorbidities, a weight loss of one pound per month is safe and of benefit, but may be difficult to achieve. For obese adolescents with comorbidities, it is considered safe to lose up to two pounds per week, although a weight loss of one to two pounds per month is usually a more realistic goal. Because is it difficult to achieve and sustain a dramatic reduction in BMI, realistic goals should emphasize gradual weight loss and maintenance rather than a rapid fall to an ideal body weight (Skelton, 2021).
DIET
There is limited evaluation and clinical evidence to support structured dietary interventions for children with obesity. These are reasonably effective in achieving short-term weight loss in a motivated patient and are safe if adequately selected and supervised. However, they have poor adherence and success rates over a longer period of time.
Rather than focusing on a specific structured diet, goals are more apt to be achieved if eating behaviors are the focus. Programs that modify family patterns of eating are most likely to be successful.
A semi-structured dietary approach aimed at encouraging children and families to select food groups of lower energy-density and decreasing portion size are best used for weight loss in children. Such an approach may include:
- Intake of five or more servings of fruits and vegetables daily
- Decreased intake of calorie-dense foods such as saturated fats, salty snacks, and high-glycemic foods such as candy
- Minimized intake of sugar-containing beverages
- Minimized eating outside the home and eating fast food in particular
- Family meals at least five times a week
- Self-regulation of food
- Eating breakfast daily
- Discouraging dieting
- Avoiding skipping meals
(Mayo Clinic, 2020b; Skelton, 2021)
It is important to note that the long-term effects remain poorly understood of a very controlled-energy diet on adolescent growth and development and subsequent reproductive function, musculoskeletal development, and intermediary metabolism. In light of these factors and problems inherent in adhering to and maintaining severe caloric restriction, very controlled-energy diets are not recommended for the great majority of children and adolescents with obesity.
In circumstances where rapid weight loss is recommended, a protein-sparing modified fast can achieve rapid weight loss in an inpatient or outpatient setting and has been successfully used in children and adolescents with obesity. A high-protein diet, however, does not reduce obese children’s desire to eat, and ratings of desire to eat significantly increase over the duration of the intervention (Schwarz, 2020).
Weight loss tools—such as ChooseMyPlate, MyPlate, and HealthyPlate—use effective visual cues to teach healthy dietary patterns, including major food groups, portion sizes, and the goal of including more fruits and vegetables.

Healthy food selection and relative portion recommendations for avoiding obesity. (Source: USDA.)
PHYSICAL ACTIVITY
Increasing child and family levels of physical activity is a key focus in obesity treatment. It has been demonstrated that lifestyle exercise programs, in connection with dietary restrictions, provide long-term weight control in children and adolescents. It is recommended that children and adolescents participate in 60 minutes or more of physical activity each day (Schwarz, 2020).
Providers can recommend a variety of options for consideration. Structured physical activity (such as sports or performance arts) may be team-based or individual, competitive or noncompetitive. Noncompetitive activities may be more appealing to some children, particularly those with more severe obesity. Less-structured activities can include recreational sports with peers or family, or self-directed physical training.
For preschool-aged children, physical activity for the most part will be unstructured, and outdoor play is particularly helpful. Providers can encourage physical activity in this age group by prescribing playground time and providing a list of local resources (such as playground locations) in addition to discouraging sedentary time. Parents can be encouraged to consider physical activity levels when making choices for daycare and after-school programs.
For older children, structured physical activity is encouraged whenever possible, such as team or individual sports, or supervised exercise sessions. Children are more likely to participate consistently in such activities since they are accountable to a coach or a leader.
Directly engaging adolescents in choosing activities to replace sedentary time is helpful, as some will enjoy engaging in sports or fitness centers, while others may not (Schwarz, 2020; Skelton, 2021).
The following are recommendations for physical activity in the management of obesity and overweight in children and adolescents:
- Limit screen time. Decrease sedentary behavior such as watching television, surfing the internet, using a tablet or smartphone, and playing video games to no more than two hours per day for children older than 2 years. Children younger than 2 should have no screen time at all.
- Emphasize activity, not exercise. Children should be moderately to vigorously active for at least an hour a day doing activities they enjoy.
(Mayo Clinic, 2020b)
DOG OWNERSHIP AND PHYSICAL ACTIVITY
Dog ownership is associated with a number of physical, mental, and emotional health benefits. Owning and caring for a dog has shown promise in increasing children’s outdoor physical activity. Among a growing body of research on the physical activity benefits of dog ownership, studies have been conducted in children that show those from dog-owning families accumulate more physical activity and are more likely to meet physical activity recommendations (Ng et al., 2021).
THE ROLE OF PHYSICAL THERAPY WITH CHILDHOOD OBESITY
The American Physical Therapy Association (2021) recommends that primary care providers involve physical therapists in the management of childhood and adolescent obesity. Physical therapists can assess a child’s risk factors for injury during exercise and evaluate and monitor a child’s increasing level of activity. Recommendations include:
- Do not rely on BMI alone. Use BMI charts that reflect demographics and tools for measuring whole-body fat mass such as waist circumference or skin-fold thickness before beginning treatment. Ideally, it is recommended that body composition be analyzed by cross-sectional imaging.
- Be aware that a child with type 2 diabetes who is receiving insulin treatment can experience hypoglycemia during exercise.
- Evaluate the child’s psychosocial barriers, which may include low self-esteem, anxiety, negative body image, or other psychological issues that can influence how a child will adhere to the plan of care.
- Measure exercise endurance capacity and muscle strength. This can be accomplished by using the 20-meter shuttle run test for endurance and the handgrip strength test and standing broad jump test for muscle strength.
- Promote weight loss by encouraging endurance exercises, whole-body exercises being the best option.
- For children over the age of 5 years, to avoid injury when there is muscle weakness, strength training is recommended under the supervision of a physical therapist to ensure the proper execution of the exercises.
Physical therapists can be very important in helping a child develop a sense of self-efficacy that can motivate them to continue exercising.
CASE
Jaime, Age 9
Jaime is a 9-year-old boy who was referred to physical therapy for help in establishing a personal fitness plan after being identified as obese during a routine BMI screening at his school. Jaime is a pleasant child who enjoys reading and playing video games during his free time. His dad drives him to and from school, and Jaime spends most of the day in the classroom. At recess, he likes to read on a bench while the other kids play. He attends gym class one day a week.
The physical therapist, Monica, conducted an initial evaluation that included Jaime’s overall health status, history of his current presenting complaint, and screening for medical red flags, as well as evaluation of pain, joint range-of-motion, manual muscle testing, bony and soft-tissue palpation, orthopedic special tests, sensation testing, postural evaluation, gait biomechanics, and static and dynamic balance testing.
Monica next met with Jaime and his parents about an appropriate long-term fitness routine that would include cardiovascular exercise, strength training, flexibility, and functionality work. Jaime looked worried at the mention of exercise. “You won’t make me play basketball, will you?” he whispered. She assured Jaime that there are plenty of exercises he can do that don’t require throwing or catching. Monica helped Jaime and his family plan an activity program designed to gradually increase his activity level to at least 60 minutes/day. His father purchased a stationary bike and a set of free weights for them to use together. Monica reviewed safe weight-lifting technique and set parameters for the appropriate amount of weight for Jaime to be lifting.
Two weeks later, Jaime reported logging 60 minutes of activity on three of seven days and at least 30 minutes on three of the remaining days. His parents also bought him new sneakers and started a daily “family workout night” after dinner, beginning with specific stretches and core strengthening exercises learned at physical therapy, followed by riding the stationary bike or swimming at the community pool. Jaime’s dad started walking to school with him instead of driving. They now log each day’s activities in order to track their progress.
After six weeks, Jaime has made the following progress toward his long-term physical fitness goals:
- A reduced BMI and an absence of weight gain since program initiation
- Reading for half of recess and playing actively with his peers during the other half
- 60 minutes of physical activity attained on 85% of days since the start of the program
Due to the consistent support of Jaime’s parents and his rapid progress toward his physical therapy goals, it is decided that Jaime need not follow up with physical therapy until one month later, at which time he may be discharged to an independent home fitness program.
Behavioral Therapy
One of the most up-to-date approaches to managing pediatric obesity is cognitive behavioral therapy (CBT). It has been suggested that CBT can be very effective for mental health problems such as depression, impulsivity, and body image distortion that may coexist with pediatric obesity. Evidence is strong for the recommendation of family-based multicomponent behavioral interventions to treat obesity in children ages 2 to 18 years old.
Common components of pediatric obesity CBT include a behavioral approach aimed at changing eating habits and physical activity through self-monitoring, and a cognitive approach aimed at changing distorted body image and help with emotion regulation.
The cognitive approach includes thinking about emotions and negative automatic thoughts related to eating habits, helping to regulate emotions, promoting problem solving to cope with high-risk situations where food control is difficult, changing self-esteem and body image, and applying cognitive strategies to prevent relapse (Weir, 2019).
MENTAL HEALTH ISSUES
Obese children endure physical complications but also experience mental health problems such as depression, attention deficit hyperactivity disorder, and eating disorders, as well as psychosocial impairments related to school adjustment, bullying, and low self-esteem.
Depression and anxiety not only decrease treatment compliance, but also negatively impact growth and development. A recent 20-year cohort study reported that childhood overweight and obesity may increase the risk for mood disorder in adulthood, making early intervention a prime consideration (Kang & Kwack, 2020).
CASE
Motivational Interviewing
Cynthia, Age 15
Cynthia is a 15-year-old African American girl who is 5 feet, 3 inches tall and weighs 180 pounds, with a BMI of 31.9. She has been referred to the local health clinic by the school nurse at Winston Senior High School because of recent weight gain. The clinic’s nurse practitioner employs Motivational Interviewing to assist adolescent patients and their families in weight-loss efforts. During the first session with the family, the nurse found both parents to be very supportive and eager to help Cynthia meet the goals agreed on with the clinic’s weight loss team.
Today is Cynthia and her parents’ second visit to the clinic, and the nurse practitioner utilizes MI in her meeting with the family.
Nurse: “Hello, Cynthia. Hello, Mr. and Mrs. Rockland. It’s good to see you all again. Tell me, how have things been going for you this past week?” (Asking an open-ended question)
Cynthia: “Oh, so, so. Mom and Dad have been after me to follow the plan, and I’m trying, but not very well, I’m afraid.” (Responding with elaboration)
Nurse: “You haven’t been completely successful sticking with the plan.” (Rephrasing)
Mom: “She’s trying, but not has hard as we think she could.”
Nurse: “You think she is not trying hard enough.” (Restating)
Mom: “Well …”
Cynthia (interrupting): “I really am trying hard, but there’s so many things that happen and get in the way!” (Emotional elaboration)
Nurse: “You sound a bit upset!” (Mirroring)
Cynthia: “I am! It’s really hard when you sit in the cafeteria and everyone else is eating the good stuff, and your lunch is a salad with a dinky piece of chicken in it!” (Elaboration)
Nurse: “It sounds like it’s hard to sit and watch others enjoying the foods you like but aren’t supposed to eat.” (Reflecting)
Dad: “I know just how she feels. I’ve been heavy all my life, and it’s very hard to give up those things you’ve always enjoyed.” (Empathizing)
Nurse: “I can certainly understand how you both feel.” (Empathizing)
Cynthia: “You know, it’s really hard. I didn’t gain any weight last summer but started gaining again when I went back to school this fall.” (Elaborating)
Nurse: “It sounds like you were successful in sticking to your diet last summer.” (Affirming)
Cynthia: “Yes, but when I went back to school, everyone around me was eating all the good things I like and can’t have.” (Elaborating)
Nurse: “You want to stick to your diet and lose weight, but you still want to enjoy the foods you like. That sounds like a dilemma to me.” (Summarizing)
Cynthia: “Yeah, that’s exactly it! But I really do want to be thinner like the other girls. I don’t want to be a fatty! I know I can do it, but sometimes it’s just so hard.” (Using “change talk”)
Nurse: “Well, let’s see. You say you want to be thin like the other girls, and at the same time, you’re saying that eating the foods you shouldn’t eat is very important to you.” (Developing and examining discrepancy)
Cynthia: “Yes, I don’t like to look the way I do, and I really want to try harder. I really do.” (Using change talk)
Nurse: “You really are strongly motivated to change and believe you can do it.” (Supporting self-efficacy)
Cynthia: “Yes, and I know Mom and Dad are really trying to help me.” (Using change talk)
Nurse: “I see. So, tell me what the three of you might do to make this wish happen.” (Finding out what the patient and family already knows)
Cynthia: “I don’t know what else I can do. I miss Taco Bell!”
Dad: “You and me both.”
Mom: “Well, I think I have a suggestion. Maybe we could all try to be more creative with the meals we make. Maybe we could explore some new recipes so your lunch is more exciting. We could start to cook together. How does that sound?” (Collaborating)
Dad: “That’s sounds like fun to me. When should we start?” (Encouraging)
Cynthia: “That does sound like fun. We’ve never cooked anything together before. Could we really do that?” (Collaborating and negotiating)
Nurse: “Would you be interested in meeting with the dietitian again to get some ideas about the foods you could make and some basic recipes?” (Asking permission, collaborating, negotiating a plan, empowering)
Cynthia: “Shall we do that, Mom and Dad? Yeah, let’s do that!” (Collaborative response)
Mom: “I would love to spend time with you in the kitchen.” (Agreeing on action plan)
Dad: “You know I like to cook, and Mom and I can share meal planning and cooking with you on alternate days of the week.” (Agreeing on action plan)
Pharmacology
The role of pharmacological therapy in the treatment of obesity in children and adolescents is limited. Although there have been some positive findings, anorectic drugs should never routinely be used for the prevention or treatment of obesity in childhood or adolescence. These agents must not be prescribed for prepubertal children until clinical studies have been performed to assess safety and efficacy. The use of medication for childhood obesity is also limited by side effects, costs, and uncertainty about their long-term safety.
Medication might be prescribed for some adolescents, but only after the patient has failed to respond to vigorous attempts to modify behavior as part of an overall weight-loss plan. However, the risks of taking prescription medications over the long term are unknown, and the medication effects on weight loss and weight maintenance for adolescents are also unknown.
Orlistat is approved by the Food and Drug Administration for the treatment of obesity in adolescents (ages ≥12 years). All adolescents who are prescribed anorectic agents should receive concurrent nutritional and family counseling and should implement a plan of regular exercise and physical activity.
Liraglutide is also approved for use in adolescents ages 12 years and older. However, its use is limited by the high frequency of gastrointestinal side effects and need for daily subcutaneous injections.
Phentermine is approved in the United States for short-term use (12 weeks) in adolescents older than age 16. Long-term study over 6 months showed modest to moderate effect on BMI, with side effects of increased heart rate and blood pressure.
Setmelanotide (Imcivree) has recently been approved for patients ages 6 years and older for weight control caused by rare genetic conditions.
Metformin, an oral diabetic medication, is helpful in children with impaired glucose tolerance or polycystic ovary syndrome, and often promotes weight loss. This medicine can usually be used in children as young as 6 years. Unfortunately, any weight loss is usually regained after stopping the medication (Skelton, 2021; Schwarz, 2020).
Surgical Procedures for Adolescents
Current data shows that bariatric surgery in adolescents is as safe and effective as bariatric surgery in adults. Bariatric surgery is effective in selected adolescents with severe obesity who fit the criteria endorsed by policy statement from the American Academy of Pediatrics. These candidate requirements include:
- Has attained final or near final adult height
- Has BMI of >40 or >35 with significant comorbidities
- Has been compliant with other treatment modalities, including lifestyle modifications and possibly pharmacotherapy
- Has a sound psychological evaluation as well as competent family support to ensure success with postsurgical changes
- Demonstrates ability to follow healthy dietary guidelines
- Has access to experienced surgeon/pediatric bariatric surgery center for long-term follow-up
Follow-up should last at least several years and include transition to an adult bariatric team over time (ASMBS, 2022a).
Contraindications include:
- Medically correctable cause of obesity
- An ongoing substance abuse problem (within the preceding year)
- Medical, psychiatric, psychosocial, or cognitive condition that prevents adherence to postoperative dietary and medication regimens or impairs decision-making capacity
- Current or planned pregnancy within 12 to 18 months of the surgery
- Concomitant eating disorders
The Roux-en-Y gastric bypass, laparoscopic adjustable gastric band, and sleeve gastrectomy are the most widely used procedures in pediatric obesity. Their use, however, is associated with subsequent nutritional deficiencies (ASMBS, 2022a).
Laparoscopic sleeve gastrectomy is the preferred technique due to is technical ease and good results. Sleeve gastrectomy has demonstrated excess weight loss and is technically less complex, with less malabsorption of specific nutrients.
The gastric bypass and laparoscopic sleeve gastrectomy both result in slightly more than a 25% weight loss over three years. Children treated with bariatric surgery also show remission of type 2 diabetes, prediabetes, abnormal kidney function, elevated blood pressure, and dyslipidemia after three years (Calcaterra et al., 2021; ASMBS, 2022a).
CARING FOR THE BARIATRIC PATIENT
Healthcare providers face a number of challenges when working with the growing number of obese patients being admitted to hospitals and other healthcare facilities. It is essential that providers understand the physiologic and mobility concerns that may hinder the patient’s capacity to adapt to the stressors of an illness as well as the safety issues for both patients and healthcare workers regarding mobilization.
Respiratory Concerns
Changes in breathing due to obesity include increased respiratory rates, increased oxygen consumption and metabolic requirements, increased work of breathing, and decreased tidal volume. Obesity has a profound effect on the physiology of breathing, leading to pulmonary compromise in a number of ways:
- Decreases in respiratory compliance due to mechanical factors such as increased weight in the thoracic cage and abdomen
- Changes in lung compliance related to the increased pulmonary blood volume
- Disproportionately high percentage of total oxygen consumption for respiratory work, even during quiet breathing, in severely obese patients related to decreased lung volumes
- Changes in the airway associated with obstructive sleep apnea, obesity hypoventilation syndrome, and respiratory failure
- Rapid patient oxygen desaturation (hypoxia) due to the decrease in residual volume
Patients with obesity are especially prone to respiratory complications, the most common being obesity-related atelectasis or pneumonia basilar atelectasis, obstructive sleep apnea, and obesity hypoventilation syndrome.
Obesity-related atelectasis or pneumonia basilar atelectasis can occur secondary to the lack of periodic deep breathing. The patient should be encouraged to mobilize and to do deep breathing in a sitting or upright position if possible.
Obstructive sleep apnea (OSA) is very common as obesity seems to increase the passive mechanical pressures, which contributes to upper airway obstruction. This results in repetitive nocturnal oxygen desaturations, fragmented sleep, and excessive daytime somnolence. OSA is commonly treated with continuous positive airway pressure (CPAP) while resting or sleeping.
Hypnotic or narcotic medications should not be administered routinely to obese patients, but if required, patients with OSA must be monitored very closely.
Obesity hypoventilation syndrome (OHS) is characterized by inadequate daytime and/or nighttime ventilation, resulting in oxygen desaturation and elevated carbon dioxide levels. Patients with OHS often develop heart failure. Acute illness or medications can exacerbate OHS, which presents as decreased level of consciousness due to hypercapnia. The most effective acute treatment is bi-level mask ventilation or bi-level positive airway pressure (BPAP).
Patient should be encouraged to practice deep breathing and coughing hourly while awake, and to use an incentive spirometer to prevent pneumonia. Lung sounds should be auscultated regularly, and the patient observed, particularly at night, for decreased oxygenation with pulse oximetry. Respiratory status is also monitored, as well as nail beds for pallor or cyanosis (AHS, 2022).
Circulation Concerns
People who are obese are more than twice as likely to develop both deep vein thrombosis (DVT) and pulmonary embolism (PE) compared to those of normal weight. The risk is even higher in patients under age 40. Obesity causes chronic inflammation and reduced fibrinolysis (breakdown of clots). Chronic inflammation is the result of less nitric oxide, a molecule that protects the endothelium and prevents cells from sticking to the endothelial surface (Taylor, 2021).
It is critical to monitor the patient’s cardiac status, with consistent and accurate vital signs using an appropriate-sized blood pressure cuff for accuracy. Assessment should include accurate weights, monitoring of edema if present, and capillary refill time of fingers and toes. The patient should be assessed regularly for signs of DVT, including redness, tenderness, or warmth of the lower extremities.
Supine positioning can be dangerous for patients with obesity and should be avoided. When the patient is lying flat, the weight of the panniculus may decrease or impair circulation to the lower extremities. Suitable positions include semi-recumbent and reverse Trendelenburg. For those able to ambulate independently or with assistance, it is recommended they walk as tolerated regularly throughout the day.
Anticlotting medications in combination with sequential compression devices should be considered unless contraindicated. The fit of compression stockings is extremely important, as those that are too small can actually create a tourniquet effect, cutting off circulation in the patient’s lower extremities (AHS, 2022).
Skin Integrity
Because of excess body weight, obese patients are predisposed to impairment of skin integrity. Factors that contribute to this include challenges in performing a skin assessment due to difficulty moving and turning the patient, and the presence of comorbid conditions such as diabetes, peripheral vascular disease, malnutrition, and lymphedema. Those with obesity may also be at higher risk for skin breakdown related to increased sweating and moisture, possible impaired mobility, increased pressure, and increased shearing during movement.
Adipose tissue has poor blood supply, which leads to inadequate circulation and decreased oxygenation, making the skin vulnerable to breakdown, slower healing, and risk of infections. Potential venous insufficiency can further impair tissue oxygenation.
Increased body size generates more heat, and the body perspires to maintain normal temperature. Excessive sweating increases risk for bacterial and fungal infections in skin folds, especially under breasts and in groin areas.
Skin fold problems occur when there is skin-to-skin contact in which a warm, moist, and dark environment is created, which then increases the potential for skin breakdown, skin-to-skin friction and shear, irritation, rashes, candidiasis, viral or bacterial infection, and potential pressure injuries.
Focus should be on the elimination of skin-to-skin contact without causing harm to fragile tissue and on keeping skin folds dry. It is helpful to seek the patient’s input, as they have the most experience in dealing with these skin integrity challenges.
Routine examination of all skin surfaces and skin folds should be done daily and increased to every shift if skin is at high risk for breakdown. A validated tool such as the Braden Scale is recommended for skin assessment.
Deep skin folds must be closely monitored, dried thoroughly, and kept open to air as much as possible. Soft, moisture-wicking cloths (such as moisture-wicking textile with antimicrobial silver) between skin folds and antimicrobial and fungus-inhibiting powders are also recommended. The use of cornstarch is not recommended, as is often used in home remedies, since it is a substrate for the growth of yeasts.
Patients with obesity are also at higher risk for pressure injuries, which may include atypical injury, such as that between skin folds, or under the panniculus. Inspect the skin at least daily for signs of pressure injury, especially non-blanchable erythema. When inspecting darkly pigmented skin, look for changes in skin tone, temperature, and tissue consistency compared to skin in other areas of the body.
Turn and reposition frequently while in bed and include repositioning when the patient is up in a chair. Identify any equipment needs such as a trapeze to assist with position changes, as well as pressure-relieving devices (AHS, 2022).
Wound Healing
Would healing depends on the circulatory system to provide oxygen and nutrients to damaged tissue. For patients with obesity, adipose tissue is poorly vascularized, and impaired chest expansion results in potential poor oxygenation. The presence of diabetes can further contribute to delayed healing and infections. All phases of wound healing are dependent on adequate supplies of protein, carbohydrates, vitamins, and minerals. Poor nutritional intake can lead to impaired wound healing (AHS, 2022).
General Hygiene and Toileting
Bariatric patients often require access to walk-in bathing facilities, hand-held showerheads, and appropriate-sized shower chairs. Long-handled, soft-bristled shower brushes allow the patient to reach all body areas. Inspection of the skin is done during bathing to determine care needs and interventions.
More frequent bathing will be required by patients who are prone to odor problems. Odor may be caused by factors including incontinence, skin infections, wounds, skin-on-skin contact, and perspiration. Products to manage moisture and odor can be placed in skin folds.
Toileting concerns for the bariatric patient include access to adequate facilities, limited reach for cleansing, and urgency and incontinence due to tissue compression causing sphincter dysfunction. Appropriate facilities include a toilet riser with handrails for support or a bariatric commode.
All genders are challenged in maintaining genital or perineal care, particularly those who are menstruating. Cleaning and drying the genital area thoroughly and applying barrier products after incontinent episodes are recommended.
Rather than using regular toilet tissue, washcloths or premoistened wipes may be employed. Occupational therapy may be consulted for assistance in obtaining an appropriate tool to assist in reaching areas requiring cleansing (Earlam & Woods, 2020).
Medications
Standard medication dosing is based on data for ideal-weight persons. Understanding of obesity-related changes in drug pharmacology in addition to the overall safety and efficacy is limited, as clinical trials rarely focus specifically on this population.
Due to pharmacokinetic and pharmacodynamic variations associated with obesity, a clinical pharmacist is an essential member of the care team in order to determine correct dosages for the bariatric patient. Differences in the proportion of adipose and lean muscle mass and fluid status can affect absorption, distribution, metabolism, and excretion of drugs.
When administering medications, the following are taken into consideration regarding absorption:
- Increased rate of absorption of oral medications can occur due to increased gastric emptying.
- Intravenous access can be difficult.
- Decreased subcutaneous absorption can occur due to poor subcutaneous blood supply.
- Intramuscular administration may fail if needles are too short.
When monitoring medications being taken by obese patients, clinicians must also recognize certain differences in patients who are obese.
Distribution is affected by:
- Ratio of adipose tissue to lean body mass, if lipid-soluble
- Accumulation of lipophilic drugs in fat stores, requiring increased dose to gain effect
- Total body water, which may be increased by resuscitation volume
- Altered protein binding
- Reduced peak serum concentration
Metabolism is affected by:
- Critical illness with increase for drug interactions
- Reduced hepatic blood flow
Elimination is affected by:
- Increased half-life of lipid-soluble drugs due to accumulation
- Increased glomerular filtration rates
- Coexisting disease related to diabetes and hypertension
- Calculated and measured creatinine clearance, which correlate poorly in obesity and critical illness
Almost any class of drug can be affected by the physiologic changes that occur with obesity, but drugs with narrow therapeutic indexes require the most attention. Antibiotics, chemotherapeutic agents, analgesics, anticoagulants, and anticonvulsants are affected by volume and clearance anomalies. It can therefore be challenging to ensure safe therapeutic concentrations for many drugs in these classes (AHS, 2022; Martin, 2019).
Mobility and Safety
Most patients with obesity are at risk for complications related to immobility, and the patient is more at risk of developing these during a long hospitalization. These may include muscle atrophy, constipation, urinary stasis, DVT, atelectasis, pneumonia, pain management problems, cardiac deconditioning, skin breakdown, and depression.
Maintaining an obese patient’s mobility and safe patient handling pose unique challenges. Patient care areas require equipment designed for obese patients. This includes adequate weight-bearing beds, toilets, specialized chairs, and wheelchairs. Obese patients may require assistance to transfer out of bed and with ambulation. Care may require additional personnel, proper lifting equipment (such as a ceiling-mounted or portable lift to help reduce the risk of injury to staff), and a standard protocol on the methods of care and use of the equipment.
Lack of appropriate equipment, lack of staff knowledge, and shortage of adequate numbers of caregivers may all be barriers to patient mobility, which increases the complications related to immobility. It is recommended that all staff involved with lifting and transferring patients be knowledgeable and competent to safely transfer patients with bariatric care needs. There is also consensus among patient handling professionals that the goal of safe patient-handling programs should be to eliminate all manual lifting whenever possible.
Patients with obesity experience a higher fall rate than the rest of the population. Factors contributing to this include body-weight distribution, gait disturbance, and overestimation of functional status by the patient. It is important to assess the patient’s ambulation status at least once per day or more often as needed, as the ability of a patient to move in bed, get up and get out of bed, and walk about within and outside of the room can vary. It is also essential to support mobility by providing pain management (Ewens et al., 2022; AHS, 2022).
GENERAL STRATEGIES FOR OVERWEIGHT AND OBESITY PREVENTION AND ADVOCACY
Every healthcare professional has the opportunity to guide their patients toward making healthy lifestyle choices. Healthcare providers can be role models and bring their knowledge and standing to advocate for healthy changes that connect with people well beyond the healthcare facility they are working in. Every healthcare professional must have the skills to counsel patients about obesity prevention.
Recommendations are provided below for healthcare professionals working with various patient populations in various specialties.
Primary Care Practices
The following recommendations have been made for adults in primary care:
- Measure BMI in all adult patients.
- Order appropriate follow-up laboratory tests for patients who are overweight and obese.
- Prescribe a long-term treatment strategy that may include:
- Counseling, coaching, or behavioral interventions on diet and lifestyle change
- Weight-loss medication for appropriate patients who have been unable to lose weight using conventional therapy and who have no contraindications
- Bariatric surgery for those individuals with severe obesity unable to lose weight through conventional therapy and who have no contraindications
-
Design offices to avoid stigmatizing overweight or obese individuals, such as providing private weighing areas and using scales that can measure weights greater than 300 pounds.
(Harvard T.H. Chan, 2022d)
Pediatric Care Practices
The newest research in children indicates that healthcare interventions in a clinic or office setting in the absence of broader community strategies to prevent obesity may lead to behavior change but may not be adequate to result in sizable improvements in weight. It is therefore recommended that clinic efforts be combined with communitywide changes, such as the “Collaborate for Healthy Weight” initiative. For all children seen in pediatric offices, recommendations include:
- Measure BMI-percentile-for-age at every well-child visit for children ages 2 years and older; measure weight-for-length percentile for children under 2 years.
- Counsel all patients and families on healthy eating, physical activity, and healthy growth, regardless of current weight status.
- Counsel all patients and families to limit television time to no more than two hours per day and to remove televisions from children’s bedrooms.
- Counsel all patients and families to limit consumption of sugar-sweetened beverages.
- Counsel all patients and families to help children achieve 60 minutes of moderate to vigorous physical activity per day.
- Establish procedures for follow-up assessment (including laboratory tests), counseling, and treatment plans for children who are overweight or obese.
- Establish policies to avoid weight bias in pediatric clinics, which may include requiring all employees to be trained on weight-bias prevention.
(Skelton, 2021; Harvard T.H. Chan, 2022d)
Obstetrical Care Practices
There are many factors before and during pregnancy that can affect a child’s obesity risk later in life. The following recommendations pertain to obstetrical care practices:
- Counsel patients on the importance of having a healthy weight before pregnancy and gaining weight at a healthy rate during pregnancy (15–25 pounds for overweight women, 11–20 pounds for obese women).
- Early ultrasound evaluation should be performed to establish gestational age and to determine whether there is a multifetal gestation.
- Recommend that mothers breastfeed their babies and provide support and training for breastfeeding.
- Counsel patients on the importance of discontinuing smoking during pregnancy.
- Screen pregnant women for gestational diabetes.
- Counsel patients on primary weight-management strategies during pregnancy, including dietary control, exercise, and behavior modification. Working with a nutritionist can help patients plan meals for optimum health gestational weight gain.
- Almost all drugs prescribed for weight reduction have adverse fetal effects and should not be used during pregnancy.
- If pregnancy occurs before the recommended timeframe for women who have had bariatric surgery, closer surveillance of maternal weight and nutritional status as well as serial monitoring of fetal growth will be beneficial.
(Palaszewski, 2021; Harvard T.H. Chan, 2022d)
Hospital and Clinic Efforts
The following are recommendations for helping in the prevention of obesity in hospital settings:
- Encourage healthcare providers to model healthy eating.
- Offer healthy foods and beverages to employees and patients.
- Ban the sale and marketing of unhealthy foods and beverages on clinic and hospital premises.
- Promote breastfeeding among new mothers who give birth in the hospital or clinic, as well as for hospital and clinic employees who are nursing.
(Harvard T.H. Chan, 2022d)
Health Insurance Providers
Recommendations put forth to insurance providers include advocating for the following:
- Cover obesity-related services that include assessment, prevention, evaluation, treatment, and follow-up, and streamline reimbursement procedures.
- Create and promote prevention programs that can be instituted plan wide.
- Provide subscribers with incentives for maintaining healthy body weight or adopting healthy behaviors.
- Measure and track progress in BMI screening through Healthcare Effectiveness Data and Information Set (HEDIS) data collection.
- Fund obesity prevention efforts in the community and/or participate in community obesity prevention coalitions.
(Harvard T.H. Chan, 2022d)
Individual Healthcare Professionals
Each healthcare professional can serve as a leader and role model—both within one’s area of practice and in the community—to encourage healthy behaviors and to make changes in the built environment. Professionals can advocate at professional organizations, local, state, and federal levels for policy and built environment changes promoting healthy eating and physical activity in healthcare settings, childcare settings, schools, after-school programs, and communities. Healthcare professionals can encourage parents to advocate for changes in the environment that promote physical activity in their children’s schools and communities (Harvard T.H. Chan, 2022d).
Ending Weight Stigma in Healthcare
Substantial evidence demonstrates the widespread experiences and impact of weight stigma that is ultimately leading to inequitable healthcare for those living with obesity. The overwhelming evidence that such weight stigma in healthcare is detrimental must be addressed. Aligned with the WHO call for zero discrimination in healthcare, there is a need for:
- Treating all patients, no matter their background or appearance, with respect and dignity
- Ensuring that everyone has equal opportunity to access quality care in a timely fashion
- Developing education resources about the complexity of obesity and the impact of weight stigma for both current and future healthcare professionals
- Addressing the stigmatizing framing of obesity policies and campaigns to remove fear, frustration, pessimism, and blaming
(Flint, 2021)
Barriers to the Provision of Weight Management in Primary Care Clinics
The current outcomes of obesity treatment indicate a failure of both patients and physicians in initiating or maintaining interventions. Recent studies have been done to identify and understand the barriers to obesity management in clinical settings from the points of view of both patients and healthcare providers.
Healthcare provider factors:
- Healthcare providers (HCPs) cite limited appointment time for patient visits as the principal reason for not discussing weight management with their patients.
- Insufficient training and counseling skills for obesity make is difficult for HCPs to provide counseling for obesity. Obesity education for HCPs includes diverse fields such as diet, nutrition, exercise, behavior therapy, and medication. Medical schools are urged to adequately address obesity education in their curricula.
- Despite its recognition as a chronic disease, obesity is underdiagnosed. HCPs must proactively screen for obesity and initiate discussions in obesity management. A survey indicates that 55% of patients with obesity received a formal diagnosis, 38% discussed a weight-loss plan with their provider, and 24% were scheduled for a follow-up appointment.
(Kim, 2020: Weller, 2021)
Patient factors:
- Awareness. Obesity is not recognized as a chronic and relapsing disease.
- Misbelief and misinformation. Rather than seeking advice from HCPs, individuals use alternative sources of information such as the internet, family and friends, television, and smartphone applications.
- Environmental factors. Successful weight loss may depend on family functioning or finding a support system within and/or outside the family. Successful adherence to long-term lifestyle changes requires a strong support network.
- Cost, particularly for patients with low socioeconomic status. Obstacles include the higher cost of healthy foods and financial inability to take part in weight-loss programs or to use an exercise facility. Unlike medical treatments for other chronic disease, obesity medications are generally not reimbursed by healthcare systems.
(Kim, 2020)
CONCLUSION
Obesity around the world and in the United States continues to be a major problem. Researchers have learned a great deal over the past several years about the pathogenesis and contributing factors involved in the development of obesity, and as a result, have a much better understanding of this chronic disease. However, despite these efforts, the problem persists and continues to grow.
Of great concern is the need for healthcare providers to become aware of their own biases and the socially accepted stigma surrounding overweight and obesity, much as those efforts were and are continuing to be made regarding issues of mental health. Overweight and obesity require healthcare professionals to take an active role in the prevention of obesity and treatment for those who live with this disease, and to learn that compassion, empathy, and patience are necessary to become a positive force against this modern public health concern.
RESOURCES
Adult obesity facts (CDC)
BMI calculator (U.S. DHHS)
Childhood obesity facts (CDC)
Institute for Healthy Childhood Weight (American Academy of Pediatrics)
Pediatric growth charts (CDC)
REFERENCES
NOTE: Complete URLs for references retrieved from online sources are provided in the PDF of this course.
Alahmadi R. (2019). The effects of parenting style and feeding style on child weight status: a systematic review. Masters Theses, 4427. The Keep: Institutional Repository of Eastern Illinois University. https://thekeep.eiu.edu
Alam I, Negara J, & Zelphira F. (2020). Effects of obesity on cognitive function., Advances in Health Sciences Research, 21, 273–5. https://doi.org/10.2991/ahsr.k.200214.072
Alberta Health Services (AHS). (2022). Guidelines for the care of hospitalized patients with bariatric care needs. https://www.albertahealthservices.ca
Amato A, Wheeler H, & Blumberg B. (2021). Obesity and endocrine-disrupting chemicals. Endocrine Connections, 10(2), R87–105. https://doi.org/10.1530/EC-20-0578
American Academy of Orthopaedic Surgeons (AAOS). (2019). The impact of childhood obesity on bone, joint, and muscle health. OrthoInfo. https://orthoinfo.aaos.org
American Association for Clinical Chemistry (AACC). (2022). Lipid profile. Testing.com. https://www.testing.com
American Association of Clinical Endocrinologists. (AACE). (n.d.). What is the disease of obesity? Clinical evaluation. https://slideplayer.com
American Medical Association (AMA). (2013). Reports of the council on science and public health. https://www.ama-assn.org
American Occupational Therapy Association (AOTA). (2015). Occupational therapy’s role in bariatric care. https://www.aota.org
American Physical Therapy Association (APTA). (2021). Physical therapist’s guide to obesity. https://www.choosept.com
American Society for Metabolic and Bariatric Surgery (ASMBS). (2022a). Who is a candidate for bariatric surgery? https://asmbs.org
American Society for Metabolic and Bariatric Surgery (ASMBS). (2022b). Childhood and adolescent obesity. https://asmbs.org
American Society for Metabolic and Bariatric Surgery (ASMBS). (2021a). The impact of obesity on your body and health. https://asmbs.org
American Society for Metabolic and Bariatric Surgery (ASMBS). (2021b). Bariatric surgery procedures. https://asmbs.org
American Society for Metabolic and Bariatric Surgery (ASMBS). (2020). Benefits of weight loss surgery. https://asmbs.org
American Thyroid Association (ATA). (2022). Thyroid and weight. https://www.thyroid.org
Anderson L. (2021). Side effects of weight loss drugs (diet pills). https://www.drugs.com
Apple R. (1987). Mothers and medicine: a social history of infant feeding, 1890–1950. University of Wisconsin Press.
Arakelyan H. (2020). Casomorphin. https://www.researchgate.net
Au L, Zhu S, Plank K, Frongillo E, Laraia B, Gurzo K, & Ritchie L. (2019). Household food insecurity is associated with higher adiposity among US school children ages 10–15 years: the Healthy Communities Study. Journal of Nutrition, 149(9), 1642–50. https://doi.org/10.1093/jn/nxz108
Balasubramanian P, Kiss T, Tarantini S, et al. (2021). Obesity-induced cognitive impairment in older adults: a microvascular perspective. Heart and Circulator physiology, 320(2), H740–61. https://doi.org/10.1152/ajpheart.00736.2020
Barros W, da Silva K, Silva R, et al. (2022). Effects of overweight/obesity on motor performance in children: a systematic review. Front Endocrinol, 12. doi:10.3389/fendo.2021.759165
Barber N. (2020). Food marketing to children. https://btugman.pressbooks.com
Blanco-Gandia M, Gonzales-Portilla M, & Rodriguez-Arias M. (2020). Diet, drugs, and the brain: are ultra-processed foods a gateway to addiction? Mètode science journal, 11, 139–45. https://doi.org/10.7203/metode.11.16195
Bleistein A. (2022). From the Obesity Medicine Association: the alarming link between screen time and pediatric obesity. https://www.physiciansweekly.com
Brennan D. (2021a). What to know about obesogens. WebMD. https://www.webmd.com
Brennan D. (2021b). What is Pickwickian syndrome? WebMD. https://www.webmd.com
Burridge K, Christensen S, Golden A, et al. (2022). Obesity history, physical exam, laboratory, body composition, and energy expenditure: an Obesity Medicine Association (OMA) clinical practice statement 2022. Obesity Pillars, 1, 100007. https://doi.org/10.1016/j.obpill.100004
Calcaterra V, Cena H, Pelizzo G, Porri D, et al. (2021). Bariatric surgery in adolescents: to do or not to do. Children (Basel), 8(6). doi:10.3390/children8060453
Cardiff E. (2021). Addictive ingredients in fast food and their effect on your body. https://www.onegreenplanet.org
Centers for Disease Control and Prevention. (CDC). (2021a). Adult obesity facts. https://www.cdc.gov
Centers for Disease Control and Prevention (CDC). (2021b). Obesity, race/ethnicity, and COVID-19. https://www.cdc.gov
Centers for Disease Control and Prevention (CDC). (2021c). Adult obesity prevalence maps. https://www.cdc.gov
Centers for Disease Control and Prevention. (CDC). (2021d). Breastfeeding report card. https://www.cdc.gov
Centers for Disease Control and Prevention (CDC). (2021e). Adult obesity causes & consequences. https://www.cdc.gov
Centers for Disease Control and Prevention (CDC). (2021f). About adult BMI. https://www.cdc.gov
Centers for Disease Control and Prevention (CDC). (2021g). About child and teen BMI. https://www.cdc.gov
Centers for Disease Control and Prevention (CDC). (2020). How much physical activity do adults need? https://www.cdc.gov
Centers for Disease Control and Prevention (CDC). (2019). Physical activity guidelines for school-aged children and adolescents. https://www.cdc.gov
Chatham R & Mixer S. (2019). Cultural influences on childhood obesity in ethnic minorities: a qualitative systematic review. J Transcult Nurs, 31(1), 87–99. doi:10.1177/1043659619869428
Chen B. (2020). Parenting styles, parenting practices, and dietary intakes of preschoolers and their parents. https://openprairie.sdstate.edu
Chung Y & Rhie Y. (2021). Severe obesity in children and adolescents: metabolic effects, assessment and treatment. J. Obes Metab Syndr. 30(4), 326–35.
Clark C. (2021). Is cheese addictive? Say “cheese” if you’re wondering. https://greatist.com
Cleveland Clinic. (2022). Is BMI an accurate measure of health? https://health.clevelandclinic.org
Cleveland Clinic. (2021). Why are certain foods so addictive? https://health.clevelandclinic.org
Damme A. (2019). Weight status, bullying involvements, and internalizing symptomology in adolescents: examining a diathesis-stress model. https://digitalcommons.unl.edu/
Dieterle C. (2018). Managing obesity in adults: a role for occupational therapy. https://www.aota.org
Earlam A & Woods L. (2020). Obesity: skin issues and skinfold management. https://www.myamericannurse.com
Egusquiza R & Blumberg B. (2020). Environmental obesogens and their impact on susceptibility to obesity: new mechanisms and chemicals. Endocrinology, 161(3). https://doi.org/10.1210/endocr/bqaa024
Elhussiney D & Mahfouz E. (2020). Obesity, environment and work ability: the risk, the link and opportunity. https://www.researchgate.net
Environmental Protection Agency (EPA). (2021a). Types of pesticide ingredients. https://www.epa.gov
Environmental Protection Agency (EPA). (2021b). Polychlorinated biphenyls (PCBs). https://www.epa.gov
Ewens B, Kemp V, Towell-Barnard A, & Whitehead L. (2022). The nursing care of people with class III obesity in an acute care setting: a scoping review. BMC Nurs, 21, 33. https://doi.org/10.1186/s12912-021-00760-7
Falbe J, Thompson H, Patel A, & Madsen K. (2019). Potentially addictive properties of sugar-sweetened beverages among adolescents. Appetite, 133, 130–7. https://doi.org/10.1016/j.appet.2018.10.032
Flint SW. (2021). Time to end weight stigma in healthcare. EClinicalMedicine, 34, 100810. doi:10.1016/j.eclinm.2021.100810. PMID: 33870153; PMCID: PMC8042345.
Flores-Dorantes M, Díaz-López Y, & Gutiérrez-Aguilar (2020). Environment and gene association with obesity and their impact on neurodegenerative and Neurodevelopmental diseases. Front. Neurosc., 14, 863. doi:10.3389/fnins.2020.00863
Folkvord F & Hermans R. (2020). Food marketing in an obesogenic environment: a narrative overview of the potential of healthy food promotion to children and adults. Curr Addict Rep, 7, 431–6. https://doi.org/10.1007/s40429-020-00338-4
Fox-Rawlings. (2022). PCBs are still causing harm decades after ban. https://www.center4research.org
Fulton M & Srinivasan V. (2021). Obesity, stigma and discrimination. StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov
Gale L. (2019). Obesity in a culturally diverse population: an overview—providing culturally competent care. https://www.ebsco.com
George Washington University (GWU). (2019). Accelerated risk of mobility loss for people aged 60+ tied to excess weight/inactivity. https://www.sciencedaily.com
Ghosal A, Ghosal A, & Ghosal S. (2021). Cognition, brain function and plasticity in the overweight and obese—a review. J. Diabetes Metab Disord, 8, 040. doi:10.24966/DMD-201X/100040
Hamdy O. (2022). Obesity. Medscape. https://emedicine.medscape.com
Harvard Medical School. (HMS). (2021). Calories burned in 30 minutes for people of three different weights. https://www.health.harvard.edu
Harvard T.H. Chan School of Public Health. (2022a). Prenatal and early life influences. https://www.hsph.harvard.edu
Harvard T.H. Chan School of Public Health. (2022b). Sleep. https://www.hsph.harvard.edu
Harvard T.H. Chan School of Public Health. (2022c). Physical activity. https://www.hsph.harvard.edu
Harvard T.H. Chan School of Public Health. (2022d). Healthcare obesity prevention recommendations: complete list. Retrieved from: https://www.hsph.harvard.edu
Hayden M, Dixon M, Dixon J, Playfair J, & O’Brien P. (2010). Perceived discrimination and stigmatisation against severely obese women: age and weight loss make a difference. Obes Facts, 3, 7–14. doi:1159/00027320
Hollis J & Robinson S. (2022). Prenatal experience and childhood obesity. https://ebook.ecog-obesity.eu
House S, Joseph R, Puro N, & Burke D. (2019). Use of technology in the management of obesity: A literature review. Perspective in Health Information Management, 16, 1c.
Hulsegge G, Mechelen W, Paagman H, et al. (2020). The moderating role of lifestyle, age, and year working in shifts in the relationship between shift work and being overweight. Int Arch Occup Environ Health, 93, 697–705. https://doi.org/10.1007/s00420-020-01519
Ingersoll K. (2022). Motivational interviewing for substance use disorders. UpToDate. https://www.uptodate.com
Jenull B, Mayer C, Knobel P, & Birnbacher R. (2021). Weight-stigma and body satisfaction among preschool children. Journal of Pediatrics, Perinatology and Child Health, 5, 112–25.
Johns Hopkins Medicine. (2022). Intermittent fasting: what is it, and how does it work? https://www.hopkinsmedicine.org
Johnson S. (2021). Pediatric obesity: prevention, assessment and treatment in primary care. https://idun.augsburg.edu
Kaczynski A, Eberth J, Stowe E, Wende M, Liese A, et al. (2020). Development of a national childhood obesogenic environment index in the United States: differences by region and rurality. Int J Behav Nutr Phys Act, 17, 83. http://doi.org/10.1186/s12966-020-00984-x
Kang N & Kwack Y. (2020). An update on mental health problems and cognitive behavioral therapy in pediatric obesity. Pediatr Gastroenterol Hepatol Nutr, 23(1), 15–25. doi:10.5223/pghn.2020.23.1.15
Kansra A, Lakkunarajah S, & Jay S. (2021). Childhood and adolescent obesity: a review. Front Pediatr, 8, 581461. doi:10.3389/fped.2020.581461
Khana D & Rehman A. (2022). Pathophysiology of obesity. StatPearls Publishing, http://ncbi.nim.gov
Kim T. (2020). Barriers to obesity management: patient and physician factors. J Obes Metab Sundr, 29(4), 244–7. doi:10.7570/jomes20214
Klish W. (2020). Clinical evaluation of the obese child and adolescent. UpToDate. https://www.uptodate.com
Knight S, Laird E, Williamson W, O’Connor J, et al. (2021). Obesity is associated with reduced cerebral blood flow modified by physical activity. Neurobiology of Aging, 105, 35–47. http://doi.org/10.1016/j.neurobiolaging.2021.04.008
Lam T, Vaartjes I, Grobbee D, Karssenberg D, & Lakervelt J. (2021). Associations between the built environment and obesity: An umbrella review. Int J Health Geogr, 20(7). https://doi.org/10.1186/s12942-021-00260-6
LaMorte W. (2019). The transtheoretical model (stages of change). http://sphweb.bumc.bu.edu
Lange D. (2021). Physical activity—statistics & facts. https://www.statista.com
Lee K, Arriola-Sanchez L, Lumeng J, et al. (2021). Weight stigma by association among parents of children with obesity: a randomized trial. Academic Pediatrics, (22)5. https://doi.org/10.1016/j.acap.2021.09.019
Li Y, Lin S, & Chiang, T. (2020). Timing of rapid weight gain and its effect on subsequent overweight or obesity in childhood: findings from a longitudinal birth cohort study. BMC Pediatr, 20, 293. https://doi.org/10.1186/s12887-020-02184-9
Lim R. (2022). Bariatric surgery for management of obesity: indications and preoperative preparation. UpToDate. https://www.uptodate.com
Long G, Sadeghirad B, Ball G, da Costa B, et al. (2020). Comparison of dietary macronutrient patterns of 14 popular named dietary programs for weight and cardiovascular risk factor reduction in adults: systematic review and network meta-analysis of randomized trials. BMJ, 369, 696. http://dx.doi.org/10.1136/bmj.m696
Luo S, Angelo B, Chow T, Monterosso J, et al. (2021). Associations between exposure to gestational diabetes mellitus in utero and daily energy intake, brain responses to food cues, and adiposity in children. Diabetes Care, 44(5), 1185–93. https://doi.org/10.2337/dc20-3006
Lutz J. (2020). Obesity and inflammation: a vicious cycle. https://www.endocrineweb.com
Martin C. (2019). The impact of obesity on drug dosing. Pharmacy Purchasing & Products. https://www.pppmag.com
Martinelli LA. (2022). Stakeholders and ethics in healthcare: ethical accountability for organizations. Routledge. https://www.google.com
Mattoo T. (2021). Patient education: high blood pressure in children (beyond the basics). UpToDate. https://www.uptodate.com
Mayo Clinic. (2021a). Cushing syndrome. https://www.mayoclinic.org
Mayo Clinic. (2021b). The Mayo Clinic diets: a weight-loss program for life. https://www.mayoclinic.org
Mayo Clinic. (2020a). Prescription weight-loss drugs. https://www.mayoclinic.org
Mayo Clinic. (2020b). Childhood obesity. https://www.mayoclinic.org
Mazurak N, Cook J, Weiland A, Ritze Y, et al. (2021). Impact of childhood obesity and psychological factors on sleep. Front Psychiatry, 12. doi:10.3389/psyf/2021.657322
McDonald’s. (2022). World famous fries. https://www.mcdonalds.com
MDApp. (2020). Relative fat mass (RFM) calculator. https://www.mdapp.co
Milken Institute. (2020). Weighing down America: 2020 update. https://milkeninstitute.org
Mohiuddin A. (2020). Fast food addiction: a major public health issues. Archives in Biomedical Engineering & Biotechnology - ABEB. https://irispublishers.com
Monteiro C, Cannon G, Lawrence M, Costa Louzada M, & Pereira Machado P. (2019). Ultra-processed foods, diet quality, and health using the NOVA classification system. FAO. https://www.fao.org
Monteiro C & Jaime P. (2020). Brazilian food guide attacked: now, overwhelming support for the guide in Brazil and worldwide. World Nutrition, 11(4), 94–9.
Morin A. (2022). The effects of caffeine on teenagers. https://www.verywellhealth.com
Motivational Interviewing Network of Trainers (MINT). (2021). Understanding Motivational Interviewing. http://www.motivationalinterviewing.org
Myers S, Govindarajulu U, Joseph M, & Landsbergis P. (2021). Work characteristics, body mass index, and risk of obesity: the National Quality of Work Life Survey. Annals of Work Exposures and Health, 65(3), 291–306. https://doi.org/10.1093/annweh/wxaa098
National Institute of Environmental Health Sciences (NIEHS). (2021a). Obesity. https://www.niehs.nih.gov
National Institute of Environmental Health Sciences (NIEHS). (2021b). Flame retardants. https://www.niehs.nih.gov
National Institute of Environmental Health Sciences (NIEHS). (2021c). All about phthalates. https://www.niehs.nih.gov
National Institutes of Health (NIH). (2021a). Randomized controlled trial of fecal microbiota transplantation in severe obesity (RCTFMTOb). https://clinicaltrials.gov
National Institutes of Health (NIH). (2021b). Screen time and children. https://medlineplus.gov
National Institutes of Health (NIH). (2021c). Circadian rhythms. https://www.nigms.nih.gov
National Institutes of Health (NIH). (2020). Types of bariatric surgery. https://www.niddk.nih.gov
National Sleep Foundation (NSF). (2020a). How much sleep do you really need? https://www.thensf.org
National Sleep Foundation (NSF). (2020b). Understanding the circadian rhythm. https://www.thensf.org/
Nedea D. (2020). Relative fat mass explained/relative fat mass (RFM) calculator. https://www.mdapp.co
Ng M, Wenden E, Lester L, Westgarth C, & Christian H. (2021). A study protocol for a randomized controlled trial to evaluate the effectiveness of a dog-facilitated physical activity minimal intervention on young children’s physical activity, health and development: the PLAYCE PAWS trial. BMC, 21, 51. https://doi.org/10.1186/s12889-020-10034-7
Obesity Action Coalition (OAC). (2018). Understanding obesity stigma brochure. https://www.obesityaction.org
Obesitycoverage. (2020). Average cost of gastric bypass surgery. https://www.obesitycoverage.com
Obesity Evidence Hub (OEH). (2021).Impact of unhealthy food marketing on children. https://www.obesityevidencehub.org.au
Obesity Medicine Association. (2021). What is obesity. https://obesitymedicine.org
Office of Disease Prevention and Health Promotion (ODPHP). (2022). Access to foods that support healthy eating patterns. https://www.healthypeople.gov
Oh R, Gilani B, & Uppaluri K. (2021). Low carbohydrate diet. StatPearls Publishing. https://www.ncbi.nlm.nih.gov
Olmo, Butler M, & Barrientos R. (2021). Evolution of the human diet and its impact on gut microbiota, immune responses, and brain health. Nutrients, 13, 196. https://doi.org/10.3390/nu1310196
Olsthoorn L, Vreeken D, & Kiliaan A. (2021). Gut microbiome, inflammation, and cerebrovascular function: link between obesity and cognition. Front. Neurosci, 15, article 761456. doi:10.3389/fnins.2021.76145
OSF HealthCare. (2020). Screen time for kids: how much is too much? https://newsroom.osfhealthcare.org
Palaszewski D. (2021). Obesity and pregnancy. Medscape. https://emedicine.medscape.com
Palmer C. (2021a). The link between gut health and obesity. https://www.goodrx.com
Patte K, Livermore M, Qian W, & Leatherdale S. (2021). Do weight perception and bullying victimization account for links between weight status and mental health among adolescents? BMC Public Health, 21, 1062. https://doi.org/10.1186/s12889-021-11037-8
Penn Medicine Princeton Health (PMPH). (2022). Digging deeper: insurance for bariatric surgery. https://www.princetonhcs.org
Perreault L. (2022). Obesity in adults: drug therapy. UpToDate. https://www.uptodate.com
Perreault L. (2021a). Determining body composition in adults. UpToDate. https://www.uptodate.com
Perreault L. (2021b). Obesity in adults: prevalence, screening and evaluation. UpToDate. https://www.uptodate.com
Perreault L & Apovian C. (2021). Obesity in adults: overview of management. UpToDate. https://www.uptodate.com
Perreault L & Bessesen D. (2021). Obesity in adults: etiologies and risk factors. UpToDate. https://www.uptodate.com
Perreault L & Burgermaster M. (2020). Behavioral therapy. UpToDate. https://www.uptodate.com
Perreault L & Delahanty L. (2021). Obesity in adults: dietary therapy. UpToDate. https://www.uptodate.com
Perreault L & Laferrère B. (2020). Overweight and obesity in adults: health consequences. UpToDate. https://www.uptodate.com
Perreault L & Rosenbaum M. (2021). Obesity: genetic contribution and pathophysiology. UpToDate. https://www.uptodate.com
Pfizer. (2022). Sweet science: high insights into fructose metabolism are helping to fight liver disease. https://www.pfizer.com
Phillips S & Shulman R. (2021). Measurement of body composition in children. UpToDate. https://www.uptodate.com
Physiopedia. (2022). Physical activity and the built environment. https://www.physio-pedia.com
President’s Council on Sports, Fitness & Nutrition (PCSFN). (2021). Facts and statistics. http://www.fitness.gov
Puccinelli P, da Costa T, Seffrin A, et al. (2021). Reduced level of physical activity during COVID-19 pandemic is associated with depression and anxiety levels: an internet-based survey. BMC Public Health, 21, 425. https://doi.org/10.1186/s12889-021-10470-z
Ramsey P & Schenken R. (2021). Obesity in pregnancy: complications and maternal management. UpToDate. https://www.uptodate.com
Research Features. (2021). How opioids drive our salt consumption. https://researchfeatures.com
Ronan L, Alexander-Bloch A, & Fletcher P. (2019). Childhood obesity, cortical structure and executive unction in healthy children. Cerebral Cortex, 30(4), 2519–28. https://doi.org/10.1093/cercor/bhz257
RXResource. (2022). Physical activity. https://www.rxresource.org
Saber A. (2021a). What is the pathophysiology of obesity. Medscape. https://www.medscape.com
Saber A. (2021b). Bariatric surgery treatment and management. Medscape. https://emedicine.medscape.com
Sarkar S, Kochhar K, & Khan N. (2019). Fat addiction: psychological and physiological trajectory. Nutrients, 11(11), 2785. doi:10:3390/nu11112785
Schwarz SM. (2020). Obesity in children: overview. Medscape. https://emedicine.medscape.com
Sease K, Rolke L, Forrester J, & Griffin S. (2021). Feedback following a family-focused pediatric weight management intervention: Experiences from the New Impact Program. J Patient Exp, 8. doi:10.1177/23743735211008309
Sherrell Z. (2021). What is weight discrimination? https://www.medicalnewstoday.com
Skalidis A, Kelleher A, & Kristo, A. (2021). Mediterranean diet. Encyclopedia, 1(2), 371–87. https://doi.org/10.3390/encyclopedia1020031
Skelton J. (2021). Management of childhood obesity in the primary care setting. UpToDate. https://www.uptodate.com
Skelton J & Klish W. (2021). Comorbidities and complications of obesity in children and adolescents. UpToDate. https://www.uptodate.com
Taylor A. (2021). Blood clots: five reasons they happen. https://theconversation.com
Tomiyama A. (2019). Stress and obesity. Annu. Rev. Psychol, 701, 703–18. https://doi.org/10.1146/annurev-psych-010418-102936
Tuvia N, Pivovarova-Ramich O, Murahovschi V, et al.(2021). Insulin directly regulates the circadian clock in adipose tissue. https://www.nigms.nih.gov
U.S. Food & Drug Administration (U.S. FDA). (2020). Weight-loss and weight-management devices. https://www.fda.gov
University of Rochester Medical Center (URMC). (2022). When your weight gain is caused by medicine. https://www.urmc.rochester.edu
Vafiadis D. (2021). How excess weight impacts our mental and emotional health. https://www.ncoa.org
Vaskovic J. (2021). Adipose tissue. https://www.kenhub.com
Villines Z. 2021. What to know about obesity discrimination in healthcare. https://www.medicalnewstoday.com/articles/obesity-discrimination-in-healthcare
Virtanen M, Jokela M, Lallukka T, et al. (2020). Long working hours and change in body weight: analysis of individual-participant data from 19 cohort studies. Int J Obes, 44, 1368–75. https://doi.org/10.1038/s41366-019-0480-3
Vorvick L. (2020). Weight gain after quitting smoking: what to do. https://medlineplus.gov
Wang, L, Steele E, Du M, et al. (2021). Youth trends in consumption of ultraprocessed foods among US youths aged 2–19 years, 1999–2018. JAMA, 326(6), 519–30. doi:10.1001/jama.2021.10238
Ward Z, Bleich S, Long M, & Gortmaker S. (2021). Association of body mass index with health care expenditures in the United States by age and sex. PLoS ONE, 16(3), E0247307. https://doi.org/10.1371/journal.pone.0247307
Watson S. (2020). Polycystic ovary syndrome (PCOS) and weight gain. https://www.webmd.com
Weir K. (2019). Family-based behavioral treatment is key to addressing childhood obesity. APA, 50(4), 30. https://www.apa.org
Weller M. (2021). Effective obesity management requires recognizing barriers, long-term treatment. https://www.healio.com
West M. (2022). What to know about the body positivity movement. https://www.medicalnewstoday.com
Więckowska-Gracek A, Mietelska-Porowska A, Wydrych M, & Wojda U. (2021). Western diet as a trigger of Alzheimer’s disease: from metabolic syndrome and systemic inflammation to neuroinflammation and neurodegeneration. Ageing Research Reviews, 70, 101397.
World Obesity. (2019). Weight stigma. https://www.worldobesity.org
World Health Organization (WHO). (2022a). Obesity and overweight. http://www.who.int
World Health Organization (WHO). (2022b). BMI classification. http://apps.who.int
World Population Review (WPR). (2021). Obesity rates by country 2021. https://worldpopulationreview.com





Customer Rating
4.9 / 1878 ratings