Asthma Patient Care
Online Continuing Education Course

Course Description
Asthma Patient Care. 10-contact-hour continuing education course on asthma signs and symptoms, diagnosis and assessment, pharmacologic treatments, long-term management, complications, breathing difficulty, and managing attacks. Applicable for nursing, occupational therapy, and other practitioners.
Note: This course is also available as part of a package. See Nursing CEU Bundle - 30 ANCC Hours
Course Price: $49.00
Contact Hours: 10
Case Management Contact Hours: 7.5
Pharmacotherapeutic Hours: 1.25
Course updated on
October 2, 2024
"Great course! Very informative. It helped clear up some questions and confusion I had about asthma." - Casey, OTA in New Mexico
"Excellent course! I highly recommend it. It's a very good value for the number of CEs offered, with well-organized, up-to-date content." - Theresa, RN in Michigan
"I found this course to be informative. Even having been an RN for 18 years, I learned new info!" - Hannah, RN in Georgia
"Enjoyed this course, as I can apply it both professionally and personally." - Bethany, PT in Kentucky
Asthma Patient Care
Copyright © 2024 Wild Iris Medical Education, Inc. All Rights Reserved.
LEARNING OUTCOME AND OBJECTIVES: Upon completion of this course, you will have increased your knowledge of how to plan, deliver, and evaluate evidence-based preventative and therapeutic care for patients at risk for asthma and patients who have asthma. Specific learning objectives to address potential knowledge gaps include:
- Define “asthma” and its types.
- Discuss the impacts of asthma.
- Review the pathophysiology, signs and symptoms, etiology, and contributing factors related to the development of asthma.
- Describe the diagnostic process and assessment of asthma severity.
- Review pharmacologic and nonpharmacologic treatments for asthma.
- Describe the management of acute asthma attacks/exacerbations.
- Summarize the elements of long-term asthma management.
- Identify the roles of respiratory, physical, and occupational therapy in the long-term management of asthma.
- Describe complications of asthma.
- Discuss asthma care for special populations.
TABLE OF CONTENTS
- Introduction
- Defining Asthma
- Impacts of Asthma
- Asthma Pathophysiology
- Etiology
- Asthma Signs and Symptoms
- Diagnosing Asthma
- Asthma Treatment
- Management of Asthma Exacerbations (Attacks)
- Asthma Inpatient Management
- Long-Term Asthma Management
- Interdisciplinary Therapies
- Asthma Complications
- Special Populations and Situations
- Conclusion
- Resources
- References
INTRODUCTION
Most people go through their days blissfully unaware of the approximately 25,000 breaths they take every 24 hours. This allows them to enjoy life and pursue their goals in relative comfort. They may experience some shortness of breath with exertion, but otherwise they breathe along nicely without concern.
For persons who have asthma, those 25,000 breaths may become the focus of their day. Depending on the severity of their symptoms, some may experience only occasional wheezing and shortness of breath, but for others each breath must be earned through great effort. Sometimes people with asthma know why an asthma attack (exacerbation) has occurred, and at other times they may be unaware of what triggered it, living with a sense of uneasiness even when they are doing well.
In those who must fight for each breath, fear and anxiety often aggravate the problem. Relief from this struggle becomes the only thing such people may think about, and they know they need help. Self-management often works, but there are times when a trip to the emergency room is necessary to reverse the disease process and return the patient to maintenance status once again. Sometimes, the person is not so lucky and may need to be hospitalized. Regrettably, asthma may even lead to death.
DEFINING ASTHMA
The Global Initiative for Asthma (GINA, 2024) provides a clinical definition of asthma, describing it as a heterogeneous disease (a condition with several etiologies) usually characterized by chronic airway inflammation. Asthma is defined by the history of such respiratory symptoms as:
- Wheezing
- Shortness of breath
- A feeling of tightness in the chest
- Cough that varies over time and in intensity
- Variable expiratory airflow limitation
These symptoms and airflow limitations may resolve by themselves or in response to medication, and may be absent sometimes for weeks or months at a time. For other individuals, however, episodic flare-ups of asthma may be life-threatening.
Asthma Phenotypes and Endotypes
A disease phenotype describes clinically observable characteristics of a disease without direct relationship to an underlying pathophysiology. Endotypes, however, describe subtypes of a disease defined by an intrinsically distinct pathogenetic mechanism; they refer to specific cells or molecules in blood or sputum.
ALLERGIC (EXTRINSIC) ASTHMA
Allergic (extrinsic) asthma is the result of antigen/antibody reaction in the respiratory tract, causing release of inflammatory mediators from mast cells that elicits the clinical response associated with an asthma attack. This is the most recognizable phenotype. It most often begins in childhood and is associated with a past and/or a family history of allergic diseases (e.g., eczema). Common allergies may include, but are not limited to:
- Tobacco smoke
- Animal dander (cats, birds, dogs)
- Dust mites
- Cockroaches
- Molds
- Pollens
(Miller, 2024)
NONALLERGIC (INTRINSIC) ASTHMA
Nonallergic (intrinsic) asthma is the result of neurologic imbalances in the autonomic nervous system in which alpha- and beta-adrenergic sites and cholinergic sites of the system are not properly coordinated. The autonomic nervous system plays an important role in asthma, primarily through the parasympathetic pathway, promoting bronchoconstriction. The airways of people with nonallergic asthma respond to such factors as:
- Cold or dry air
- Heat and humidity
- Fragrances
- Stress
- Anxiety
- Strenuous exercise
- Hormonal changes
In addition, any factor that diminishes oxygen availability can also play a part in intrinsic asthma. These may include:
- Anemia
- Dehydration
- Tissue alkalosis
- Neuromuscular disease (thoracic cage, diaphragm, and accessory muscles)
Patients with nonallergic asthma often demonstrate less short-term response to inhaled corticosteroids (GINA, 2024).
Occupational Asthma
Occupational asthma is a type of intrinsic asthma caused by exposure to inhaled irritants in the workplace. It is often a reversible condition, meaning that symptoms may disappear when the irritants that caused the asthma are avoided. However, permanent damage can result if the person experiences prolonged exposure. Examples of workplace irritants include:
- Animal substances, such as proteins found in dander, hair, scales, fur, saliva, and body wastes
- Chemicals used to make paints, varnishes, adhesives, laminates, soldering resin, insulation, packaging materials, foam mattresses, and upholstery
- Enzymes used in detergents and flour conditioners
- Metals, particularly platinum, chromium, and nickel sulfate
- Plant substances, including proteins found in natural rubber latex, flour, cereals, cotton, flax, hemp, rye, wheat, and papain (digestive enzyme derived from papaya)
- Respiratory irritants, such as chlorine gas, sulfur dioxide, and smoke
Specific symptoms of occupational asthma include airway irritation, obstruction, and inflammation, worsening after arriving at work and improving on weekends or during extended periods away from work (Mayo Clinic, 2024f).
Eosinophilic Asthma
Eosinophilic asthma, a nonallergic intrinsic endotype of the disease, is characterized by an increase in the number of eosinophils in the blood, lung tissue, and mucus in the respiratory tract. The entire respiratory tract is involved in airflow obstruction, from the sinuses to the small or distal airways.
Eosinophils release a number of different mediators with the capacity to cause airway hyperresponsiveness and are major effectors of lung tissue damage in asthma, contributing to airway remodeling. Early eosinophilia is an early feature of asthma exacerbations (also referred to as asthma attacks).
Eosinophilic asthma is rare and usually begins in adulthood. The symptoms are often severe and can be persistent. The medications used in the treatment of asthma do not have much effect on eosinophilic asthma, even at high doses (Moore, 2024).
Obesity-Associated Asthma
Obesity-associated asthma, a type of intrinsic asthma, occurs in both children and adults. Both asthma and obesity have a considerable hereditary component, and potential underlying mechanisms include a shared genetic complement, dietary and nutritional factors, alterations in the gut microbiome, systemic inflammation, metabolic abnormalities, and changes in lung anatomy and function.
Maternal obesity and weight gain during pregnancy are independently associated with an increased risk of asthma in the child. Excessive weight gain in infancy has also been linked to recurrent wheezing and asthma (Reyes-Angel et al., 2022).
Aspirin-Exacerbated Respiratory Disease (AERD)
AERD is a distinct intrinsic eosinophilic phenotype of severe asthma consisting of three key features: asthma, nasal polyps, and severe respiratory symptoms that are exacerbated by aspirin and other nonsteroidal anti-inflammatory drugs. This asthma phenotype is characterized by the initial symptoms of rhinosinusitis and then progresses to severe asthma symptoms. AERD usually begins in young adulthood, although children can be affected, and may not include any other allergies (Laidlaw & Boyce, 2023).
Cough-Variant Asthma
Asthma may present as an apparently nonspecific cough. When cough is the only asthma symptom, it is known as cough-variant asthma. In this type of asthma, the cough may come and go with the seasons, appear after an upper respiratory infection, or become worse with exposure to cold air or certain chemicals or fragrances. Cough-variant asthma may cause coughing during the day or night, sometimes disrupting sleep.
Specific symptoms include a chronic, nonproductive cough with a sensitive cough reflex. In some children, chronic cough can be the most prominent presenting symptom of asthma. The cough is typically dry, and there is an absence of wheezing, exertional dyspnea, or atopy (genetic predisposition for allergies). It is possible for this form of asthma to progress to asthma with all of its other symptoms.
Studies suggest that asthma is an uncommon cause of cough in children, as some children show no benefit from treatment with beta agonists and steroids (Marchant & Chang, 2024).
NOCTURNAL ASTHMA
Nocturnal asthma can be either intrinsic or extrinsic and is a characteristic feature of asthma that is not well controlled in a patient with daytime asthma symptoms. Nocturnal asthma is associated with circadian patterns in which the best lung function occurs at around 4 p.m. and worst at around 4 a.m. It is also associated with more severe disease and increased mortality, with up to 80% of asthma deaths in hospitalized patients occurring at night (Abdo et al., 2021; Wang et al., 2021).
Nocturnal asthma is caused by:
- Neurohormonal change
- Lung function and bronchial hyperresponsiveness
- Distal airway inflammation
- Inhibition of the anti-inflammatory effect of glucocorticoids
- Increased pulmonary capillary blood volume
- Reduced beta-2 adrenoceptor function and gene function
- Gastroesophageal reflux with aspiration
(Martin R, 2024)
EXERCISE-INDUCED BRONCHOCONSTRICTION
Exercise-induced bronchoconstriction (EIB) was formerly referred to as exercise-induced asthma, wrongly suggesting that exercise causes asthma. EIB is a narrowing of the airways in the lungs triggered by strenuous exercise. EIB occurs in up to 90% of people with asthma and up to 20% of those without asthma (O’Byrne, 2024). Elite athletes have an increased prevalence of up to 20%–50% (Pigakis et al., 2022).
EIB is caused by an acute large increase in the amount of air entering the airways that requires heating and humidifying. This can result in inflammatory, neuronal, and vascular changes, ultimately leading to bronchoconstriction and symptoms of asthma.
EIB symptoms usually begin during exercise and become worse 5 to 10 minutes after stopping exercise. Symptoms most often resolve in another 30 minutes and can range from mild to severe (Nunez, 2021). Occasionally, some individuals will experience a second wave or late phase of symptoms 4 to 12 hours after stopping exercise. These symptoms are frequently less severe and can take up to 24 hours to resolve (Garry, 2024).
IMPACTS OF ASTHMA
Given the absence of a definitive laboratory test or biomarker for the diagnosis of asthma, many definitions and methods of data collection have been used and reported in epidemiologic studies in the past. To discuss the topic epidemiologically, asthma is now defined as bronchial hyperresponsiveness in the presence of wheezing in the previous 12 months (Litonjua & Weiss, 2024a).
Asthma Worldwide
Presently, asthma is a major chronic disease, affecting an estimated 260 million people worldwide. Asthma is one of the most common chronic diseases among children and affects all age groups, races, and ethnicities. However, ethnicity and socioeconomic status do influence the prevalence, morbidity, and mortality of asthma throughout the world. Asthma worldwide is the 34th leading cause of disability-adjusted years annually and is a leading cause for missed school days among children (Litonjua & Weiss, 2024a; Global Asthma Network, 2022; AAFA, 2024a).
Individuals who live in developed countries have higher asthma prevalence compared to those who have similar genetic predispositions and reside in developing countries. The higher prevalence rates are hypothesized to be more related to environmental and lifestyle causes than genetic differences.
Factors that account for the lower prevalence in developing countries include lower rates of atopy, more breastfeeding, larger household size, and, sometimes, rural residency during childhood. Another factor may be substantial underdiagnosis of asthma in some less-developed countries.
Mortality from asthma worldwide is low compared to other chronic diseases, and according to the World Health Organization (WHO) mortality database, South Africa has the highest age-standardized asthma mortality among low- and middle-income countries, while the Netherlands has the lowest among high-income countries. The WHO estimates that asthma caused 455,000 deaths in 2019, with underprescription of inhaled glucocorticoids and insufficient access to emergency medical care or specialist care playing a part in most asthma deaths (WHO, 2024; Litonjua & Weiss, 2024a).
Asthma in the United States
Data from the CDC have shown that the prevalence of asthma increased in the United States from the early 1980s to the early 2000s and subsequently decreased slightly (Litonjua & Weiss, 2024a).
Approximately 25 million Americans have asthma (about 1 in 13), including 8% of adults and 7% of children. About 20 million adults ages 18 and over have asthma, and asthma is more common in adult women than adult men. Asthma is the leading chronic disease in children, and currently there are about 5 million children under the age of 18 with asthma (CDC, 2023a).
| Age (years) |
Individuals with Asthma (thousands) |
|---|---|
| (CDC, 2023a) | |
| 0–4 | 369 |
| 5–14 | 3,123 |
| 15–19 | 1,861 |
| 20–24 | 1,969 |
| 25–34 | 3,507 |
| 35–64 | 10,079 |
| 65+ | 4,034 |
GENDER
The strongest nonmodifiable factor associated with asthma is gender. As adults, women have an increased asthma prevalence compared to men. Furthermore, women are more likely to have severe asthma, a later onset of asthma, a higher rate of hospitalizations, and higher mortality compared to men (AAFA, 2024a).
| Gender | Individuals with Asthma |
|---|---|
| (CDC, 2023a) | |
| Males (total) | 10,273,831 |
| <18 years | 2,695,146 |
| 18+ years | 7,578,685 |
| Females (total) | 14,690,043 |
| <18 years | 1,980,329 |
| 18+ years | 12,709,714 |
Asthma is more prevalent in males in childhood until they reach puberty and more prevalent in females after puberty. This has been explained by smaller airways in relation to lung size in boys compared with girls under age 10 years. This predisposes boys to worsened airway reactivity compared with girls. Boys are also more likely than girls to experience a decrease in symptoms by late adolescence. After puberty, smaller airway caliber is then observed in females. Known differences in asthma may also be due to other factors such as hormonal effects, genetic susceptibility, and immunologic response (Jenkins et al., 2022).
Asthma prevalence increases in very young persons and very old persons because of airway responsiveness and lower levels of lung function. Two thirds of all asthma cases are diagnosed before the patient is 18 years old, and about half of all children with asthma have a decrease or disappearance of symptoms by early adulthood (Morris, 2024a).
Women may be aware of worsening symptoms at times of hormonal change such as puberty, menstruation, pregnancy, and perimenopause. One third of women report worse asthma symptoms before or during a menstrual period. Some women, particularly those with severe asthma, have worse symptoms during pregnancy. Many women do, however, notice an improvement or no change at all when pregnant (Asthma UK, 2024b).
Women with severe or poorly controlled asthma during pregnancy might increase the risk of various problems, including:
- Hypertension and kidney damage (preeclampsia)
- Restricted fetal growth
- Premature birth
- Need for cesarean section
In extreme cases, the baby’s life might be in jeopardy (Huang & Namazy, 2023).
RACE/ETHNICITY
The CDC reports that asthma prevalence from 2019 to 2021 among respondents diagnosed with asthma was distributed by race and ethnicity as shown in the table below.
| Race/Ethnicity | Asthma Prevalence |
|---|---|
| (CDC, 2023a) | |
| American Indian/Alaska Native | 12.3% |
| Black non-Hispanic | 10.9% |
| White non-Hispanic | 7.6% |
| Hispanic | 6.4% |
| Asian non-Hispanic | 4.1% |
Racial and ethnic disparities in asthma are caused by complex factors, including:
- Structural determinants (systemic racism, segregation, and discriminatory policies)
- Social determinants (socioeconomic status, education, neighborhood and physical environment, employment, social support networks, and access to healthcare)
- Biologic determinants (genes and ancestry)
- Behavioral determinants (tobacco use and adherence to medications)
(AAFA, 2024a)
Minority populations are impacted by asthma more than the White population in the United States. The populations most impacted are Puerto Ricans and non-Hispanic Blacks (Nazario et al., 2022). Non-Hispanic Black people have a 2.8 times higher mortality rate than non-Hispanic White people. Puerto Ricans have a 2.17 times higher death rate from asthma than non-Hispanic Whites.
Non-Hispanic Black children have a death rate from asthma nearly eight times that of non-Hispanic White children. They are five times more likely to be admitted to the hospital for asthma as compared to non-Hispanic White children (CDC, 2022b).
Black children exposed to secondhand tobacco smoke are at increased risk for acute lower respiratory tract infections such as bronchitis. Black children living below or near the poverty level are more likely to have high levels of blood cotinine (a breakdown product of nicotine) compared to children living in higher-income families (CDC, 2022b).
GEOGRAPHY
The prevalence of asthma differs based on geography. Related factors include:
- Poverty
- Air pollution, including ozone and small particles
- Pollen levels
- Smoking laws
- Access to specialists
According to the 2021 National Health Interview Survey, the U.S. states with the highest prevalence of asthma were:
- Maine, 12.5%
- West Virginia, 12.1%
- Oregon, 11.2%
- Kentucky, 11.7%
The states with the lowest asthma prevalence were:
- South Dakota, 8.3%
- Texas, 8.4%
- Minnesota, 8.8%
- Iowa, 9.1%
- Nevada, 9.1%
(CDC, 2023b)
Asthma rates in 2018 among children ranged from 5.0% in Nebraska to 13.2% in Alabama (ALA, 2022).
Regional trends indicate that asthma is more prevalent in Eastern and Midwestern states, with Allentown, Pennsylvania, ranking as the asthma “capital” (AAFA, 2023).
ASTHMA EXACERBATION PREVALENCE
In 2019, the number of physician office visits for asthma was 4.9 million. In 2020, asthma resulted in 94,560 inpatient hospital discharges and 986,453 visits to the emergency department. Black individuals were six times more likely than White individuals to have an emergency department visit secondary to asthma (AAFA, 2024a).
ASTHMA MORTALITY
On average, 10 Americans die from asthma each day. In 2021, 3,517 people died from asthma in the United States. Many asthma deaths are avoidable with proper treatment and medical care. Adults are six times more likely to die from asthma than children. Women are more likely to die than men; however, boys are more likely to die from asthma than girls. Black Americans are nearly three times more likely to die from asthma than White Americans (AAFA, 2024a).
ASTHMA AND QUALITY OF LIFE
Asthma causes lower quality of life and has large direct and indirect economic costs. It is the most common chronic health condition in childhood. Asthma affects individuals in many ways—physically, psychologically, socially, cognitively, and financially.
- Physical effects of asthma can range from an occasional bothersome cough all the way to the life-threatening inability to breathe. The frequency and seriousness of asthma symptoms depend greatly on how well a person’s asthma is controlled as well as how severe the individual’s asthma was to begin with. In addition, asthma can affect the individual’s sleep, mobility, activities of daily living, vitality, and sexual activity.
- Psychologically, an individual having difficulty breathing can experience fear during an acute episode and constant anxiety due to the unpredictability of the disease and possibility that another episode could happen at any time. Depression and asthma are common comorbid diseases and are associated with poor asthma outcomes.
- Socially, those with asthma may experience self-consciousness in employment, schooling, social interactions, and personal relationships related to the need to use an inhaler and to avoid triggers that can set off an asthma attack. Embarrassment and social stigma may be experienced, especially by children and adolescents at a time when “fitting in” is so important.
- Cognitively, adults with longer asthma duration and lower lung function are at greatest risk for cognitive impairment owing to the increased risk of intermittent cerebral hypoxia.
- Financially, people with asthma may incur the costs of medications, outpatient visits, emergency healthcare, and admission to a hospital for treatment and monitoring.
(Abuaish et al., 2023; Fong et al., 2022; Grant et al., 2022)
ASTHMA PATHOPHYSIOLOGY
The pathophysiology of asthma is complex and involves:
- Airway inflammation
- Airway hyperresponsiveness
- Intermittent airflow obstruction
- Airway remodeling
The important role of inflammation has been substantiated, but evidence is emerging for considerable variability in the pattern of inflammation, indicating differences in phenotype, which may have a significant influence on responses to treatment.
The mechanism of inflammation may be either acute, subacute, or chronic, and the presence of airway edema and mucus secretion contributes to airflow obstruction and bronchial reactivity. Varying degrees of mononuclear cell and eosinophil infiltration, mucus hypersecretion, desquamation of the epithelium, smooth muscle hyperplasia, and airway remodeling are present.
Airway hyperresponsiveness is an exaggerated response to numerous exogenous and endogenous stimuli. The mechanisms involved include direct stimulation of airway smooth muscle and indirect stimulation by substances from mediator-secreting cells such as mast cells or nonmyelinated sensory neurons.
The progression of the underlying disease severity does not appear to be prevented by current asthma treatment with anti-inflammatory medications (Morris, 2024a).
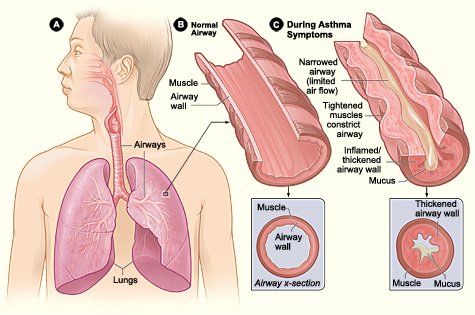
During an asthma attack, the airways of the lung narrow and the movement of air is obstructed. This narrowing is caused by three processes: muscles in the airway walls contract, the airway walls become edematous and swollen, and excess mucus fills the airways. (Source: National Institutes of Health: National Heart, Lung, Blood Institute.)
The Asthma Cascade
The asthma cascade is the well-defined constellation of signs and symptoms produced by an allergen or other factors. Allergens are normally harmless substances that the immune system treats as health threats. When a person who has the allergic type of asthma comes into contact with one of these substances after becoming sensitized to it, the immune system responds to combat it. In patients with nonallergic asthma, when something other than an allergen (e.g., exercise, cold weather) induces asthma symptoms, the immune system responds in the same manner.
Within minutes following such an exposure, the person has a reaction caused by the release of mast cells, which degenerate and release histamines, prostaglandins, bradykinins, and leukotrienes. These substances affect nerve cells, smooth muscle cells, goblet cells that secrete mucus, and endothelial cells that affect blood vessels. This results in:
- Increased capillary permeability
- Mucosal edema
- Bronchoconstriction (bronchospasm)
- Thick tenacious mucus secretion
- Hyperresponsiveness of bronchial smooth muscle
- Reversible air flow obstruction
(Aegerter & Lambrecht, 2023; Bao & Shu, 2022)
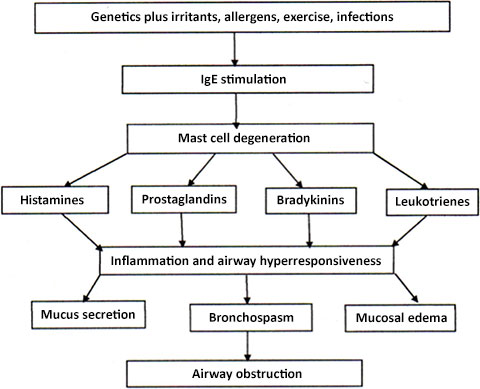
Asthma cascade. (Source: J. Swan, Author.)
Over time, damage to the epithelial cells affects ciliary function, impairing the removal of mucus and cellular debris and resulting in the formation of airway plugs. In addition, long-term damage caused by repeated bouts of untreated inflammation results in airway remodeling by epithelial cells, which may worsen inflammation and aggravate asthma over time if not treated and managed correctly.
Irreversible airway obstruction, which leads to poor prognosis and is highly associated with smoking and male gender, may develop in some patients who have moderate to severe asthma. In these patients, the structure and function of the airway changes cannot be reversed in spite of ongoing anti-inflammatory or bronchodilator treatment (Thomson et al., 2022).
Asthma Development in Children and Adolescents
Asthma usually develops in children before the age of 5 years. Many children who have allergies develop asthma, but not all.
Usually, symptoms begin in the first years of life. It has been found that about 25 out of 100 children with persistent asthma began wheezing before they were 6 months old, and about 75 out of 100 began wheezing by the age of 3 years. As a child grows, approximately:
- 15 out of 100 infants who wheeze develop persistent wheezing and go on to develop asthma.
- 60 out of 100 infants who wheeze no longer wheeze by age 6.
- 50 out of 100 preschool-age children who wheeze have persistent asthma later in childhood.
In most cases of intermittent asthma associated with respiratory infections (rather than allergies), symptoms tend to become less severe and may disappear by adolescence. But asthma seems to continue in adolescence in children who have moderate to severe asthma, and these children may have asthma as adults.
Children with persistent asthma:
- Developed symptoms before age 3
- Had allergies in infancy and childhood
- Have a family history of allergies
- Wheeze without a viral infection present
- Have recurrent asthma attacks associated with viral infections (e.g., respiratory syncytial virus)
- Have been exposed to tobacco smoke, including before birth
Other risk factors that increase a child’s likelihood of developing asthma include:
- Living in an area with high pollution
- Obesity
- Being male
- Being Black or Puerto Rican
(UM, 2023; Mayo Clinic, 2024a)
Asthma Development in Adults
Asthma can develop at any point in life. Asthma that diagnosed in people older than age 20 is known as adult-onset asthma. New-onset asthma in adults is often the result of undiagnosed childhood asthma. However, some people who had childhood asthma tend to experience reappearance of symptoms through their 30s and 40s at various levels of severity.
Unlike children who often have experienced intermittent asthma symptoms in response to allergy triggers or respiratory infections, adults with newly diagnosed asthma generally have persistent symptoms, and daily medications may be required to keep their asthma under control.
There are several factors that make a person more likely to develop adult-onset asthma. Being a woman increases the risk after age 20, and obesity appears to significantly increase the risk. Individuals who had asthma as a child may see asthma recur later in life.
At least 30% of adult asthma cases, especially in adults who are allergic to cats, are triggered by allergies. Exposure to allergens or irritants such as cigarette smoke, chemicals, mold, dust, or other substances commonly found in the person’s environment, including home or work, may trigger the first asthma symptoms, and prolonged exposure to certain occupational workplace materials may set off asthma symptoms in adults.
Hormonal fluctuations in women may play a role in the development of adult-onset asthma, and some women first develop asthma symptoms during or after pregnancy. Women going through menopause can also develop asthma symptoms for the first time.
Different illnesses, viruses, or infections can be a factor in the development of adult-onset asthma, and a serious cold or bout with influenza is often a factor. Smoking is not a cause of adult-onset asthma; however, smoking or being exposed to secondhand smoke may provoke asthma symptoms (AAFA, 2024b).
Asthma Development in Older Adults
Asthma can develop in anyone at any age, and it is not uncommon for adults in their 70s or 80s to develop asthma symptoms for the first time. The most common triggers for the appearance of asthma include respiratory infection or virus, exercise, allergens, and air pollution (AAFA, 2024c). Up to half of adults with an asthma diagnosis are current or former smokers. Tobacco smoke damages the airways, which then respond with asthma symptoms, and contributes to worsened control of symptoms (Thomson et al., 2022).
ETIOLOGY
Although the fundamental causes of asthma are not completely understood, there is strong evidence that the development of asthma includes a combination of genetic predisposition and environmental exposure to ingested or inhaled substances that could provoke allergic reactions or irritate the airways as well as to infectious agents.
Genetic Contributions
Asthma runs in families, and if one identical twin has asthma, the other twin is likely to have it. Observations such as these demonstrate that the tendency to develop asthma is inherited. Over 100 different genes are thought to be linked to asthma, and through linkage studies (i.e., gene “hunting” and genetic testing), the following novel genes for asthma have been identified:
- ADAM33: A gene that influences lung function in early life and affects how people inhale and exhale
- VDR: Provides instruction for making vitamin D receptors, allowing the body to respond to vitamin D, low levels of which are linked to increased risk of asthma attacks
- DPP10: A rare mutation associated with asthma that encodes a protein that binds specific voltage-gated potassium channels that play a significant role in cytokine production and airway smooth muscle cell and goblet cell function
- PHF11: A regulator of human atopic disease
- HLA: Genes involved in the regulation of immune-specific responses to common allergens
- GPR154: Increased expression of this gene in ciliated cells of the respiratory epithelium and in bronchial smooth muscle cells
- BPFIB1: A key component for clearance of mucus containing inhaled particles and pathogens from the airway
(Donoghue et al., 2023; Weiss, 2021)
Lung Microbiome
The notion that the lungs are sterile has been abandoned now that evidence has been found of bacterial populations (microbiome) in the lung and that intestinal microbiota provide these bacteria. Each person has a unique microbiota, and when microbial populations are disturbed, a negative impact occurs, known as dysbiosis. A higher microbial abundance and species variation are observed in chronic disease states of the respiratory tract, including asthma.
It has been reported that several fungi associated with intestinal dysbiosis could enhance the severity of asthma, since intestines and lungs communicate and work in tandem. Specific types of proteobacteria are pronounced in asthma and are usually associated with uncontrolled asthma. In addition, Firmicutes with the genus Lactobacillus have been isolated in asthmatic patients, and Firmicutes with the genus Clostridium have been isolated in children with airway allergies (Stavropoulou et al., 2021).
OXIDATIVE STRESS AND ENZYME ANTIOXIDANTS
Asthma and asthma exacerbations are characterized by high oxidative stress and impaired macrophage function. Oxidative stress is an imbalance between the production of free radicals and the ability of the body to counteract or detoxify their harmful effects through neutralization by antioxidants. Free radicals are oxygen-containing molecules that have one or more unpaired electrons, making them highly reactive with other molecules.
Oxidative stress is associated with a decreased capacity of macrophages to respond to pathogens, and this appears to be crucial in the insufficient initial response to exacerbating stimuli. Modulating the inflammatory response of macrophages in the lung may have the potential to repair damaged tissue caused by asthma as well as produce macrophage-targeted treatments to reduce inflammation (Britt et al., 2023).
Environmental Contributions
In a person with asthma, substances in the environment can trigger an episode of bronchoconstriction, and it appears that exposure to some of the same substances can also initiate the disease.
TOBACCO PRODUCTS
Tobacco smoke irritates the lining of the airways and is a powerful trigger of asthma symptoms. This is true for adults, but especially so for children. Tobacco smoke harms the smoker and people exposed to secondhand smoke by:
- Damaging the cilia that sweep particles and mucus out of the airways
- Causing an increase in mucus, which, together with the damaged cilia, leads to mucus and other irritating substances building up in the airways
- Introducing many cancer-causing substances into the lungs
Secondhand smoke is a combination of smoke from a burning tobacco product and smoke that has been exhaled by a smoker. Inhaling secondhand smoke may be even more harmful than actually smoking the product because the smoke that burns off the end of a cigar or cigarette contains more harmful substances (tar, carbon monoxide, nicotine, and others) than the smoke inhaled by the smoker.
Adults and children who live with a smoker are more likely to develop respiratory illnesses such as asthma. Children with asthma are especially sensitive to secondhand smoke. They are more likely to develop asthma symptoms and to develop lung and sinus infections, which can make asthma symptoms worse and more difficult to control.
Use of tobacco products, including cigarette smoking, smokeless tobacco, and electronic cigarettes, is harmful to both mothers and unborn children, as nicotine and other substances cross the placenta and go directly to the fetus. Smoking in pregnancy causes structural changes in the placenta and impaired oxygen delivery to the fetus. Children of mothers who smoked during pregnancy are more likely to have respiratory problems and are 10 times more likely to develop asthma (Cleveland Clinic, 2021; Rodriguez, 2024).
For those who live in multiunit housing, such as an apartment, duplex, or condo, secondhand smoke from another resident’s indoor smoking can trigger asthma symptoms. Secondhand smoke can migrate from other units and common areas and travel through doorways and cracks in walls, along electrical lines, via plumbing, and through ventilation systems (ALA, 2023a).
AIR POLLUTION
Poor air quality due to an increase in the amount of carbon dioxide (CO2) emitted into the atmosphere can trigger asthma symptoms. Carbon dioxide is created by the burning of fossil fuels like coal and oil. Increases in global atmospheric CO2 concentration stimulate earlier and greater production of pollen allergens and airborne fungal spores, both known aggravators of asthma (Chatkin et al., 2022).
Increased temperatures lead to increased ground-level ozone, which causes airway inflammation and damages lung tissue. Ground-level ozone can be the most harmful for people living with asthma. It is created by a chemical reaction between nitrogen oxide and organic compounds when exposed to sunlight. These compounds can include emissions from industrial facilities, motor vehicle exhaust, and gasoline fumes. Ground-level ozone is very likely to reach unhealthy levels on hot sunny days in urban environments and is a major component of urban smog.
The populations most vulnerable to ground-level ozone are children, older adults, people with lung disease, and people who spend a great deal of time outdoors. Children are at the greatest risk and are more likely than adults to have asthma. Unhealthy rises in ground-level ozone pollution correspond with increases in emergency room visits and hospitalizations for people with asthma (AAFA, 2024d).
Each year wildfires occurring across the country have a significant effect on air quality. Smoke is made up of a complex mixture of gases and fine particles produced when wood and other organic materials burn. The biggest threat from smoke is from fine particles that can penetrate deep into the lungs. Children and those with respiratory disease like asthma are at high risk for asthma episodes when the air quality is poor. Wildfires do not affect only those in the immediate fire area; blowing smoke can impact people hundreds of miles away (AAFA, 2024d; CDC, 2023c).
PRENATAL ULTRAFINE PARTICLE EXPOSURE
Ultrafine particles penetrate deeper into the lungs, have greater ability to induce oxidative stress, and more readily enter the circulatory system. When these particles enter into the bloodstream of a pregnant woman, they cross over into the placenta and enter the bloodstream of the fetus. Because fetal development occurs through sequential biologic events, toxins that disrupt these processes can have a variable effect, depending on the nature of the pollutant as well as timing and/or exposure level.
Researchers have found that children who are exposed to ultrafine particles from air pollution in utero are more at risk of asthma in childhood than unexposed children, particularly in boys (Kim et al., 2023).
INDOOR AIR POLLUTION
Many reports and studies have found that the following populations may be disproportionately impacted by indoor asthma triggers:
- Children
- Older adults
- Low-income individuals
- Minority populations
Indoor air can be up to five times more polluted than outdoor air. Sources of indoor air pollution include:
- Fuel-burning combustion appliances
- Tobacco products
- Dust, pet dander, molds
- Cockroach allergens
- Building materials, furnishings, upholstery, carpets
- Household cleaning and maintenance products
- Personal care products
- Hobby supplies
- Central heating and cooling systems
- Humidifiers (since high humidity can lead to higher dust mite levels)
- Excess moisture
- Outdoor sources such as radon, pesticides, air pollution (especially for low-income communities and communities of color, who are far more likely to live in areas with heavy pollution)
- Inadequate ventilation
- Cooking (from oil and fat particulates)
If too little fresh air enters indoors, pollutants can accumulate to levels that pose health and comfort problems. If clean outdoor air does not replace indoor air often, then allergens and pollutants may stay in the home and recirculate. The indoor air in newer, more energy-efficient homes may become more polluted because these homes do not have the same gaps and cracks as older homes to allow air circulation (U.S. EPA, 2023).
WEATHER
Thunderstorm asthma results when a potent mix of pollen and weather conditions triggers severe asthma symptoms in a large number of people over a short period of time. Epidemic thunderstorm asthma (ETSA) outbreaks have occurred globally over the last four decades. Thunderstorm asthma has been reported in the United Kingdom, Australia, Canada, Italy, and the United States. Australia has been particularly susceptible, with nearly half of all episodes reported internationally.
Pollen grains from grasses are large and normally unable to enter the bronchial tree. However, in storms these grains get swept up in the wind and carried for long distances. Some burst open and release tiny particles that are concentrated in the wind just before the storm. These particles are small enough to enter deep into the lungs, making it difficult to breathe. This can become very severe very quickly and may be life-threatening (GINA, 2024; Hughes et al., 2022).
DIETARY FACTORS
Several food and food groups have been found to influence the development and course of asthma.
- High fat/low fiber intake: A high-fat and low-fiber diet results in increased airway hyperresponsiveness via enhanced cytokine production in the lungs.
- Dairy products: Frequent dairy consumption has been found to increase the odds of developing childhood asthma. The mechanism is unclear but may include responses to milk protein or milk lipids.
- Plant-based diet: Diets emphasizing fruits, vegetables, and whole grains, while placing less emphasis on high-fat meats and dairy products, have been associated with reduced asthma risk in children.
- Vitamin E deficiency: Vitamin E interrupts lipid peroxidation to inhibit oxidant-induced damage in human tissue. An isoform of vitamin E scavenges reactive nitrogen species, which can become elevated with acute neutrophilic inflammation. Children born to mothers with vitamin E deficiency are more likely to develop symptoms of asthma and to require medication.
- Vitamin D deficiency and insufficiency: Both deficiency and insufficiency in vitamin D levels are significantly higher in asthma patients. Children who are vitamin D deficient are more likely to have asthma. Vitamin D insufficiency has also been associated with increased risk of hospitalization or emergency department visits. Low maternal vitamin D intake during pregnancy is associated with an increased risk of children developing asthma.
(Bédard et al., 2021; Brustad et al., 2023)
RESPIRATORY INFECTIONS
Respiratory infections are common and can affect lungs, nose, sinuses, and throat, especially in children and adults with preexisting asthma.
Respiratory tract infections are a main asthma trigger and can result in severe asthma symptoms. A respiratory tract infection causes inflammation, and asthma is an inflammatory condition. Together they deliver an inflammatory onslaught that triggers an asthma attack. People with asthma can have a more severe illness and take longer to recover from respiratory infections (CDC, 2023d).
Viral Infections
There is a large body of evidence that demonstrates a link between early viral infections and asthma inception and exacerbation. Viral respiratory tract infections are the most common cause of wheezing illnesses and asthma exacerbations in both children and adults. Respiratory viruses can induce symptoms of acute bronchiolitis, croup, and recurrent wheezing in young children (Jackson & Gern, 2022; Redding, 2024).
Respiratory viruses infect and cause cytopathic damage to airway epithelium. This damage then induces the release of proinflammatory agents, which then propagate eosinophilia and stimulate the release of cytokines that promote asthma and atopic disease. Some viruses may not damage the epithelium directly but rather interact with macrophages, T cells, or mast cells to stimulate allergic airway inflammation and modulate the host’s response to allergens and irritants in the environment (Redding, 2024).
Specific viruses associated with the development of asthma include:
- Respiratory syncytial virus (RSV) in children under 2 years of age is the most common cause of wheezing and is an important risk factor for intrinsic asthma, with severe infections conferring greater risk.
- Rhinovirus (RV) (the common cold) is a more important risk factor for the development of extrinsic asthma, likely through T-helper 2-biased inflammation. Rhinovirus is more significant in adults and children older than 2 years, causing increased symptomatology in patients with preexisting asthma.
- Parainfluenza can cause lower respiratory tract infections and is most likely to affect infants, young children, the older adult, those with chronic diseases such as asthma, and those with compromised immune systems, causing new-onset asthma and also acting as an asthma trigger.
- Human metapneumovirus (hMPV) presents similar to RSV and is a common cause of upper and lower respiratory tract infections in infants and children. It also affects adults, particularly older adults, and those with weakened immune systems. Lower airway infections have been shown to trigger asthma attacks in those with existing asthma.
- Coronavirus (CoV) infections can range from a mild common cold to more severe disease such as COVID-19, which can be fatal.
- Adenovirus (AdV) has been found to initiate chronic, more persistent, and severe asthma. How AdV affects asthmatic patients, however, remains unclear.
(Redding, 2024; Jackson & Gern, 2022)
Bacterial Infections
Similar to viruses, airway bacteria have also been suggested as early-life risk factors for later development of asthma. Also, the gut microbiome, considered to be a risk factor for later development of asthma, might influence the susceptibility to viral infections in the airway.
In addition, there is substantial evidence of an interaction between bacteria and viruses in the airways. Rhinovirus has been found to be associated with increased bacterial pathogens, and Moraxella catarrhalis and Streptococcus pneumoniae seem to contribute to the severity of respiratory tract illness and asthma.
Several mechanisms are involved in which viral infections can increase the risk of bacterial infections, including immune suppression, epithelial damage, and changes in the local lung environment, altering the growth conditions for pathogenic bacteria and viruses (Lalbiaktluangi et al., 2023).
CESAREAN SECTION
Children born by cesarean section have a higher risk of asthma than those born by vaginal delivery, particularly children of parents with allergies. There are two possible causes that have been hypothesized:
- Lack of contact by the infant with the mother’s bacteria. Neonates born by vaginal delivery acquire most of their intestinal flora by being exposed to their mother’s vulvovaginal/bowel flora during birth, which influences early immune modulation (Litonjua & Weiss, 2024b).
- Infants delivered by cesarean section have less contact with stress hormones and chest pressure that normally occurs during vaginal delivery, which has a negative effect on lung function because these mechanisms are associated with the reabsorption of amniotic fluid from the lungs (Gürdeniz et al., 2022).
Neonates who are born following a planned cesarean section without labor do not experience labor-related stress and immune modulation and are at increased risk of asthma up to the age of 12 years.
In an attempt to restore normal neonatal colonization of cesarean-born neonates, vaginal seeding has been suggested; however, both the safety and the effectiveness of this practice are unproven and it is only recommended in research trials (Norwitz, 2024).
Comorbid Factors
OBESITY
Obesity is a risk factor for asthma, particularly in adult women, and the greater the body mass index (BMI), the greater the risk of asthma. An increased prevalence of asthma also occurs in children with obesity. Among adults with severe asthma, nearly 60% are obese. This is related to a complex interplay of biologic, physiologic, and environmental factors. Asthma in patients who are obese is often severe and difficult to control.
In some people, obesity precedes asthma, and obesity is a risk factor for later development of asthma. In others, asthma precedes obesity, suggesting that asthma may be a risk factor for the development of obesity.
Obesity results in mechanical changes. It increases the collapsibility of the peripheral airways and parenchyma, especially among people with late-onset asthma. Excessive accumulation of fat in the thoracic and abdominal cavities leads to lung compression and an attendant reduction in lung volume. Other factors that are likely contributors to the increased risk and severity of asthma in obese individuals include:
- Genetics, evidenced by twin studies suggesting 8% of genetic component is shared with asthma
- Air pollution and parental smoking, which are independent risk factors for both obesity and asthma
- Dietary factors, including high sugar or saturated fat intake or low antioxidant or fiber intake
- Lung growth in children (e.g., increased lung volume relative to airway caliber)
- Adipose tissue proinflammatory mediators
- Immune cell function alterations (e.g., suppression of T-helper lymphocyte function or lymphoid cell response to intrinsic damage)
- Increased oxidative stress with late-onset asthma
(Dixon & Nyenhuis, 2024)
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
Chronic obstructive pulmonary disease (COPD) has been found in a significant proportion of patients who present with symptoms of chronic airway disease. These patients have features of both asthma and COPD, which is referred to as asthma-COPD overlap (ACO), although specific features that can be used to make a diagnosis of ACO have yet to be agreed upon.
Despite the lack of a well-accepted definition, there are a range of features that support the diagnosis of ACO, including:
- Age 40 years or older
- Persistent respiratory symptoms, but variability in symptoms may be prominent
- Airflow limitation that is not fully reversible
- History of doctor-diagnosed asthma at some point
- History of atopy or allergies
- Exposure to a risk factor such as tobacco smoking or equivalent indoor/outdoor pollution
Research efforts are needed to better understand asthma and COPD phenotypes and what types of biomarkers (physiologic, radiologic, or biologic) help to distinguish those patients with ACO who are most responsive to specific therapies (Han, 2024).
GASTROESOPHAGEAL REFLUX DISORDER
Studies have shown that gastroesophageal reflux disorder (GERD) can trigger asthma symptoms. In addition, GERD is more common in people with asthma than in the general population, and anyone—including infants, children, and teens—can develop GERD. Individuals with asthma that is especially difficult to treat appear more susceptible to GERD than other affected persons. GERD is thought to cause asthma symptoms in one of two ways:
- Stomach acid that enters the esophagus irritates nerve endings, and the brain responds with impulses to the lungs stimulating muscle and mucus production in the airways, which then constrict, resulting in asthma symptoms.
- Refluxed stomach contents are aspirated into the lungs, irritating the airways and causing the symptoms of asthma to occur.
It is also believed by some that asthma may trigger GERD. Either breathing difficulties or certain asthma medications cause the esophageal sphincter muscle to relax and allow stomach contents to reflux, which then causes asthma symptoms, completing a cycle. GERD may also be related to eating specific foods or, rarely, to food allergies (AAFA, 2024e).
CASE
JONAH, AGE 11
Jonah is an 11-year-old boy whose identical twin brother, Adam, was diagnosed with asthma at age 8. Jonah is brought to the pediatrician’s office by his mother, Laura, who tells the office nurse that Jonah has been experiencing episodes of wheezing and shortness of breath over the last 2 weeks, during which time there have been several days of high humidity and poor air quality.
When asked about Jonah’s medical history as part of the nursing assessment, Laura reported that the twins had been delivered by cesarean section. She cannot recall any early respiratory infections in Jonah, though she notes that he seems to have become more susceptible to colds in recent years. When asked about her own history, Laura recalls periodic episodes of wheezing and coughing when she was a young girl, but she was never screened for asthma.
Because Jonah’s twin brother has been diagnosed with asthma, the twins were born by cesarean section, Laura possibly had asthma as a young girl, and Jonah is reactive to temperature and air pollution, it is decided to screen and test Jonah for asthma. These tests are completed in the office, and a diagnosis of asthma is confirmed.
(Continues later in this course under "Asthma Patient Education.")
ASTHMA SIGNS AND SYMPTOMS
The classic signs and symptoms of asthma are coughing, wheezing, and dyspnea.
But asthma symptoms vary from patient to patient, and symptoms can change as a patient ages. The type of asthma symptoms a patient has, how often they occur, and how severe they are may also vary over time. Some people with asthma may have extended symptom-free periods interrupted by periodic asthma episodes, while others have some symptoms every day. Sometimes symptoms might be experienced as an irritation, while at other times they may limit activities of daily living. Severe symptoms can be fatal, and it is important they be treated as soon as they occur so they do not become severe (Cleveland Clinic, 2022a).
Most children with asthma exhibit symptoms before they turn 5. In very young children, it may be difficult for parents and clinicians to recognize that the symptoms are due to asthma. Symptoms of pediatric asthma can range from a nagging cough that lingers for days or weeks to sudden and scary breathing emergencies.
While other conditions can cause the same symptoms as asthma, the pattern of symptoms in people who have asthma usually has some of the following characteristics:
- Symptoms come and go over time or within the same day.
- Symptoms start or get worse with viral infections, such as a “cold.”
- Symptoms are triggered by exercise, allergies, cold air, or hyperventilation from laughing or crying.
- Symptoms are worse at night or in the morning.
(NHLBI, 2024a)
Coughing
Coughing may be the only symptom of asthma, especially in cases of exercise-induced bronchoconstriction or nocturnal asthma. Usually, the cough is nonproductive and nonconvulsive. A recurring cough may be a symptom of asthma. It is more likely to indicate asthma if the cough is accompanied by other asthma symptoms. However, not everyone with asthma coughs.
Frequent coughing, especially at night, is usually dry and nonproductive, but in some people with uncontrolled asthma, there may be thick, clear mucus. Children with nocturnal asthma tend to cough after midnight and during the early hours of the morning (Asthma UK, 2024a; Morris, 2024a).
Wheezing
Wheezing is a musical, high-pitched, whistling sound caused by airflow turbulence. It is one of the most common symptoms of asthma. Wheezing is produced by air being forced through narrowed airways, and in asthma the affected airways are mainly the small bronchioles of the lungs. Asthma can occur without wheezing, however, when the obstruction predominately involves the small airways.
In the mildest form of asthma, wheezing is heard only at the end of expiration. As severity increases, the wheeze lasts throughout expiration. In a more severe asthmatic attack, wheezing is also present during inspiration. In the most severe attacks, wheezing may be absent because of the severe limitation of airflow associated with airway narrowing and respiratory muscle fatigue (Morris, 2024a).
Many babies and young children wheeze due to colds or viruses and do not develop asthma as they get older. The diagnosis of asthma in children usually cannot be made until they are older, by age 4 or 5 (Sawicki & Haver, 2024a).
Dyspnea
Dyspnea, or shortness of breath, has many causes and is very common. The experience of dyspnea arises from interactions among multiple physiologic, psychological, social, and environmental factors. Bronchoconstriction leads to a series of sensations as the degree of constriction worsens, from chest tightness to an increased effort to breathe to a sensation of air hunger. Patients often complain of an increased effort to breathe.
Asthma is most likely the cause of dyspnea when:
- It is accompanied by coughing and wheezing
- Symptoms seem to be triggered by specific factors (e.g., allergens, cold air, exercise)
- The person is an adult who had asthma or asthma-like symptoms as a child
- The person has hay fever or other allergies or family members with allergies or asthma
(Schwartzstein, 2024; Li, 2024)
Airway Mucus Hypersecretion
Mucus is the normal secretory product of the epithelial lining and contains secreted water, sugar, proteins, lipids, minerals, and mucins. Under normal conditions, mucus protects the airways and moistens the air. Patients with severe asthma or with asthma that is not well controlled produce extra mucus that worsens the obstruction in their airways.
Inflammation and oxidative stress cause the inner lining of airways to swell and produce mucus. Patients with hypersecretion have more dyspnea, have poorer asthma control and quality of life, and experience more exacerbations. They are significantly older, with a longer duration of disease and more frequent severe asthma. They also have greater airflow obstruction and a higher number of emergency department visits.
The mucus produced in asthma is thicker and stickier (more viscous) than normal. Additionally, in persons with asthma, the cilia (specialized cells that cleanse the airways of inhaled particles and mucus) are dysfunctional. Asthmatic mucus is more likely to remain in the airways and form plugs that make it more difficult for patients to clear their lungs by coughing (Jesenak et al., 2023).
Sleep Disturbances
About 75% of people with asthma are wakened by nighttime symptoms at least once a week. Around 40% of people with asthma experience nocturnal symptoms every night. Having poorly controlled severe asthma makes a person more likely to experience nocturnal symptoms.
The mechanism underlying this is not fully understood but may be related to normal circadian hormonal changes that take place in the evening. These changes may contribute to inflammation in the airways, increasing the risk of nocturnal asthma symptoms. Other mechanisms may also include obesity, GERD, and environmental triggers (Newsom & Rehman, 2023).
Signs and Symptoms Unique to Children
Asthma in children is not different from asthma in adults, but children face unique challenges. Infants and young children with asthma display the following characteristics:
- Breathlessness at rest
- Loss of interest in feeding
- Sitting upright
- Talking in words, not sentences
- Common agitation
- Chest retractions
- Vomiting with cough
With imminent respiratory arrest, the child displays the symptoms mentioned above and is also drowsy and confused. Adolescents, however, may not have these symptoms until they are in frank respiratory failure (hypoxia, hypercarbia, increased work of breathing).
For children older than 2 years, asthma can cause:
- Shortness of breath
- Easy fatigability
- Complaints of feeling ill
- Poor school performance
- Avoidance of normal activities such as playing outside or visiting friends
(Sharma, 2024)
DIAGNOSING ASTHMA
There is no “gold standard” or standardized diagnostic criteria for asthma. Diagnosis is based on the patient’s history, physical examination, consideration of other diagnoses, and documentation of variable expiratory airflow limitation as determined by spirometry. In some instances, observing a response to treatment may confirm an asthma diagnosis, but lack of a response to treatment does not rule out asthma (NACA, 2023).
History
Given the wide variation in presentation, a detailed history is needed to understand each individual’s particular asthma variant. Information necessary for assistance in making a diagnosis of asthma requires asking the patient about:
- Current symptoms: Are they occurring mostly in the daytime, at night, or both?
- Pattern of symptoms: What is their course over a day, week, or year?
- Chronology: What is the chronologic history of the symptoms over the person’s lifetime?
- Smoking history: Does or did the patient smoke (tobacco, cannabis)? Has the person been exposed to secondhand smoke?
- Precipitating or aggravating factors: What brings the symptoms on or what makes them worse, e.g., do they occur with exercise or with viral infections?
- Relieving factors: Is there anything that relieves the symptoms, e.g., medications?
- Home or work exposure: What types of environmental exposures are present in the home or workplace?
- Impact of symptoms: How do the symptoms affect the person’s occupation, lifestyle, and activities of daily living?
- Past history: Is there a history of allergies, including atopic dermatitis (eczema) or allergic rhinitis (hay fever)? Is there a history of other pertinent medical conditions such as COPD?
- Family history: Is there is history of asthma and/or allergies among family members?
(NACA, 2023)
EXACERBATION HISTORY
The exacerbation history is important with respect to the following:
- Usual prodromal signs or symptoms
- Rapidity of onset
- Associated illnesses
- Number in the last year
- Need for emergency department visits, hospitalizations, ICU admissions, and intubations
- Missed days from work or school
- Activity limitation
(Morris, 2024a)
HISTORY OF SYMPTOMS IN CHILDREN
When taking a history of a child with wheezing or asthma-like symptoms:
- Confirm that the breathing sounds described by the parents (caregivers) as wheezing are actually “wheeze.”
- If possible, see the child during a bout of wheezing.
- Ask the parents (caregivers) to make an audio or video recording of noisy breathing.
- Ask the parents (caregivers) to describe exactly what they see or hear, and then show them a video of true wheezing and ask whether the signs match those of the child.
- Ask about the appearance of the child’s chest during episodes of noisy breathing (use of accessory muscles to breathe, retractions of the chest wall adjacent to the ribs).
(NACA, 2023)
TYPICAL ASTHMA SYMPTOM PATTERNS
Although asthma is described as a disease with episodic attacks, the pattern of clinical symptoms varies from person to person. In the medical history, recognition of the pattern of symptoms is pivotal to raising the possibility of a diagnosis of asthma. The symptom pattern of the individual should be described, noting these features:
- Whether the symptoms occur continually, episodically, or both
- Onset of symptoms, duration, and frequency
- Whether the symptoms occur perennially, seasonally, or both
- Diurnal variations, especially nocturnal and upon awakening early in the morning
- For women, whether the symptoms occur during a particular part of the menstrual cycle
Children with chronic asthma may have one of several distinct patterns of symptoms, and the asthma pattern can change over time. These may include:
- Intermittent asthma attacks with no symptoms between them
- Chronic symptoms with intermittent worsening
- Attacks that become more severe or frequent over time
- Morning “dipping” (when the symptoms worsen in the morning and improve throughout the day)
(Sawicki & Haver, 2024b)
ASTHMA TRIGGERS AND AGGRAVATING FACTORS
Once asthma is acquired, it is a disease of episodic bouts of wheezing, coughing, and difficulty breathing. Regardless of the factors that entered into the initial development of asthma, there are multiple triggers and aggravators that can bring about exacerbations in a patient with an established diagnosis of asthma.
Many of the factors that are implicated in the development of asthma can also trigger an exacerbation. For asthma patients, it is necessary to learn what those triggers and aggravators are. For some, the triggers are hard to identify, and their asthma symptoms seem to appear spontaneously.
| Type | Examples |
|---|---|
| (ALA, 2023c; U.S. EPA, 2024; MN DOH, 2024; Simon, 2024) | |
| Infections and comorbid conditions |
|
| Hormonal changes |
|
| Inhaled substances |
|
| Ingested substances |
|
| Physical factors |
|
| Comorbid conditions |
|
| Characteristics of the home |
|
| Environmental changes |
|
| Exercise |
|
| Emotional situations |
|
CHRONOLOGY OF THE PATIENT’S ASTHMA
The chronology section of a patient’s asthma history includes major disease events and treatments:
- First appearance of symptoms
- Date of diagnosis
- Dates of ED visits and hospitalizations (noting any ICU admissions or intubations)
- Dates of related medical and health problems
- Treatment history
- Treatment routine currently in effect
Of great significance is a past near-fatal asthma exacerbation requiring endotracheal intubation, which is the greatest single predictor of death from bronchial asthma (Chakraborty et al., 2024).
CASE
ASTHMA HISTORy
James, age 61, recently moved to another town and made his first visit to a new primary care physician. As part of his intake assessment, the nurse in the office collected the following information:
- Born to parents who smoked
- Age 4–7, some wheezing with colds
- Age 7, mild hay fever began yearly
- Age 16, started smoking (infrequently)
- Age 18, smoking regularly, with occasional coughing spells
- Age 25, choking/coughing episode, possible asthma diagnosed in ED
- Age 25, given inhaler for asthma attacks, stopped smoking
- Age 25–29, used inhaler occasionally
- Age 29, divorced, moved to new city, began smoking again
- Age 30, two visits to ED for asthma attacks
- Age 31–36, physician changed PRN bronchodilator to isoproterenol (Isuprel); slowly stopped smoking completely
- Current regimen, albuterol (Proventil) PRN, which is effective at reversing the four or five asthma episodes each year, most often in the early summer (hay fever season), and on occasion in cold wintry weather; weight at pre-age 45 levels; no ED visits in more than 20 years
FAMILY HISTORY
The family history section of the medical history lists those close relatives with atopic illnesses such as:
- Asthma
- Allergies
- Sinusitis
- Rhinitis
- Eczema
- Nasal polyps (a condition associated with asthma)
Atopic illnesses share an underlying problem with the immune system, predisposing persons toward the development of allergic hypersensitivity reactions (Morris, 2024a).
SOCIAL HISTORY
Social history includes:
- Smoking
- Workplace or school characteristics
- Educational level
- Employment
- Social support
- Factors that may contribute to nonadherence of asthma medications
- Illicit drug use
(Morris, 2024a)
Impact of Asthma on Patient and Family
It is always important to respond to diseases in a way that addresses practical problems in patients’ lives. The goal of this section of the medical history is to elicit the practical difficulties that are posed by the patient’s asthma. It includes:
- Ways asthma symptoms disrupt the patient’s normal routine, such as the number of unplanned health visits (urgent care, ED, or hospitalization) and the number of days missed from school or work
- Limitations imposed by asthma, such as activities that cannot be undertaken and frequency of sleep disturbances
- Effect on growth, development, behavior, and school or work performance
- Issues related to impact on the family’s finances
- School characteristics that may interfere with adherence to treatment
Perception of the Disease by Patient and Family
As with all those who have chronic diseases, individuals with asthma must be the day-to-day managers of their medical care. This section of the history asks about:
- Patient’s, parents’, spouse/partner’s knowledge of the disease process and belief in the chronicity of asthma and efficacy of treatment
- Patient’s perception and beliefs regarding the use and long-term effects of medications
- Ability of the patient, parents, spouse/partner to cope with the disease
- Level of family support and the patient’s, parents’, spouse/partner’s capacity to recognize the severity of exacerbation
- Whether the patient and family can realistically carry out the current management plan
- Whether the current plan is economically affordable
(NACA, 2023)
CASE
PATIENT HISTORY
Deborah is a 24-year-old teacher’s aide who works in an elementary school. She has come to her healthcare provider’s office stating she has had a chest cold for 2 weeks and that it does not seem to be getting better. She also reports frequent bouts of coughing and bringing up thick, sticky mucus. She also says she has had some occasional wheezing and difficulty breathing. Her sleep has been disturbed at least three nights a week since this all started.
Following a physical examination, she is referred to the office nurse for a complete asthma assessment. The nurse has Deborah fill out an asthma screening questionnaire. Her responses indicate a family history of asthma, a personal history of allergies, worsening of coughing and wheezing during periods of humid weather and poor air quality, more frequent episodes of sleep disturbances over the past 2 months, and cigarette smoking, which she indicates she is trying to quit.
When asked about her work situation, Deborah notes that in addition to using a blackboard and chalk during the school day and “magic markers” to grade students’ papers, she is regularly exposed to first- and second-graders who come to school with coughs and colds. She adds that the school is located in an inner-city, low-income neighborhood not far from a factory with smokestacks that spew out thick, black smoke.
Following review of the assessment with her healthcare provider, Deborah is referred for lung function testing, and the results confirm a diagnosis of asthma.
Physical Examination
The physical examination of a patient with suspected asthma includes looking for specific evidence of atopy or allergic rhinitis:
- Eye exam
- Conjunctival congestion (redness, swelling, inflammation) or discharge
- Skin around the eyes, looking for signs of atopy or allergy:
- Allergic/ocular shiners (dark circles under the eyes caused by congestion of the nose and sinuses)
- Dennie’s lines (folds of skin below the lower eyelid caused by edema in atopic dermatitis)
- Nose interior and exterior
- Swollen or boggy normal structures (turbinates)
- Pale and violet-colored nasal mucosa due to allergic rhinitis
- Amount, color, and consistency of any nasal discharge
- Abnormal structures such as nasal polyps
- Foreign bodies (e.g., button, bead)
- Transverse nasal crease (“allergic salute”) across the lower third of the nose caused by constant upward wiping of the nose due to allergic rhinitis
- Oral cavity
- Postnasal drip (amount, color, consistency)
- Signs of inflammation of the throat
- Chest
- Shape and movement
- Increased anteroposterior diameter of chest in children due to hyperinflation, causing an abdominal breathing pattern
- Use of accessory muscles to breathe
- Prolonged expirations, inhalation period shorter than exhalation
- Lungs
- High-pitched musical wheezes most commonly heard during auscultation on expiration, crackles (rales), congestion, unequal breath sounds, or any other abnormal sounds
- Prolonged end-expiratory wheeze (in a child who is not sick, forced exhalation may reveal expiratory wheezing)
- Hyperresonance found during percussion, related to trapped air in the lungs

Allergic shiner in a pediatric patient. (Source: Fitzpatrick AM. CC SA 4.0.)
EXAMINATION DURING A MILD ASTHMA ATTACK
During a mild attack, patients may:
- Be breathless after physical activity such as walking into the office
- Still be able to speak in sentences and lie flat
- Be agitated
- Have increased respiratory rate, but accessory muscles are not required to breathe
- Have a pulse rate <100 beats per minute (bpm)
- Have moderate wheezing detectible upon auscultation of the chest but otherwise inaudible
- Have an oxygen saturation on room air >95%
EXAMINATION DURING A MODERATELY SEVERE ASTHMA ATTACK
During a moderately severe asthma attack, patients may:
- Be breathless and assume a sitting position while talking
- Have an increased respiratory rate
- Require accessory muscles to breathe
- Exhibit supraclavicular and intercostal retractions and nasal flaring in children
- Have abdominal breathing in children
- Have a pulse rate of 100–120 bpm
- Exhibit plainly audible expiratory wheezing
- Exhibit pulsus paradoxus (an exaggerated fall in systolic blood pressure during inspiration) of 10–20 mmHg
- Have an oxygen saturation on room air of 91%–95%
EXAMINATION DURING A SEVERE ASTHMA ATTACK
During a severe asthma attack, patients may:
- Be breathless during rest, sit upright, talk in words rather than sentences, and usually be agitated
- Have a respiratory rate often >30 per minute
- Require accessory muscles to breathe
- Have no interest in feeding
- Commonly exhibit suprasternal retractions
- Have a pulse >120 bpm
- Exhibit pulsus paradoxus (an exaggerated fall in systolic blood pressure during inspiration) of 20–40 mmHg
- Exhibit loud expiratory and inspiratory wheezing
- Have an oxygen saturation on room air <91%
- Assume a tripod position (sitting hunched over with hands supporting the torso) as severity increases
EXAMINATION DURING IMMINENT RESPIRATORY ARREST
When children are in imminent respiratory arrest, in addition to the symptoms mentioned above, they are drowsy and confused, but adolescents may not have these symptoms until they are in frank respiratory failure.
When a patient is experiencing status asthmaticus with imminent respiratory arrest, paradoxical thoracoabdominal movements in which the abdomen moves out with expirations occur. Wheezing may be absent due to severe airway obstruction, and severe hypoxemia presents with bradycardia. Pulsus paradoxus previously noted may now be absent, and this indicates respiratory muscle fatigue.
As the attack becomes more severe, there may be profuse diaphoresis along with a rise in pCO2 and hypoventilation. During such a severe episode, patients may struggle to breathe and become confused and agitated. They may try to remove their oxygen mask, complaining that they cannot breathe. These are all indications of life-threatening hypoxia (decreased oxygen reaching the tissues). As the CO2 level increases, breathing slows, the patient becomes somnolent, and there may be profuse diaphoresis. At this point almost no breath sounds may be heard, and the patient is now willing to lie flat (Morris, 2024a; Sharma, 2024).
PHYSICAL EXAMINATION OF CHILDREN
The physical examination of children is identical to that of the adolescent and adult, but one of the most important goals is to identify signs and symptoms that suggest an alternative diagnosis requiring further investigation. These include:
- Upper airway diseases: allergic rhinitis and sinusitis
- Obstructions involving large airways:
- Foreign body in trachea or bronchus
- Vocal cord dysfunction
- Vascular rings or laryngeal webs
- Laryngotracheomalacia, tracheal stenosis, or bronchostenosis
- Enlarged lymph nodes or tumor
- Obstructions involving small airways:
- Viral bronchiolitis or obliterative bronchiolitis
- Cystic fibrosis
- Bronchopulmonary dysplasia
- Heart disease
- Other causes:
- Recurrent cough not due to asthma
- Aspiration from swallowing mechanism dysfunction or gastroesophageal reflux
Diagnostic Testing
PULMONARY FUNCTION TESTS
The best objective measures of asthma are pulmonary (lung) function tests, which can quantify the degree of a patient’s airflow obstruction.
Spirometry is the most common pulmonary function test, employing a spirometer to measure the amount of air a patient can inhale completely and exhale completely as well as the rate of airflow through the airways. Spirometry assesses the unified mechanical function of the lung, chest wall, and respiratory muscles by measuring the total volume of air exhaled from a full lung, called the total lung capacity (TLC).
Spirometry is used to establish baseline lung function, evaluate dyspnea, detect pulmonary disease, monitor effects of therapies used to treat respiratory disease, evaluate respiratory impairment or disability, evaluate operative risk, and perform surveillance for occupation-related lung disease.
During the process, the technician applies a clamp to the patient’s nose to keep it shut. The patient is asked to inhale deeply and blow out as hard, as quickly, and as long as possible into the mouthpiece of the spirometer. The patient should exhale for at least 6 seconds, and at the end of the forced exhalation, the patient should again inhale as fully and as rapidly as possible. The forced vital capacity (FVC) should then be compared with the inhaled volume to verify that the forced expiratory maneuver did start from full inflation.
Before-and-after tests can also be used to monitor the effectiveness of various medications on a patient. Spirometric measurements before and 2 to 4 weeks after the patient begins a new drug can document the degree of improvement.

Child undergoing spirometry testing. (Source: 50Martin50, CC SA 3.0.)
For asthma, three basic lung characteristics are of clinical value:
- Forced vital capacity (FVC) is the total amount of air that can be forced quickly from the lungs after a complete inhalation.
- Forced expiratory volume in 1 second (FEV1) is the amount of air expired in the first second of forced exhalation. Airway obstruction is the most common cause of reduction in FEV1.
- FEV1:FVC ratio assesses airflow obstruction. When people with airway obstruction exhale, it takes longer than normal to empty the lungs. The amount of air expelled in 1 second, therefore, is reduced. The value of FEV1:FVC ratio goes down when a patient’s airways are narrowed.
(Lange-Vaidya, 2024; Mayo Clinic, 2024b)
Peak expiratory flow (PEF) meters are recommended for monitoring asthma in the home. PEF meters are inexpensive, handheld devices that record the maximum flow of air while a patient is forcefully emptying their lungs. Normal PEF values can vary according to a person’s sex, age, height, and race.

Peak expiratory flow (PEF) meters. (Source: Hosseman.)
USING A PEAK FLOW METER
When using a peak flow meter, the patient:
- Measures peak flow close to the same time each day
- Makes certain the sliding marker or arrow on the meter is at the bottom of the numbered scale before beginning
- Stands straight, takes in a complete breath, closes the lips tightly around the mouthpiece, and blows out as hard and as fast as possible until all air is emptied from the lungs
- Writes down the number the marker or arrow has reached along the numbered scale
- Repeats the steps above two more times
- Records the highest reading of the three, which is called the patient’s predicted normal value, or “personal best”
| Zone | Measurement | Finding |
|---|---|---|
| (ALA, 2024a) | ||
| Green | 80%–100% of patient’s normal | Asthma is under control. |
| Yellow | 50%–80% of patient’s normal | Rescue medicines should be used; a medical visit may be needed. |
| Red | <50% of patient’s normal | Signals a medical alert; emergency care is needed. |
Body plethysmography, also known as a lung volume test, measures the amount of air the person can hold in the lungs and the amount of air that remains after forced exhalation. It is used to determine whether exposure to substances in the home or workplace have caused lung damage and whether there is a need for a change in treatment (Cleveland Clinic, 2022b).
Gas diffusion testing or diffusing capacity of the lung for carbon monoxide (DLCO) determines how well the alveoli are delivering oxygen to and removing carbon dioxide from the blood into the capillaries surrounding them. The person inhales air containing a very small amount of carbon monoxide and a tracer gas (such as methane or helium), holds the breath for 10 seconds, and then rapidly exhales. The exhaled gas is tested to determine how much of the tracer gas was absorbed during the breath. Another name for this test is lung diffusion testing (NIH, 2023).
FRACTIONAL EXHALED NITRIC OXIDE TESTING (FeNO)
FeNO testing can help determine how much inflammation is present in the airways. It does not test directly for asthma but can assist in confirming an asthma diagnosis in adults and children ages 5 and older. It is also done if spirometry cannot be performed. Exhaled nitric oxide testing is technically complex and is not routinely used in monitoring (Morris, 2024b).
CHILDREN AND LUNG FUNCTION TESTING
Most children who have asthma develop their first symptoms before 5 years of age. Asthma in children ages 0–5 years, however, can be hard to diagnose since spirometry is not usually done in children younger than 6 years because of the difficulties in obtaining reliable forced expiratory maneuvers in this age group.
Alternative measurements that require less patient cooperation have been developed for use in young children; however, they are not widely available. These alternatives include:
- Interrupter technique (Rint) measures airway resistance, including lung airways and rib cage during tidal breathing (normal, restful breathing). The method is based on transient interruption of airflow at the mouth for a brief period during which alveolar pressure and mouth pressure reach equilibrium, and the pressure change at the mouth can be used to calibrate the resistant of the airways.
- Forced oscillation technique (FOT) and impulse oscillometry system (IOS) are both widely used in pediatric settings. They are noninvasive techniques performed during tidal breathing, requiring only minimal cooperation from the patient. FOT and IOS assess bronchial hyperresponsiveness by employing small-amplitude pressure oscillations superimposed on normal breathing.
- Multiple breath washout (MBW), also referred to as gas dilution, measures the clearance of a gas from the lungs. It is performed during tidal breathing, during which a marker gas, usually helium, less frequently nitrogen, is washed out with 100% oxygen. Preschool children perform the test in a seated position, and a video can be used for distraction and to promote a regular breathing pattern.
- Single-breath counting (SBC) is a novel technique for measuring pulmonary function in children. SBC is the measurement of how far the child can count using a normal speaking voice after one maximal-effort inhalation. The count is in cadence to a metronome that is set at two beats per second. SBC has been found to correlate well with standard measures of pulmonary function.
(Rosen & Colin, 2024; Morris, 2024a)
BRONCHODILATOR TESTING AND BRONCHIAL PROVOCATION
Among the features of asthma that vary from individual to individual is the innate degree of hypersensitivity of the patient’s airways. In some patients, a small amount of irritation triggers a severe reaction. Other patients, however, are less sensitive and experience much less bronchoconstriction with the same amount of irritation.
Bronchodilator testing is recommended in almost all adult and adolescent patients with airflow limitation on their baseline spirometry. Acute reversibility of airflow obstruction is tested by administering two to four puffs of a quick-acting bronchodilator (e.g., albuterol) using a valved holding chamber (spacer) and repeating spirometry 10 to 20 minutes later. Measurements can also be made before and after administration of a nebulized bronchodilator.
A positive bronchodilator response, however, is not sufficient to make the diagnosis of asthma, as the response may be seen with other conditions such as COPD. Asthma is normally distinguished from these other conditions by the capacity for a large increase in FEV1. The definition of large response, however, is not standardized.
Bronchoprovocation is useful for diagnosing asthma in patients with normal baseline airflow. It can be used to identify or exclude airway hyperresponsiveness in patients with an atypical presentation or isolated symptoms of asthma, especially cough. Several types of bronchoprovocation testing are available to assess airway responsiveness in specific patient situations. These may include:
- Pharmacologic drugs to cause narrowing of the airways, including methacholine or mannitol
- Exercise challenge
- Eucapnic voluntary hyperpnea, which mimics the effect that prolonged exercise has on the airway
- Food additive challenge
- Antigen challenge
During this test, a direct provocative stimulus is used to stimulate bronchoconstriction. People with asthma are more sensitive to such stimuli than those without asthma. Although these challenges are very safe, they may make the patient feel dizzy or uncomfortable and can cause symptoms of an asthma attack.
A positive bronchoprovocation test is not entirely specific for asthma. False-negative results are uncommon, and a negative test performed in a patient off of asthma controller therapy does reliably exclude the diagnosis of asthma.
Other specialized testing can be used when assessing for exercise-induced bronchoconstriction as well as evaluation for possible occupational asthma by obtaining measurements before and after a work shift (Irvin, 2024; ALA, 2023b).
ALLERGY TESTING
Many persons with asthma have atopy. In these people, allergic reactions from inhaled biologic substances will increase their sensitivity to asthmatic triggers. The best protection from this increased sensitization is for the patient to avoid inhaling the allergens, and to do this, patients must identify the allergens that cause them trouble.
As a first step in building a list of probable offending allergens, the patient keeps a diary of exposures and symptoms. The second step is allergy testing to verify or reject at least some of the suspected allergens. Ridding a patient’s environment of offending allergens can be time-consuming and expensive, and allergy testing will indicate which specific types of cleaning and avoidance should be worth the effort.
Allergy testing can be done in vivo and in vitro.
In Vivo Tests (Skin Tests)
In vivo tests are quick, fairly reliable, and cost-effective. There are three common methods of allergy skin testing.
In a skin prick test (also called a puncture or scratch test), a series of tiny drops of allergens is placed on the skin, and the skin underneath each drop is pricked with a needle or lancet so that the allergen will penetrate beneath the skin surface. Several allergens can be tested at the same time. If the person has an allergy to an allergen, a dime-sized wheal will appear at the prick site and will be red and itchy. In adults, the test is usually done on the forearm; children may be tested on the upper back.

Skin prick test for allergies. (Source: National Institutes of Health.)
If the skin prick test is negative, an intradermal test may be done, in which the allergen is injected into the skin. This test is more likely to be used to find out if the patient is allergic to bee venom or a drug (e.g., penicillin). Or it may be used if the skin prick test was negative and the clinician still thinks the patient is allergic to the allergen.
Another type of skin testing is the patch test, in which an allergen is applied to a patch and placed on the skin, where it remains for 48 hours. The clinician looks at the area in 72 to 96 hours, and if the skin has become red, irritated, and itchy, the results may indicate an allergy (NIH, 2022).

Intradermal skin testing for allergies. (Source: Wikimedia, CC SA 2.0.)
Intradermal testing carries a slightly higher risk of provoking significant allergic reactions than other methods. In rare instances a patient can have a severe, immediate allergic reaction (anaphylaxis) and require emergency management.
Intradermal tests can also be more accurate than skin prick and patch tests, but sometimes they may be falsely positive. In some cases, a person may have a positive response to a substance but have no problems with that substance in everyday life. Also, if the dose of allergen is large, even people who are not allergic to it can have a positive reaction (Mustafa & Ramsey, 2021; Mayo Clinic, 2024d; WebMD, 2024).
In vivo allergy testing is not without risk. In some people, an area of swelling, redness, and itching may develop hours after the test and persist for as long as a couple of days. Other possible side effects include pain or bleeding at the injection site, dizziness, or lightheadedness during testing.
In Vitro Tests
In vitro tests use a blood sample from the patient to detect circulating IgE antibodies to specific allergens.
The most commonly used in vitro tests are immunoassays, which include the enzyme-linked immunosorbent assay (ELISA or EIA) and variations on this technique (fluorescent enzyme immunoassays [FEIA] and chemiluminescent immunoassays).
A positive immunoassay test confirms only the presence of the antibody, but actual reactivity must be determined by the patient’s history or by a supervised challenge. An allergen-inhalation challenge is performed in specialized centers able to handle potentially significant reactions. This test is often needed to help diagnose occupational asthma.
Skin testing is preferred over in vitro testing because it is quicker, less expensive, and more sensitive, and does not require submitting a blood sample. In certain circumstances, however, in vitro testing is advantageous over skin testing because it does not pose a risk of an allergic reaction. It is used in older adults with cardiovascular disease, patients with sensitivities to allergens that are associated with severe anaphylactic reactions, and patients with histories of severe reaction to very small amounts of the allergen.
Immunoassays are valid for infants as young as 6 weeks and can be performed on capillary blood samples. In vitro tests may be preferable for those with skin conditions, such as widespread and severe atopic dermatitis, or dermographism (exaggerated weal and flare response occurring within minutes of skin being stroked or scratched). In vitro tests are often indicated to confirm negative skin tests. Another advantage is that in vitro tests are not affected by medications that might cause confusion with skin testing.
Immunoassays are available for:
- Foods
- Insect venoms
- Environmental allergies such as pollen, dust mites, or cockroaches
- Natural rubber latex
- Some beta-lactam drugs such as penicillin or cephalosporins
- Some occupational allergens
(Kowal & DuBuske, 2024)
LABORATORY DATA
Laboratory studies are not usually a major part of diagnosing or following asthma, but a few tests can give supportive evidence and may be used to exclude other diagnoses. These tests include:
- CBC (complete blood count), to screen for eosinophilia or significant anemia and to evaluate blood cells to provide information on infection and inflammation
- Alpha-1 antitrypsin level, for lifelong nonsmokers to exclude emphysema
- Comprehensive metabolic panel, to evaluate overall body organ function, including kidney, liver, and lungs
- Sweat test or trypsin/chymotrypsin, to rule out cystic fibrosis in both children and adults
- AFB tuberculin testing, to rule out tuberculosis and nontuberculous mycobacteria
- Lung biopsy, to evaluate lung tissue for damage and for cancer
(Cahill, 2024; Lange-Vaidya, 2024)
Other laboratory tests related to asthma may include:
- Blood gases (ABGs) during severe asthma attacks, to predict respiratory failure and the consequent need for mechanical ventilation (only patients whose oxygenation is not restored to over 90% with oxygen therapy require an ABG)
- Sputum cultures, to diagnose lung infections caused by bacteria
- Sputum cytology, to assess for the increased concentration of eosinophils and neutrophils that occurs in patients with asthma
(Morris, 2024b)
PULSE OXIMETRY
Pulse oximetry (PO) measures the percentage of hemoglobin that is carrying oxygen to determine hypoxemia in patients with acute asthma. PO is often used in children to grade the severity of an acute asthma exacerbation and to determine whether the child requires hospitalization.
A pulse oximeter device is placed on the finger, nose, toe, earlobe, or forehead, and a beam of light is passed through to the blood in the capillaries. The amount of oxygen in the blood is measured, along with the pulse rate (ALA, 2023e).
A pulse oximetry reading should always be considered an estimate of oxygen saturation. Therefore, numbers from a pulse oximeter should not be used in isolation. A reading may be anywhere from 2% to 4% higher or lower than the actual oxygen level in the arterial blood.

A finger-mounted pulse oximeter with pulse bar taking measurements through the fingernail. (Source: Thinkpaul, CC SA 3.0.)
FDA ALERT
In February 2021, the FDA issued an alert on limitations of pulse oximeters. The pulse oximeter may not give accurate or consistent readings in persons with poor circulation, dark skin pigmentation, thick skin, current tobacco usage, cool skin temperature, dark fingernail polish, long artificial nails, or soiled fingers (U.S. FDA, 2021). As a result, people with dark skin may have low oxygen saturation levels that go unnoticed and untreated. Recent research suggests that these inaccurate pulse oximetry readings can lead to poor clinical outcomes (Jamali et al., 2022).
An oxygen saturation (SpO2) reading of 95% or higher is normal for a healthy individual. A reading of 91%–95% is clinically acceptable but low and may be due to the patient being a smoker. Readings from 70% to 90% are unsafe levels and indicate hypoxemia. Less than 70% indicates extreme lack of oxygen. However, clinical correlation is always necessary, since the exact cutoff below which tissue hypoxia ensues has not been defined.
IMAGING STUDIES
A chest X-ray is valuable for revealing complications or alternative causes of wheezing. It is usually more useful in the initial diagnosis of asthma than in the detection of exacerbation, although it is valuable in excluding complications, including pneumonia and asthma mimics, even during exacerbation.
In most patients with asthma, chest X-ray findings are normal or may indicate hyperinflation. Because pneumonia is one of the most common complications of asthma, chest X-ray is indicated in those with fever to rule out pneumonia.
For diagnostic purposes, atypical presentations, and hospital admissions, chest X-rays should be taken. In asthma, X-rays can show the presence of superimposed infections, atelectasis (collapse of an expanded lung), or pneumothorax (abnormal presence of air in the pleural cavity, leading to collapse of the lung). Chest films may also help to distinguish asthma from allergic bronchopulmonary aspergillosis, sarcoidosis, congestive heart failure, pulmonary emboli, foreign body aspiration, and lung cancer (Morris, 2024b).
High-resolution CT (HRCT) is a second-line examination useful for patients with chronic or recurring symptoms and those with possible complications, such as allergic bronchopulmonary aspergillosis and bronchiectasis. Findings in bronchial asthma include:
- Bronchial wall thickening
- Bronchial dilatation
- Cylindrical and varicose bronchiectasis
- Reduced airway luminal area (the major determinant of airway resistance)
- Mucoid impaction of the bronchi
- Centrilobular opacities, or bronchiolar impaction
- Linear opacities
- Air trapping, as demonstrated or exacerbated with expiration
- Mosaic lung attenuation, or focal and regional areas of decreased perfusion
(Morris, 2024b)
ECG
ECG is done to determine whether the heart is the cause of severe asthma symptoms, such as irregular heartbeat, an enlarged heart, or previous damage to the heart muscle. It is also done to determine if the patient’s heart is healthy enough for medications that may be prescribed for asthma management (Asthma UK, 2022a).
Patients who are severely symptomatic should have ECG monitoring. Sinus tachycardia and ECG evidence of right heart strain are common in patients with acute asthma (Morris, 2024b).
NUCLEAR IMAGING
Technetium-99m DTPA radioaerosol lung scintigraphy is a classic technique that shows the extent of major airway distribution, peripheral distribution, and absorption in the oronasal air passages. Ventilation scanning has been used as an indicator of ventilation defects in asthmatic children as well as to assess distribution of aerosol and particulates from asthma medications (Morris, 2024b).
24-HOUR pH PROBE
A 24-hour pH probe can be used to help diagnose GERD if a patient is not being managed effectively with asthma therapy. This is an outpatient procedure done to measure the pH or amount of acid that flows into the esophagus from the stomach (Morris, 2024b).
Classifying Asthma Severity
There are two methods for classifying asthma severity:
- The Global Initiative for Asthma (GINA) Guidelines classify asthma according to the treatment requirements that are necessary to control symptoms; thus, severity is assigned in a retrospective manner.
- The National Asthma Education and Prevention Program (NAEPP) Guidelines classify asthma based on signs and symptoms in three age groups: 0–4 years, 5–11 years, and 12 years and older. (These classifications were included in the NAEPP “Guidelines for the Diagnosis and Management of Asthma 2007” report [NAEPP, 2007] and have not been revised since that time. However, the NAEPP acknowledged in their 2020 report [NAEPP, 2020] that asthma severity must be updated to include asthma phenotypes and endotypes.)
| Asthma Classification | Based on Treatment Requirements | |
|---|---|---|
| (GINA, 2024) | ||
| Mild | Well controlled with low-intensity therapy, such as low-dose inhaled corticosteroid (ICS)-formoterol or with low-dose controller treatment such as low-dose ICS plus as-needed short-acting beta-2 agonist (SABA) | |
| Moderate | Well controlled with low- or medium-dose maintenance ICS-formoterol | |
| Severe | Uncontrolled asthma despite high-dose ICS-LABA or requires high-dose ICS-LABA to prevent uncontrolled asthma | |
| Asthma Classification | Based on Signs and Symptoms* |
|---|---|
| *In individuals who are not receiving long-term control medications (NAEPP, 2007) |
|
| Intermittent |
|
| Mild persistent |
|
| Moderate persistent |
|
| Severe persistent |
|
| Asthma Classification | Based on Signs and Symptoms* |
|---|---|
| *In individuals who are not receiving long-term control medications
(NAEPP, 2007) |
|
| Intermittent |
|
| Mild persistent |
|
| Moderate persistent |
|
| Severe persistent |
|
| Asthma Classification | Based on Signs and Symptoms* |
|---|---|
| *In individuals who are not receiving long-term control medications
(NAEPP, 2007) |
|
| Intermittent |
|
| Mild persistent |
|
| Moderate persistent |
|
| Severe persistent |
|
ASTHMA TREATMENT
The goals of treatment for asthma include:
- Preventing long-term symptoms that interfere with daily living
- Maintaining lung function near the person’s personal best measurement
- Preventing repeated asthma exacerbations
- Providing the best medical treatment with the fewest possible side effects
The cornerstones to prevent exacerbations and control symptoms include pharmacologic and nonpharmacologic interventions:
- ICS-containing medication for everyone with asthma, including individuals with infrequent symptoms, to reduce the risk of serious exacerbations.
- Reliever inhaler for everyone with asthma, either ICS-formoterol, ICS-SABA, or SABA. The preferred reliever inhaler is low-dose ICS-formoterol to reduce the risk of severe exacerbations as opposed to a SABA reliever. ICS-formoterol should not be the reliever by individuals who take a different maintenance ICS-LABA. In this case, the reliever should be SABA or ICS-SABA.
- Treating modifiable risk factors (such as exposure to smoking, allergens, or air pollution) and comorbidities (such as obesity, GERD, food allergy, anxiety, depression, pregnancy, and chronic rhinosinusitis).
- Nonpharmacologic therapies such as smoking cessation, physical activity, investigation for occupational asthma, and aspirin-exacerbated respiratory disease.
(GINA, 2024)
The routes of delivery for asthma medications are systemic (oral or injectable) and inhaled. The inhaled route is more convenient and is used most commonly because of fewer side effects and quicker onset of action.
There are three types of asthma medicines:
- Reliever medicines work quickly and are taken as needed at the first sign of breakthrough symptoms, including worsening or exacerbations of asthma.
- Controller medicines treat asthma by correcting the underlying changes in the airways, such as swelling and mucus hypersecretion; they can be combined with other medications. (Per GINA track 1, controller treatment is via low-dose ICS-formoterol administered when symptoms occur and before exercise or allergen exposure. In steps 3–5, a maintenance controller is added as once- or twice-daily ICS-formoterol. This is called maintenance and reliever therapy.)
- Add-on therapies for severe asthma include long-acting muscarinic antagonists (LAMAs), leukotriene receptor antagonists (LTRAs), low-dose azithromycin, and biologic agents.
(GINA, 2024)
(See also “Treatment Tracks” later in this course.)
Drug Administration: Inhalation
Many asthma drugs are administered by inhalation to send the medication directly to the target tissue, the inner linings of the airways of the lung. Higher concentrations of medicine can be delivered this way with fewer systemic side effects.
TYPES OF AEROSOL DEVICES
A variety of devices are available for delivering drugs directly into the lungs. The common aerosol devices are described below.
Nebulizer
A nebulizer is a drug delivery device used to change medication from a liquid to a mist so that it can be more easily inhaled into the lungs through a mouthpiece or mask worn over the nose and mouth. A nebulizer is the most common device used to deliver medications to infants, small children, and patients requiring hospitalization.
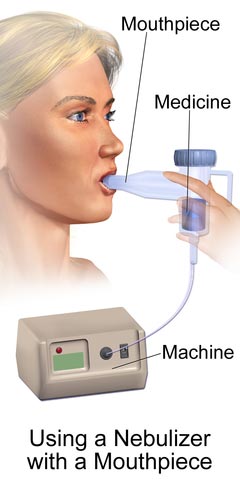
(Source: BruceBlaus, CC SA 4.0 International.)
Metered-Dose Inhaler (MDI)
An MDI is a pressurized canister containing medication that fits into a boot-shaped mouthpiece. The canister is activated by compressing it into the boot, which delivers a metered dose of the drug to be inhaled. This is the most common device used to deliver medications in an ambulatory setting.

Metered-dose inhaler (MDI). (Source: NIAID, CC 2.0 Generic.)
Spacers, or valved holding chambers (VHCs), are often used with non-breath-activated MDIs to minimize local side effects and enhance drug delivery. A spacer is a simple tube added to the mouthpiece of an MDI to move the inhaler farther from the patient’s mouth. A VHC is a spacer with a one-way valve that keeps the patient from exhaling into the MDI.

Child using inhaler with spacer. (Source: Michael J. Ermarth, FDA.)
Dry Powder Inhaler (DPI)
This device does not use a chemical propellant to push the medication out of the inhaler. Instead, the medication is released through the mouthpiece by deep and fast inspiration. A DPI is not indicated for use in young children because of the requirement of a high inspiratory flow.

Dry powder inhalers (left to right): Turbuhaler, Accuhaler, Ellipta devices. (Source: NIAID, CC SA 4.0 International.)
Soft Mist Inhaler (SMI)
A soft mist inhaler is a newer type of device that creates a cloud of medicine that is inhaled without the assistance of a propellant. Because the mist contains more particles than MDIs and DPIs and the spray leaves the inhaler more slowly, more of the drug enters the lungs (Hess & Dhand, 2024).
PROPER USE OF INHALERS
It is important to read the device-specific instructions for proper use of any inhaler if it is to be effective. The following are general instructions for use of inhalers.
Most asthma patients use MDIs for their reliever medications. It is easiest to learn the proper use of an MDI through an in-person demonstration. All patients who are prescribed medications using inhalers should receive initial instructions and careful follow-up to ensure proper use.
These are the essential steps whether or not a spacer or VHC is used:
- Take the cap off, inspect to make certain mouthpiece and spray hole are clean, and shake the inhaler well.

- Take a breath in and fully exhale the air in the lungs.

- Hold the inhaler upright with finger on the top of the canister and thumb holding the bottom of the inhaler.

- Put the inhaler in the mouth above the tongue and between the teeth. Seal lips around the inhaler. Close the lips around the mouthpiece (closed-mouth technique) or hold the mouthpiece 1 to 2 inches in front of the open mouth.

- Begin to breathe in slowly. Press down on the inhaler one time and keep breathing in.

- Hold the breath for 5 to 10 seconds.

- Open the mouth and breathe out slowly.

(Source: CDC, 2018; GINA, 2024.)
If taking two puffs of the reliever medication, wait 15–30 seconds and shake the inhaler again before taking the second puff. For other medicines it is not necessary to wait before taking the prescribed number of puffs. If using a steroid inhaler, rinse the mouth with water, gargle, and spit out the water (Hess & Dhand, 2024).
When using a dry powder inhaler, the steps are the same; however, the inhaler is activated when the person inhales, not by pressing down on a tube.
INHALER CLEANING
It is important to keep the inhaler clean. Any powder in or around the hole where the medicine sprays out should be cleaned.
- Remove the metal canister from the L-shaped plastic mouthpiece. Do not wash the canister or immerse it in water.
- Rinse only the mouthpiece and cap by running warm tap water through them for 30–60 seconds.
- Shake off excess water and allow the mouthpiece and cap to air dry overnight.
- In the morning, put the canister back inside. Put the cap on.
- Replace the mouthpiece cover.
- If it is necessary to use the inhaler before the mouthpiece is dry, shake off excess water, replace canister, and test spray two times (away from the face).
- Follow the manufacturer’s instructions for cleaning a dry powder inhaler.
(Hess & Dhand, 2024)
INHALER MISUSE
Incorrect inhaler use can result in poor asthma control, an increased risk for exacerbations of symptoms, and increased adverse medication effects. In fact, up to 80% of individuals in the community demonstrate poor inhaler technique. Since most individuals who do not use an inhaler properly do not know they are using incorrect technique, inhaler technique should be observed frequently during patient encounters (GINA, 2024).
GINA guidelines (2024) recommend the use of a standardized checklist to check inhaler technique to improve asthma control in children and adults. The healthcare provider should watch the individual use an inhaler, make corrections, and recheck technique. Since inhaler technique declines over time, a check of inhaler technique should be done frequently
For MDI users, common errors involve coordination, speed and/or depth of inspiration, and postinhalation breath hold. Common errors among dry-powder inhaler users are incorrect preparation, no full expiration after inhalation, and no postinhalation breath hold (Asthma UK, 2024c).
Incorrect inhaler technique is linked to a significantly greater risk for inhaled corticosteroid overuse. Unintentional nonadherence to first-line rescue inhalers can lead to use of long-acting inhaled medications that might not otherwise be needed. Improper use of inhaled corticosteroids can increase the risk of pneumonia and other direct and indirect complications. These findings highlight the importance of inhaler technique training.
CASE
INHALER EDUCATION
Kamiko is a 35-year-old woman who has recently been diagnosed with asthma and has returned for her second follow-up appointment. She has an appointment with the office nurse to receive additional education on controlling her disease. During the visit her medications are discussed and reviewed, as well as the new asthma action plan developed between herself and her primary care physician.
When Kamiko was newly diagnosed with asthma and prescribed a rescue inhaler, she was given training in the proper use of the inhaler and was able to demonstrate proper technique and understanding of care of the device. Today before Kamiko leaves the office, the nurse asks her to demonstrate the use of her inhaler again. A dummy inhaler is provided, and as the nurse watches, Kamiko proceeds through the steps.
Following her demonstration, the nurse points out three problems with Kamiko’s technique. First, she did not fully exhale all the air in her lungs before inhaling the medication. Secondly, she did not shake the inhaler again before administering a second dose. And lastly, she did not begin to inhale until she had sprayed the medicine into her mouth.
The nurse next demonstrates the proper technique for Kamiko, who then returns the demonstration, showing that she can now use her inhaler correctly. She is given a pamphlet to refer to at home that visually guides her through the technique, and another follow-up appointment is made with the nurse for reevaluation in 2 weeks.
Bronchodilators
Bronchodilators are used to reverse the bronchoconstriction of asthma attacks and in this way to relieve cough, wheezing, dyspnea, and chest tightness. Bronchodilators are also the primary medicine for preventing exercise-induced bronchoconstriction. There are three classes of bronchodilators:
- Beta-2 agonists
- Anticholinergics
- Methylxanthines
SHORT-ACTING BETA-2 AGONISTS (SABAs)
Short-acting beta-2 agonists are reliever medications, often referred to as quick-relief or rescue medications. The smooth muscle in bronchioles (small airways) is relaxed by beta-2 adrenergic agonist drugs, reversing and preventing further contraction of muscle cells.
Because beta-2 agonists have a wide array of effects throughout the body, they are preferably administered by inhalation directly to the inner lining of the airways. When inhaled, they produce an effect in less than 5 minutes and the effect then lasts for 2–4 hours. For safety, SABAs should not be used alone in the treatment of asthma (GINA, 2024).
| Generic Name | Brand Name |
|---|---|
| Albuterol |
Proventil HFA Ventolin HFA Proair HFA Proair RespiClick Proair Digihaler AccuNeb solution |
| Levalbuterol |
Xopenex Xopenex HFA Levalbuterol HFA |
| Terbutaline (oral) | None |
Side effects:
- Tachycardia
- Tremors
- Jitteriness
- Palpitations
Precautions:
- Patients with heart disease, hyperthyroidism, seizure disorder, or hypertension should be closely monitored.
LONG-ACTING BETA-2 AGONISTS (LABAs)
LABAs are recommended for use only in conjunction with inhaled steroids in asthma. Long-acting bronchodilators are used to provide control, not quick relief of asthma. They should only be used with inhaled steroids for long-term control of asthma symptoms (GINA, 2024).
| Generic Name | Brand Name |
|---|---|
| Formoterol fumarate inhalation powder | Foradil |
| Salmeterol | Serevent Diskus |
| Olodaterol | Striverdi Respimat |
ANTICHOLINERGICS
Another group of bronchodilators, anticholinergics, are muscarinic receptor antagonists (parasympatholytics). They are used along with beta-2 agonists for treatment of severe symptoms. They are not, however, intended for acute asthma attacks.
Whereas beta-2 agonists affect the bronchioles (small airways), anticholinergics affect the muscles around the bronchi (large airways) by blocking receptors that cause spasm and by decreasing secretion of mucus. Anticholinergics begin to work within 15 minutes, work best after 1–2 hours, and usually last from 3 to 4 hours, or up to 6 hours in some people.
| Generic Name | Brand Name |
|---|---|
| Ipratropium bromide | Atrovent HFA |
| Long-acting tiotropium | Spiriva Respimat |
| Umeclidinium | Anora Ellipta Incruse Ellipta |
Side effects:
- Dry mouth
Precautions:
- Individuals with glaucoma should be carefully monitored by an ophthalmologist.
- Persons with allergy to soya lecithin (e.g., soybeans, peanuts) should not take these drugs.
(Schiffman, 2022)
METHYLXANTHINES
Methylxanthines belong to the class of bronchodilators that includes caffeine. These drugs have two distinct effects in the airways: smooth muscle relaxation and suppression of the response of airways to stimuli. They also have an effect on mucus clearance. Methylxanthines can be helpful for relief of nighttime asthma symptoms.
Theophylline is an alternative, but not preferred, therapy in mild to moderate persistent asthma. It is usually reserved as an add-on or third-line therapy, most often in combination with inhaled therapy, and its use requires monitoring of plasma concentrations so that therapeutic but not toxic levels are achieved. Oral theophylline is not recommended in the treatment of asthma. While low-dose sustained-release theophylline may be used as a treatment option, there are concerns about low efficacy, high risk of adverse effects, and safety (GINA, 2024). Intravenous theophylline is not recommended by GINA (2024) for use in asthma exacerbations due to low efficacy and safety concerns.
Aminophylline is a combination of theophylline and ethylenediamine in a 2:1 ratio. This medication is used as a second- or third-line adjunct treatment for asthma (ethylenediamine is an additive that increases pH sufficiently enough to dissolve theophylline). Aminophylline in the intravenous form is not recommended by GINA (2024) for use in asthma exacerbations due to low efficacy and safety concerns.
| Generic Name | Brand Name |
|---|---|
| Theophylline (long acting) | Theo-24 |
| Theophylline and dextrose injectable | None |
| Aminophylline (injectable) | None |
Methylxanthines have a narrow therapeutic range and thus a high incidence of adverse effects.
Mild side effects:
- Nausea and vomiting
- Increased gastric acid secretion and subsequent GERD
- Polyuria
- Insomnia
- Palpitations
- Headache
- Tremors
- Weakness
Severe side effects:
- Intractable vomiting
- Arrhythmias
- Tachycardia or bradycardia
- Cardiac arrest
- Allergic skin reactions
- Seizures
Precautions:
- Because theophylline is related to caffeine, ingesting large amounts of caffeine in coffee, tea, chocolate, or soft drinks may increase theophylline side effects.
- Some drugs, such as cimetidine (Tagamet), erythromycin (E.E.S.), and ciprofloxacin (Cipro), may increase theophylline levels.
- Certain diets, such as high protein/low carbohydrate or vice versa, may change the effect of theophylline.
- Phenytoin (Dilantin) and carbamazepine (Tegretol) may decrease theophylline levels.
Contraindicated for people with:
- Cardiovascular disease
- Cystic fibrosis
- Hepatic impairment
- Hypo- or hyperthyroidism
- Peptic ulcer disease
- Seizure disorder
- Pregnancy and breastfeeding
Corticosteroids
Corticosteroids are variants of the natural hormone cortisol. Corticosteroids dampen inflammation at the level of cell nuclei, switching off genes for inflammatory molecules such as cytokines, chemokines, and inflammatory enzymes, and activating genes that have anti-inflammatory effects.
INHALED CORTICOSTEROIDS
Inhaled corticosteroids (ICSs) are considered the most potent and consistent anti-inflammatory agents currently available for preventing exacerbations in patients with persistent asthma. Regular use of these medications reduces the frequency of asthma symptoms, bronchial hyperresponsiveness, and risk of serious exacerbation, and improves quality of life.
ICSs work directly at the cellular level by reversing capillary permeability and lysosomal stabilization to reduce inflammation. The onset of action is gradual and may take from several days to several weeks for maximal benefit with consistent use. Recently updated guidelines recommend ICSs be used for acute asthma symptoms in conjunction with beta-2 agonists in adolescents and adults.
ICSs come in liquid capsule formulation given through a nebulizer machine, metered-dose inhalers (MDIs) administered through spacers, and dry powder inhalers (DPIs). These medications are initiated in a stepwise fashion based on the frequency and severity of asthma symptoms. Low-, medium-, and high-dose inhaled corticoids are available to treat mild, moderate, and severe persistent asthma (Liang & Chao, 2023).
| Generic Name | Brand Name |
|---|---|
| Beclomethasone dipropionate | QVAR Redihaler |
| Budesonide | Pulmicort Flexhaler Pulmicort Respules |
| Fluticasone propionate |
Flovent HFA Flovent Diskus Advair HFA+ Arnuity Ellipta ArmonAir Digihaler ArmonAir RespiClick |
| Mometasone | Asmanex HFA Asmanex Twisthaler |
| Ciclesonide | Alvesco |
Side effects:
- Mouth and throat irritation
- Dysphonia
- Oral yeast infections
- Reflex cough
- Bronchospasm
- Risk of bone fractures with high doses
Precautions:
- ICSs may decrease growth in children, so the lowest dose possible should be prescribed.
- ICSs may increase risk of serious or fatal infections in those exposed to serious viral infections (e.g., chickenpox, measles).
- ICSs can cause cataracts or glaucoma.
- ICSs can increase the risk of pneumonia.
- Symptomatic patients on long-term, high-dose ICS should be screened for:
- Cataracts
- Glaucoma
- Hypothalamic-pituitary-adrenal axis dysfunction
- Impaired glucose metabolism
Contraindications:
- There are very few absolute contraindications to ICS. These include hypersensitivity to the medications and severe hypersensitivity to milk proteins/lactose.
INHALED COMBINATION MEDICATIONS
An asthma combination inhaler combines two or three medications, which can ease hyperresponsiveness of airways and help prevent an asthma attack. They are used for the long-term control of asthma symptoms.
| Generic Name | Brand Name |
|---|---|
| Formoterol (LABA) and budesonide (ICS) | Symbicort |
| Formoterol (LABA) and mometasone (ICS) | Dulera |
| Salmeterol (LABA) and fluticasone (ICS) | Advair Diskus Advair HFA |
| Vilanterol (LABA) and fluticasone (ICS) | Breo Ellipta |
| Vilanterol/umeclidinium (anticholinergic) and fluticasone (ICS) | Trelegy |
SYSTEMIC CORTICOSTEROIDS
Systemic corticosteroids, whether administered intravenously or orally, are a key treatment for moderate or severe episodes of asthma. For patients whose asthma attacks do not resolve promptly after inhalation of their reliever medicines, systemic corticosteroids will speed the widening of airways and make a near-term recurrence less likely.
In emergency settings, intravenous corticosteroids are used, and sometimes oral systemic steroids are taken in high doses for several days. This is referred to as a steroid burst.
Oral steroids can also be used to control symptoms in people with severe persistent asthma. When used for this purpose, the drug is taken daily at a lower dose than is used during an asthma exacerbation. The smallest possible dose should be given to avoid long-term effects. Some people can control their symptoms with every-other-day dosing.
| Generic Name | Brand Name |
|---|---|
| Oral prednisone | Prednisone Intensol Rayos |
| Oral prednisolone | Orapred ODT Pediapred Prelone Medrol |
| Injectable methylprednisolone | Dep-Medrol Solu-Medrol |
| Oral methylprednisolone | Medrol |
| Injectable triamcinolone |
Kenalog Aristospan Triesence |
Side effects with short-term use:
- Weight gain (fat deposits in abdomen, face, nape of neck)
- Fluid retention
- Upset stomach
- Hypertension
- Mood swings
- Memory or behavior problems
- Confusion or delirium
Side effects with long-term use:
- Growth suppression
- Hyperglycemia
- Cataracts
- Glaucoma
- Osteoporosis and fractures
- Thin skin, bruising, and slower healing
- Muscle weakness
- Increased risk for infections
- Adrenal gland hormone suppression
- Severe fatigue
- Loss of appetite
- Nausea
- Muscle weakness
Precautions:
- When taking steroids chronically, they should not be abruptly discontinued; tapering the drug allows the adrenal glands time to return to normal secretion patterns.
- Any acute infections should be treated and fully resolved before starting oral corticosteroids.
- Avoid use in patients with adrenal insufficiency.
- Use with caution in people with glaucoma/cataracts and osteoporosis.
- Patients may experience withdrawal symptoms, including:
- Weakness
- Fatigue
- Body aches
- Joint pain
- Decreased appetite
- Nausea
- Lightheadedness
- Irritability or mood swings
Leukotriene Modifiers
Leukotriene modifiers act on cells that produce leukotrienes, which are lipid compounds released from mast cells, eosinophils, and basophils and that are responsible for airway bronchoconstriction, inflammatory cell recruitment, increased vascular permeability, and secretion production. Leukotriene modifiers work in two ways:
- By binding to cysteinyl leukotrienes receptors and blocking their activation and subsequent inflammatory cascade
- By stopping or inhibiting the production of the enzyme 5-lipoxygenase, a precursor to the production of leukotrienes
Leukotriene modifiers can help prevent symptoms for up to 24 hours, are well tolerated, and appear to work best in patients with mild to moderate persistent asthma. They are often used in addition to inhaled corticosteroids to avoid the use of oral corticosteroids and are an alternative, but not preferred, therapy to low- to medium-dose inhaled corticosteroids.
Guidelines suggest a trial of an antileukotriene in patients with severe asthma who are not controlled on high-dose inhaled corticosteroids and long-acting beta-2 agonists.
| Generic Name | Brand Name |
|---|---|
| Leukotriene receptor agonists | |
| Montelukast | Singulair |
| Zafirlukast | Accolate |
| 5-lipoxygenase inhibitor | |
| Zileuton |
Zyflo Zyflo CR |
Side effects of montelukast:
- Headache
- Earache
- Sore throat
- Abdominal pain
- Cough
- Dyspepsia
- Increased risk for respiratory infections
Precautions for montelukast:
On rare occasions montelukast has been linked to psychological reactions such as:
- Insomnia
- Anxiety
- Nightmares
- Aggression
- Hallucinations
- Depression
- Suicidal thinking
Contraindications for montelukast:
- Persons with phenylketonuria (PKU) should not take the chewable tablets that contain aspartame (an artificial sweetener that contains phenylalanine).
Side effects for zafirlukast:
- Headache
- Upper respiratory infections
- Nausea
- Vomiting
- Dyspepsia
- Abdominal pain
- Diarrhea
- Malaise
- Rarely, elevation of liver enzymes, acute hepatitis, and hyperbilirubinemia
Contraindications for zafirlukast:
- Not for use in patients with hepatic impairment
Immunomodulators
Immunomodulators are asthma therapy medications used to help regulate or normalize the immune system.
MONOCLONAL ANTIBODY THERAPY
Monoclonal antibody (biologic) therapy uses laboratory-produced substitute antibodies to bind to certain cells or proteins. They are add-on maintenance treatments for patients with exacerbations and/or poor control of symptoms despite taking high-dose ICS-LABA and for those with allergic or eosinophilic biomarkers or need maintenance oral corticosteroids (GINA, 2024). They include anti-IgE, anti-IL5/5Ra, anti-Il4Ra, and anti-TSLP.
Omalizumab is a newer asthma medication that may be used for persons with persistent moderate to severe asthma due to seasonal allergies that is not controlled by inhaled corticosteroids. A disadvantage is that it is very expensive ($12,000 to $15,000 per year). Omalizumab works by binding to human immunoglobulin E (IgE) on the surface of mast cells and basophils, resulting in reduced release of allergy-inciting chemicals.
Mepolizumab is also used for moderate to severe asthma. This agent works by binding to interleukin 5, resulting in decreased eosinophils that contribute to the development of asthma attacks.
Anyone age 6 and older can be given an omalizumab injection every 2 to 4 weeks. For individuals with elevated eosinophils, mepolizumab is given by injection every 4 weeks.
Dupilumab is used for the treatment of moderate to severe eosinophilic asthma in people age 6 and older. It reduces asthma exacerbations, enables oral corticosteroid tapering, and improves lung function (GINA, 2024).
| Generic Name | Brand Name |
|---|---|
| Omalizumab (anti-IgE) injection | Xolair |
| Mepolizumab (anti-IL5) injection | Nucala |
| Benralizumab (anti-IL5) injection (for ages 12 and older) |
Fasenra |
| Reslizumab (anti-IL5) injection (for ages 18 and older) |
Cinqair |
| Dupilumab | Dupixent |
Side effects:
- Pain or swelling in the area of injection
- Oropharyngeal pain
- Eosinophilia
Precautions:
- Omalizumab has the rare potential to induce anaphylaxis, so it must be administered only in a closely observed clinic.
- The FDA has issued a warning about a slight increased risk for heart and brain blood vessel problems with omalizumab, such as ministrokes, heart attacks, hypertension in the pulmonary arteries, and blood clots.
- Avoid use of live vaccines in patients being treated with dupilumab.
MAST CELL STABILIZERS
A mast cell stabilizer is an inhaled medication that prevents the release of histamine and other inflammatory substances from mast cells in response to an allergen that causes asthma. A mast cell stabilizer is not as potent as ICSs.
The only available mast cell stabilizer available for use in asthma is cromolyn sodium solution delivered via nebulizer. It may be used alone or with other asthma medications, such as bronchodilators or corticosteroids.
Symptoms may improve soon after starting cromolyn, but it could take up to 4 weeks before the full benefit of the medication is realized. Frequent dosing is necessary, as its effects last only 6–8 hours.
Common side effects:
- Coughing
- Nausea
- Throat dryness or irritation
Rare side effects:
- Dysphagia
- Pruritus
- Increased wheezing
- Dyspnea
- Hypotension
- Swelling of face, lips, or eyelids
- Chest tightness
Contraindications:
- Do not use in children younger than 2 years of age.
Precautions:
- Use with caution in those with heart disease or cardiac arrhythmias.
Pharmacology Step Therapy
GINA guidelines (2024) divide treatment into two tracks. Track 1 is the preferred treatment track, while track 2 offers an alternative if following track 1 is not possible. Each track consists of a series of steps that are based on the treatment needed to control symptoms.
The “step” and “track” treatment of asthma is based on severity of symptoms and the patient’s age, with medications added or deleted according to the frequency and severity of the patient’s symptoms. GINA guidelines describe two treatment tracks for adults and adolescents with asthma, mostly based on the choice of reliever therapy.
TREATMENT TRACKS
GINA (2024) guidelines recommend that adults and adolescents age 12 and older use low-dose inhaled corticosteroids (ICS) with formoterol to relieve symptoms or receive low-dose ICS whenever a SABA is needed. Inhaled corticosteroid medication is recommended even when an individual has infrequent symptoms, to lower the risk of serious exacerbations. GINA also recommends a reliever inhaler (ICS-formoterol, ICS-SABA, or SABA) for all individuals with asthma, although low-dose ICS-formoterol is preferred since it decreases the risk of severe exacerbations over a SABA reliever.
In track 1, which is preferred, reliever therapy is low-dose ICS-formoterol. When symptoms occur, low-dose ICS-formoterol is used as needed for symptom relief. In steps 3–5, the individual also receives ICS-formoterol as a daily treatment. This is the preferred treatment over using a SABA reliever since it decreases the risk for severe exacerbations. In track 1, only one medication is needed in steps 1–4.
Track 2 is an alternative therapy plan if track 1 cannot be used or if an individual is stable, had good adherence to therapy, and no episodes of exacerbations on current therapy. In track 2, reliever therapy is ICS-SABA or a SABA.
| Step | Track 1 (preferred controller and reliever) |
Track 2 (alternative controller and reliever) |
Reliever |
|---|---|---|---|
| 1 | Low-dose ICS-formoterol as needed | ICS whenever SABA is taken | Low-dose ICS-formoterol |
| 2 | Low-dose ICS-formoterol as needed | Low-dose maintenance ICS | As-needed low-dose ICS-formoterol |
| 3 | Low-dose maintenance ICS-formoterol | Low-dose maintenance ICS-LABA | As-needed low-dose ICS-formoterol |
| 4 | Medium-dose maintenance ICS-formoterol | Medium/high-dose maintenance ICS-LABA | As-needed low-dose ICS-formoterol |
| 5 |
|
|
As-needed low-dose ICS-formoterol |
| Step | Track 1 (preferred controller to prevent exacerbations and control symptoms) | Track 2 (other controller options; limited indications or less evidence for efficacy or safety) | Reliever |
|---|---|---|---|
| 1 | Low-dose ICS taken whenever SABA taken | Low-dose ICS taken whenever SABA taken | As-needed SABA (or ICS-formoterol reliever in maintenance and reliever therapy in steps 3 and 4) |
| 2 | Daily low-dose ICS | Daily leukotriene antagonist (LTRA) or low-dose ICS taken whenever SABA taken | As-needed SABA (or ICS-formoterol reliever in maintenance and reliever therapy in steps 3 and 4) |
| 3 | Low-dose ICS-LABA, OR medium-dose ICS, OR very low-dose ICS-formoterol maintenance and reliever therapy | Low-dose ICS + LTRA | As-needed SABA (or ICS-formoterol reliever in maintenance and reliever therapy in steps 3 and 4) |
| 4 | Refer for expert advice, OR medium-dose ICS-LABA, OR low-dose ICS-formoterol maintenance and reliever therapy | Add tiotropium or add LTRA | As-needed SABA (or ICS-formoterol reliever in maintenance and reliever therapy in steps 3 and 4) |
| 5 | Refer for phenotype assessment ± higher dose ICS-LABA or add-on therapy (e.g., anti-IgE, anti-IL4Ra, anti-IL5) | As last resort, consider add-on low-dose oral corticosteroid, but consider side effects | As-needed SABA (or ICS-formoterol reliever in maintenance and reliever therapy in steps 3 and 4) |
| Step | Preferred Controller Choice | Other Controller Options (limited indications or less evidence for efficacy or safety) | Reliever | Consider This Step for Children with: |
|---|---|---|---|---|
| 1 | Insufficient evidence for daily controller | Consider intermittent short course ICS at onset of viral illness | As-needed SABA | Infrequent viral wheezing and no or few interval symptoms |
| 2 | Daily low-dose ICS | Daily leukotriene receptor antagonist (LTRA) or intermittent short course ICS at onset of respiratory illness | As-needed SABA |
|
| 3 | Double low-dose ICS | Continue controller & refer to specialist assessment | As-needed SABA |
|
| 4 | Continue controller & refer to specialist assessment | Add LTRA, or increase ICS frequency, or add intermittent ICS | As-needed SABA |
|
For patients whose asthma has been well controlled for 2 to 3 months on a stable regimen, controller medications can be reduced in a stepwise fashion to a patient’s minimum effective treatment level. The purpose for stepping down therapy is to reduce long-term exposure to high doses of inhaled glucocorticoids (GINA, 2024).
WHEN TO REFER
Referral to a pulmonologist or allergist/immunologist is recommended in the following circumstances:
- Difficulty confirming a diagnosis of asthma
- A patient has experienced a life-threatening asthma attack
- The patient has required hospitalization or more than two bursts of oral glucocorticoids in a year or inability to discontinue oral glucocorticoids
- Need for step 5 care or higher in adult or step 4 or higher in children; need for step 4 care in an adult; need for step 3 care in a child over 5 years of age; need for step 2 care or higher in a child less than 5 years of age
- Poor asthma control after several months of active therapy and monitoring
- Anaphylaxis or confirmed food allergy
- Presence of complicating comorbidity
- Need for additional diagnostic tests
- Candidate for biologics or bronchial thermoplasty
- Candidate for allergen immunotherapy
- Patients with possible occupational triggers
- Patients with psychosocial or psychiatric problems which interfere with asthma
(Hartert & Bacharier, 2024)
Bronchial Thermoplasty
For patients with severe asthma that remains unimproved with the use of inhaled corticosteroids or long-term asthma medication, a minimally invasive nonpharmacologic procedure has been developed known as bronchial thermoplasty. Bronchial thermoplasty takes place over three bronchoscopy sessions and involves treating the inside of the airways in the lungs with a localized radiofrequency pulse.
This therapy was linked with an increase in the number of asthma exacerbations during the 3-month period of treatment in patients taking high-dose ICS-LABA medications. This was followed by a decrease in exacerbations but no favorable effects on symptoms or lung function compared to those in the sham treatment group. Follow-up suggests a prolonged decrease in exacerbations in some patients compared with before bronchial treatment. More research needs to be done to study effectiveness and safety of this treatment (GINA, 2024).
MANAGEMENT OF ASTHMA EXACERBATIONS (ATTACKS)
The most effective strategy for dealing with an asthma attack is early recognition and treatment. In ideal situations, patients assess the severity of an asthma attack at home by following an individualized asthma action plan (see “Developing an Asthma Action Plan” later in this course).
Some patients are more sensitive to an increase in asthma symptoms than others who may not recognize a problem until reduced airflow becomes more severe. This group may not know that asthma is worsening until a PEF measurement shows a decrease. It is helpful to identify these patients and provide education stressing that recognition of early signs of worsening asthma should be based on PEF monitoring.
Patients with a history of the following are at high risk for a fatal asthma attack:
- Previous severe exacerbation (e.g., intubation, intensive care unit admission)
- Asthma attack despite current course of oral glucocorticoids
- More than one hospitalization for asthma in the past year
- Three or more emergency department visits for asthma in the past year
- Food allergy in a patient with asthma
- Currently not using inhaled glucocorticoids
- Recent or current course of oral glucocorticoids
- Use of more than one canister of SABA per month
- Difficulty perceiving asthma symptoms or severe exacerbations
- Poor adherence with asthma medication and/or written asthma action plan
- Illicit drug use and major psychosocial problems including depression
- Comorbidities (e.g., cardiovascular or chronic lung disease)
(Cahill, 2024)
Basic Principles of Asthma Management
Basic principles to control hypoxia and to reverse airflow obstruction include:
- Assessing the severity of the attack and risk for asthma-related death
- Assessing potential triggers
- Using inhaled short-acting beta-2 agonists (such as albuterol, levalbuterol, albuterol-budesonide, or ICS-formoterol inhaler) early and frequently
- Starting systemic glucocorticoids if there is not an immediate and marked response to the inhaled SABA
- Advising patients who are not responding to go to an acute care facility or their asthma provider immediately, especially if they have a history of near-fatal asthmatic attacks
(Cahill, 2024)
Initial Home Management
The goals for home management are to relieve symptoms and prevent worsening of the attack to a severe and possibly life-threatening event. Patients should follow the instructions in their asthma action plan, which may include:
- Increasing the usual reliever medication, such as low-dose ICS-formoterol, a SABA, or ICS-SABA. In ICS-formoterol, both medications result in a reduction of severe exacerbations requiring oral corticosteroids, an emergency department visit, or hospitalization compared to using a SABA reliever.
- Continuing use of controller medication.
- Adding an oral corticosteroid according to the action plan and contacting the clinician to report symptoms and response to treatment and for guidance with care. The single most effective strategy for reducing emergency department visits and hospitalization for acute asthma is the timely administration of oral glucocorticoids.
- After the first hour, if there is improvement with increasing reliever medication, based on action plan or clinician guidance, a determination about seeking additional medical attention should be made.
- If there is a good response to home treatment and repeat PEF increases to >80% of the patient’s baseline over the course of about 1 hour, then the patient can safely continue home treatment.
- If initial home treatment is unsuccessful and there are signs or symptoms of severe asthma, or if the peak flow is <50% of the patient’s baseline, urgent medical attention should be sought.
The patient should not drive themself to the urgent care setting, and inhaled reliever medication should continue to be used while waiting for help to arrive (Cahill, 2024; GINA, 2024).
ASTHMA HOME MANAGEMENT FOR CHILDREN 5 YEARS AND YOUNGER
Parents or caregivers should follow the asthma action plan developed by their clinician. GINA (2024) recommends that treatment for an exacerbation at home begin with an inhaled SABA and assessing the condition in 1 hour or sooner. Urgent medical care is needed if the child is in acute distress, is lethargic, or does not respond to initial bronchodilator treatment, or the condition worsens, particularly in children less than 1 year of age. The parents or caregivers should seek medical attention the same day if the child needs inhaled SABA more often than 3-hourly or for more than 24 hours.
RESPONDING TO AN ATTACK WHEN NO INHALER IS AVAILABLE
An individual experiencing an asthma attack but who does not have a reliever inhaler at hand can be instructed to follow these steps:
- Get away from the asthma trigger as soon as possible and go to an air-conditioned environment or other place with clean air.
- Sit upright; stooping over or lying down constricts breathing.
- Take long, deep breaths to help slow down breathing and prevent hyperventilation, breathing in through the nose and then out through the mouth.
- Stay calm to prevent further tightening of chest muscles and make breathing easier.
- Drink a cup or two of a hot, caffeinated beverage (coffee or black tea), which can help open the airways slightly and help loosen mucus, providing some relief for an hour or two. (Caffeine is mobilized into theophylline, which is a drug used to prevent and treat asthma by relaxing airways and decreasing the lungs’ response to irritants.)
- Seek emergency medical help if wheezing, coughing, and breathing difficulty do not subside after a period of rest.
(SingHealth, 2024; Seladi-Schulman, 2023)
CASE
RESPONDING TO AN ASTHMA ATTACK
Gabriela, an RN, volunteers at her town’s outdoor summer-in-the-park concert series. While she is staffing the first aid tent, a frantic mother and teenager rush in. The mother shouts, “Mattie needs hot coffee RIGHT NOW!” The teen is pale, bent forward clasping her chest, struggling for breath, and obviously anxious. The mother tells the volunteers that her daughter is having an asthma attack, doesn’t have her inhaler, and that her doctor said hot black coffee could be used while waiting for an ambulance. She tells them Mattie had been exposed to cigarette smoke from other concertgoers and that it’s one of her asthma triggers.
Gabriela remains with Mattie and her mother while another volunteer goes to a nearby concession stand for the coffee and a third calls 911. Mattie gasps to Gabriela that her chest feels tight and that she can’t breathe. Gabriela tells her to sit down and sit up straight. She talks calmly to Mattie while applying a pulse oximeter to her finger, instructing her to take slow, deep breaths, to breathe in through her nose, and to breathe out through her mouth while pursing her lips. Mattie’s oxygen saturation (SaO2) is 95% on room air, and Gabriela tells Mattie that her “oxygen number” is within a safe range, the coffee is coming, and the ambulance will arrive shortly. Gabriela continues to talk calmly to both Mattie and her mother and notes that, as they talk, Mattie appears less anxious and her SaO2 drifts between 94% and 96%.
The hot coffee arrives and Mattie drinks it slowly but steadily, grimacing because she “hates coffee.” The ambulance arrives, and the EMTs assess Mattie, whose SaO2 is now 96% on room air. Per protocol, they administer a bronchodilator by nebulizer and monitor her response. Mattie responds well to the nebulizer treatment and meets criteria for discharge to home with an SaO2 of 99%.
During the entire treatment, Mattie’s mom vacillates between holding her daughter’s hand and berating herself for forgetting to bring the inhaler. One of the other volunteers stays with her and encourages her to be a bit easier on herself and try to remain calm to help Mattie relax.
As Mattie’s primary volunteer care provider, Gabriela tells Mattie, who is 17 and a high school senior, that she is not blaming either her or her mom for forgetting the inhaler but encourages her to take responsibility for making certain she has her inhaler with her at all times. She also asks if Mattie has a written asthma action plan, to which she replies yes.
When Mattie and her mother leave, they assure themselves and the volunteers that this has been a scary but valuable lesson. At the end of the concert, they stop by the tent to report that Mattie is doing fine and has had no further problems.
Asthma EMS Management
EMS management begins with assessment, which may be complicated by a setting that includes noise, distractions from bystanders or family, and an anxious hypoxic patient who is unable to provide a complete history. It is important to determine treatment provided to the patient before EMS arrival. Intravenous access should be obtained as quickly as possible.
Following assessment, the primary goal in EMS treatment is reversal of bronchospasm with nebulized SABA connected to supplemental oxygen. Ipratropium bromide can be mixed with SABA in a nebulizer. If the acute asthma exacerbation is associated with anaphylaxis or angioedema, epinephrine IM may be given, but epinephrine is not routinely administered for asthma exacerbations due to other causes (Fishe et al., 2023; GINA, 2024).
CPAP (continuous positive airway pressure) and BiPAP (bilevel positive airway pressure) are prehospital treatment options for moderate to severe asthma attacks. CPAP increases the pressure that the patient exhales against, which pushes open lower airways and improves gas exchange. BiPAP delivers a higher pressure with inhalation and expiration. Nebulized bronchodilators should be administered through CPAP, which provides an airtight seal to help direct medication into the lower airways. Care must be taken to avoid applying too much pressure, as air sacs are hyperinflated, and it is possible to cause a pneumothorax.
Magnesium sulfate IV is not routinely used for asthma exacerbations but may be administered for its effect as a smooth muscle relaxant in those who do not respond to initial treatment (GINA, 2024). For patients who are anxious or combative during a severe asthma attack, ketamine IV or IM may be used for sedation, as it causes bronchodilation and does not carry a risk of respiratory depression (Fishe et al., 2023). Systemic methylprednisolone or dexamethasone may be given to reduce inflammation.
Asthma patients with impending respiratory arrest require assisted ventilation starting with a bag valve mask and may later require intubation (Fishe et al., 2023).
CAPNOGRAPHY
Waveform capnography is a valuable tool to differentiate an asthma attack from other causes of respiratory distress (Sullivan, 2024). Capnography is a noninvasive measurement during inspiration and expiration of the concentration of carbon dioxide in the respiratory gases. End tidal capnography (EtCO2) is the measurement of the amount of carbon dioxide at the end of an exhaled breath. The results are displayed on a screen in waveforms and provide an immediate picture of the patient’s condition.
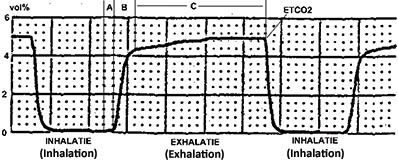
Capnography waveform measuring amount of exhaled carbon dioxide. (Source: Rschiedon at Dutch Wikipedia, CC SA 3.0.)
CASE
EMS RESPONSE TO AN ASTHMA ATTACK
The EMS crew is dispatched following a 911 call by a man’s wife, who reports that her husband is experiencing a severe asthma attack that has been brought on due to seasonal allergies. When they arrive, they find the man, Howard, wheezing and extremely dyspneic. The patient’s wife tells the team he has been using his rescue inhaler multiple times over the last few hours without relief.
The crew determines that Howard is nearing respiratory arrest as evidenced by his inability to speak two words in a row, severely reduced tidal volume, cool and clammy skin, and rapid heart rate and breathing. The paramedic, Jordan, administers 0.5 mg IM epinephrine 1:100 IM immediately, and the EMT, Sharon, places the patient on CPAP at 5 mmHg. Jordan starts an IV of normal saline.
After consulting with the local emergency department team, they administer 125 mg of methylprednisolone. Magnesium sulfate 2 gm IV is then started to run over 10 minutes. Capnography is used to monitor Howard’s response to treatment, which begins to show improvement, and he is then transported to the hospital emergency department.
Emergency Department Management
In an acute care setting, assessment of asthma exacerbation severity is based on symptoms, physical findings, peak expiratory flow, or less commonly, forced expiratory volume in 1 second (FEV1) measures, pulse oxygen saturation, and in certain circumstances, arterial blood gas measurement.
A focused history and physical are obtained while treatment is initiated, assessing for signs of severe exacerbation, which may include:
- Tachypnea
- Tachycardia
- Use of accessory muscles
- Diaphoresis
- Inability to speak in full sentences or phrases
- Inability to lie supine due to breathlessness
- Pulsus paradoxus
It is important to note that up to 50% of patients with severe airflow obstruction will not manifest any of these signs (Cahill, 2024).
Assessment is made for symptoms such as fever or purulent sputum in order to rule out alternative diagnoses. Chest X-ray is obtained when a complicating cardiopulmonary process is suspected, when a patient requires hospitalization, and when the diagnosis is uncertain.
Pulse oximetry is obtained for noninvasive screening for hypoxia, and a peak flow measurement is made in those without signs of impending respiratory failure.
In the ED, standard treatment is as follows:
- Supplemental oxygen is administered for all patients with hypoxemia, usually via nasal cannula but occasionally by face mask if needed.
- Inhaled SABA is considered standard initial care. Typically, three treatments are administered within the first hour. Delivery method varies with the setting and severity of the attack.
- Ipratropium, an inhaled anticholinergic agent (short-acting muscarinic antagonist, or SAMA) may be added, and ICS-formoterol may be used as an alternative to high-dose SABA therapy.
- Epinephrine administered IM is indicated for acute asthma associated with anaphylaxis or angioedema; it is not recommended for other asthma exacerbations.
- Systemic glucocorticoids speed resolution of an exacerbation and prevent relapse and are administered in all but the mildest cases.
- Intravenous administration of magnesium sulfate is not recommended for routine administration in asthma exacerbations but may reduce hospital admissions in some patients, such as adults with FEV1 <25%–30% predicted at presentation, those with persistent hypoxemia who fail to respond to initial treatment, and children with an FEV1 that fails to reach 60% predicted after 1 hour of treatment.
(GINA, 2024)
After the first hour of intensive treatment, a patient whose symptoms have resolved and whose PEF is 80% of predicted with good self-care skills and a supportive home environment may be discharged to continue treatment at home (GINA, 2024). Otherwise:
- Hospitalization is recommended in those with a FEV1 or PEF <25% predicted or personal best before treatment or posttreatment FEV1 or PEF is <40% predicted or personal best.
- If lung function after treatment is 40%–60% predicted, discharge may occur after taking risk factors and availability of follow-up care into the decision.
- If lung function after treatment is >60% predicted or personal best, discharge is recommended after taking risk factors and availability of follow-up care into the decision.
LIFE-THREATENING ASTHMA EXACERBATION
In patients presenting to the ED with impending or actual respiratory arrest, in addition to the treatments outlined above, options for ventilatory support must be assessed and implemented immediately as needed (Cahill, 2024). Signs of impending arrest that require rapid sequence intubation may include:
- Slowing of respiratory rate
- Depressed mental status
- Inability to maintain respiratory effort
- Inability to cooperate with administration of inhaled medications
- Worsening hypercapnia and associated respiratory acidosis
- Inability to maintain an oxygen saturation >92% despite face mask supplemental oxygen
Noninvasive ventilation (NIV) is increasingly used in patients with severe asthma exacerbations in an effort to avoid invasive mechanical ventilation. Noninvasive positive-pressure ventilation (NPPV) using a mask that conducts gas from a positive-pressure ventilator into the airways has become the predominant means of administering NIV. A short trial of NIV may be appropriate in cooperative patients not responding to medical therapy who do not require immediate intubation (Cahill, 2024).
WHEN TO HOSPITALIZE
The decision to admit to the hospital is based on findings from repeat assessment of a patient after receiving three doses of an inhaled bronchodilator, including the following criteria:
- Duration and severity of asthma symptoms
- Severity of airflow obstruction
- Course and severity of prior exacerbations
- Medication use and access to medications
- Adequacy of support and home conditions
- Presence of psychiatric illness
Patients who should be admitted to ICU for close observation and monitoring may exhibit the following:
- Rapidly worsening asthma or a lack of response to the initial therapy in the ED
- Confusion, drowsiness, signs of impending respiratory arrest, or loss of consciousness
- Impending respiratory arrest, as indicated by hypoxemia despite supplemental oxygen and/or hypercarbia
Intubation is required because of the continued deterioration of the patient’s condition despite aggressive treatments.
Status asthmaticus, an acute severe asthmatic episode that is resistant to appropriate outpatient therapy, is a medical emergency requiring aggressive hospital management. This may include admission to the ICU for treatment of hypoxia and dehydration, and possibly for assisted ventilation due to respiratory failure.
DISCHARGE FROM THE ED
Most patients with improving symptoms and a PEF >60% of predicted can be safely discharged if they are knowledgeable about their asthma and have the availability of follow-up care. Even with a rapid improvement, patients should be watched for 30–60 minutes to be certain they are stable before being released. Upon discharge, the patient should have an appointment for follow-up care.
All patients who have had an asthma attack severe enough to require emergency management should be given an ICS to reduce the risk of further exacerbations. The preferred treatment for adults and adolescents is ICS-formoterol (GINA, 2024).
Patient education includes a brief, focused session providing information about asthma, how to avoid asthma triggers, and how to provide initial home management in the event of further exacerbations. Assessment and retraining of inhaler use technique should be included. If the patient does not already have one, a personalized asthma action plan is provided.
Follow-up care with a primary provider or asthma specialist is recommended and facilitated whenever possible.
CASE
EMERGENCY DEPARTMENT RESPONSE
Manuel, a 20-year-old college student, arrives with his girlfriend, Jimena, to the emergency department reporting that he cannot breathe. Jimena tells the triage nurse that Manuel has a history of asthma and that he has been using his reliever and controller medications only sporadically because he has no health insurance and cannot afford to refill his medication. This week she says he has been using his reliever inhaler every day and that today he did not have a response. She says she believes the canister is empty.
The triage nurse, Jake, immediately places Manuel in a room and places him in high Fowler’s position. He begins his assessment of Manuel and notes that the patient’s breathing is labored, he has audible wheezing, and he can speak only in two- or three-word sentences.
A focused examination shows a pulse of 122 bpm and respiratory rate of 34 breaths per minute. Continuous pulse oximetry is begun, with initial O2 saturation of 89%. Jake applies supplemental oxygen per nasal cannula at 2 L/min and places Manuel on a cardiac monitor, which indicates sinus tachycardia.
The ED physician examines Manuel and finds he has diminished breath sounds and expiratory wheezing in all lung fields. Oxygen is increased to 3 L/min to reach an O2 saturation of 92%.
A nebulized SABA bronchodilator is begun. An IV is started, and Jake administers IV glucocorticoid. He obtains an arterial blood gas sample, which indicates hypoxia and hypercapnia.
The albuterol nebulizer treatment is repeated for a total of three treatments over the next hour. Monitoring of response to the nebulized treatment after the second treatment shows an increase in wheezing, which is a sign of improvement, as the bronchodilator begins to open the airways.
After Manuel’s third treatment, his pulse is 100 bpm, respiratory rate 22 bpm, and O2 saturation 97%. Auscultation reveals improved air flow through all lung fields and only a few expiratory wheezes.
Manuel is now able to answer questions without difficulty and remains under observation in the emergency department for an hour to ensure resolution.
Prior to discharge, Manuel is given an intramuscular injection of a long-acting glucocorticoid since he has not been medication adherent in the past. He is supplied with a combination controller/reliever inhaler with instructions in its use.
An individualized asthma action plan is prepared for Manuel in collaboration with Jake, the respiratory therapist, and the physician. He is given a list of available pharmaceutical assistance programs for free or low-cost asthma medications and instructed to have a follow-up with a primary care provider within 12–24 hours. Manuel is also given a list of clinicians and clinics in his area.
ASTHMA EXACERBATION MANAGEMENT IN CHILDREN
Most children with moderate or severe asthma exacerbations should be managed in an emergency department setting. Several clinical asthma severity scores for pediatric patients have been developed for use in evaluation of initial exacerbation severity, response to treatment, and determination of the need for hospitalization. These include:
- PRAM (Pediatric Respiratory Assessment Measure) uses five variables: wheezing, air entry, contraction of scalene muscles, suprasternal retraction, and oxygen saturation.
- PIS (Pulmonary Index Score) is based on five clinical variables: respiratory rate, degree of wheezing, inspiratory-to-expiratory ratio, accessory muscle use, and oxygen saturation.
- PASS (Pediatric Asthma Severity Score) is for patients ages 1–18 and includes three clinical findings: wheezing, prolonged expiration, and work of breathing.
- RAD (Respiratory rate, Accessory muscle use, and Decreased breath sounds) is used for children aged 5–17 years.
Oral systemic glucocorticoids are started as soon as possible after arrival in the ED, followed by administration of SABA via small-volume nebulizer or metered-dose inhaler with spacer. If repeated doses are needed, they are given every 20 to 30 minutes for three doses.
For moderate exacerbation, nebulized SABA combined with ipratropium bromide is administered every 20 to 30 minutes for three doses or continuously for 1 hour. Oxygen is be administered to maintain saturation between 94% and 98%.
For severe exacerbations, most children need ongoing administration of continuous rather than intermittent nebulized SABA, unless they have a dramatic improvement after the first hour.
Intravenous methylprednisolone can be started as soon as intravenous access is obtained. Intravenous magnesium may also be administered if needed.
Consultation with a pediatric intensive care unit and/or anesthesia is indicated when a child has signs of impending respiratory failure, including:
- Cyanosis
- Inability to maintain respiratory effort
- Depressed mental status
- Pulse oxygen saturation <90% and/or respiratory acidosis noted on venous, arterial, or capillary blood gas sample
IV terbutaline in addition to inhaled SABAs and noninvasive positive pressure ventilation or endotracheal intubation may be indicated. Clinicians must be prepared to manage acute deterioration after intubation. The clinician most experienced in airway management should perform the procedure.
Children who have marked improvement in clinical parameters within the first 1–2 hours of therapy may be discharged home. Marked improvement is manifested by diminished or absent wheezing and retracting and increased aeration that is sustained at least 60 minutes after the most recent SABA dose.
Children who were moderately to severely ill on arrival and who have little improvement or worsen after initial therapy with SABAs and systemic glucocorticoids require hospitalization, including those who continue to have significant wheezing, retractions, and poor aeration. Additional factors include:
- Beta-2 agonist therapy more often than 4 hours
- Requirement for supplemental oxygen/low oxygen saturation on pulse oximetry an hour or more after starting therapy
- Inability to self-hydrate
- History of rapid progression of severity
- Poor adherence to outpatient medication regimen
- Recent treatment with systemic glucocorticoids or beta agonist overuse
- Inadequate access to medical care, including lack of transportation back to hospital if deterioration occurs
- Poor social support system at home, with inability of caregivers to provide medical care and supervision
(Scarfone, 2024; Sawicki & Haver, 2024b)
ASTHMA EXACERBATION MANAGEMENT IN PREGNANT WOMEN
Mild and well-controlled moderate asthma can be associated with excellent maternal and perinatal pregnancy outcomes. Severe and/or poorly controlled asthma has been associated with numerous adverse perinatal outcomes as well as maternal morbidity and mortality.
Pregnant patients who present with typical mild exacerbation are placed on a cardiac monitor and pulse oximetry. Fetal heart rate monitoring is the best available method for determining whether the fetus is adequately oxygenated.
The recommended pharmacotherapy for acute asthma during pregnancy is substantially identical to the management in nonpregnant patients. When considering asthma medication use in a pregnant woman or a woman anticipating pregnancy, concerns about potential risks of asthma medication are generally outweighed by the potential adverse effects of untreated asthma. Careful follow-up by clinicians experienced in managing asthma is essential.
Inhaled corticosteroids are the preferred medication for all levels of persistent asthma during pregnancy, with the goal of maintaining adequate oxygenation of the fetus by prevention of hypoxic episodes in the mother (Morris, 2024a; Schatz & Weinberger, 2024).
ASTHMA INPATIENT MANAGEMENT
When patients are admitted to the hospital following an acute asthma exacerbation, a multidisciplinary team will manage their care, including medicine, nursing, and respiratory therapy.
The purpose for hospitalization is to closely monitor the patient and to have aggressive interventions available in the event the asthma worsens. Hospitalization also serves the purposes of removing the patient from the stimuli in the home environment that may have aggravated asthma, ensuring medication compliance, and permitting inactivity during recovery. In many instances, airway obstruction remains unstable, with wide swings in expiratory flow over minutes or hours.
Patients usually will have received bronchodilator treatments, systemic corticosteroids, other medications, and oxygen in the emergency department. Inpatient treatment is often a continuation of those therapies and monitoring progress.
Inpatient Medical Management
Medication and treatment modalities will be ordered by the admitting provider, who determines initial pharmacologic treatment depending on the severity of the patient’s exacerbation. During the patient’s inpatient stay, medical management is as follows:
MONITORING
- Obtaining ABGs on admission
- Monitoring and responding to changes in vital signs:
- Done on admission and every 4 hours for 12 hours
- After 12 hours, every 6 hours
- Monitoring PEF rate:
- If the patient is on hourly nebulizer treatments, peak flow every hour
- At least twice daily
- Monitoring oxygen saturation with spirometry:
- Provide supplemental oxygen to keep O2 saturation adequate (>93% for adults, >95% for children)
- Discontinue when O2 saturation is adequate for 4 hours and patient is on general ward
- Continue spot checks of O2 saturation with vital signs or as needed for respiratory distress
- Telemetry monitoring indications:
- Patient is receiving SABA nebulizer treatments more often than every 4 hours
For infants or young children, corroborate O2 saturation monitor with pulse rate as a child’s movements make oxygen saturation inaccurate. A decrease in oxygen saturation increases pulse rate.
MEDICATIONS
- SABA by nebulizer
- IV methylprednisolone (Solu-Medrol)
- Change to oral prednisone when SABA is spaced at 4 hours or more and patient is tolerating oral intake
EVALUATION
- Arterial blood gases
- Pulmonary function tests. Criteria:
- PEF <30%
- Prior history of pCO2 >40
- Failure to improve in 4 hours of therapy
- Clinical asthma score >7
- Indications to monitor serum electrolytes:
- Nausea or vomiting
- IV fluids administered for >24 hours
- Beta agonist use more often than every 4 hours for 24 hours
- Chest X-ray indications:
- First episode wheezing
- Marked breath sound asymmetry
- History of exam suggestive of pneumonia
- Signs of improvement:
- Minimal or no wheezing
- Fewer than two awakenings at night due to mild asthma symptoms
- Good activity tolerance
- Pulmonary function test: PEF or FEV1 >60% of baseline
- Adequate O2 saturation off supplemental oxygen
MORE INTENSIVE TREATMENT OPTION
- Admit to intensive care unit if no improvement in 6–12 hours
PREPARATION FOR DISCHARGE
- Assess for asthma-related death risk factors:
- Requires inhaled SABA no more frequently than once every 4 hours
- Parenteral steroids switched to oral corticosteroids
- Adequate O2 saturation on room air
- Asthma education, including:
- Instructions and return demonstration for use of inhaled controller medications
- Instruction in obtaining peak flow measurements at home
- Completing a personalized asthma action plan
- Appointment made for follow-up in 7–10 days after discharge
Inpatient Nursing Management
Upon arrival to a nursing unit, the admitting nurse performs a complete nursing assessment and develops a plan of care that addresses issues according to the patient’s individual needs. In the creation of a care plan, specific problems are identified, related factors are acknowledged, defining characteristics are considered, and a nursing diagnosis is made. Common problems for a patient with asthma may include, but are not limited to:
- Inability to clear airways effectively
- Altered breathing patterns
- Altered exchange of gases in the lungs
- Anxiety
For each nursing diagnosis, short- and long-range measurable and achievable goals are set, followed by nursing interventions that will assist the patient to meet those goals. The plan is implemented, and each intervention and outcome are assessed for effectiveness.
INABILITY TO CLEAR AIRWAYS EFFECTIVELY
Ineffective airway clearance is related to bronchoconstriction, increased mucus production, decreased ciliary action, ineffective cough, and decreased energy or fatigue as evidenced by:
- Abnormal breath sounds
- Abnormal respiratory rate, rhythm, and depth
- Excessive secretions
- Dyspnea
- Hypoxemia/cyanosis
- Inability to cough up secretions
- Ineffective or absent cough
- Orthopnea
Goals/Outcomes
- Patient will maintain clear and open airways as evidenced by:
- Normal breath sounds
- Normal rate/depth of respirations
- Effective cough after treatment and deep breathing
- Increased air exchange
- Patient will explain methods to enhance secretion removal
- Patient will recognize the significant of changes in sputum, including:
- Color
- Character
- Amount
- Odor
- Patient will identify and avoid specific factors that inhibit effective airway clearance
Nursing Assessment
- Airway patency and abnormal breath sounds:
- Decreased or absent breath sounds
- Wheezing (high-pitched whistling)
- Expiratory grunt
- Rales (clicking, rattling, coarse crackles)
- Rhonchi (low-pitched rattle)
- Stridor (high-pitched musical sound)
- Respirations:
- Rate and depth
- Pattern
- Flaring of nostrils
- Dyspnea on exertion
- Evidence of splinting
- Use of accessory muscles
- Position taken for breathing
- Changes in mental status:
- Increased lethargy
- Confusion
- Restlessness
- Irritability
- Vital signs (elevated temperature may indicate infection)
- Effectiveness of cough and productivity
- Sputum
- Quality, amount, color, and consistency
- Signs of infection (odor and discoloration)
- Signs of dehydration (thick, tenacious)
- Submit a sputum specimen for culture and sensitivity testing, as appropriate
- Oxygen saturation, using pulse oximetry
- Arterial blood gases
- Hydration status:
- Skin turgor
- Mucous membranes
- Tongue
- Abdominal or thoracic pain (as possible cause for shallow breathing and ineffective cough)
- Peak airway pressures and airway resistance, if on mechanical ventilation
- Patient’s understanding of the disease process (depending on patient’s acute state as well as cognitive level)
- Patient’s use of herbal treatments that may result in drug interactions with prescribed medications (e.g., echinacea, goldenseal, ma huang)
Nursing Interventions
- Teach and assist with effective ways to remove secretions, i.e., taking a deep breath, holding it for 2 seconds, and then coughing two or three times in succession.
- Position patient in high Fowler’s, if tolerated, to improve lung exchange and air exchange.
- Provide education that includes:
- Proper sitting position to promote use of abdominal muscles for more forceful cough
- Use of pillow or hands to splint the abdomen when coughing
- Use of quad and huff techniques:
- Hold breath for two or three seconds.
- Exhale forcefully but slowly to move mucus from smaller to larger airways.
- Repeat two more times.
- End with one strong cough to clear mucus from larger airways.
- Use of incentive spirometry
- Importance of ambulation and frequent position changes
- Proper use of prescribed medications and inhalers
- Need for adequate fluid intake even after discharge
- Perform nasotracheal suctioning PRN, especially if cough is ineffective.
- Maintain humidified oxygen to reduce thickness of secretion.
- Encourage fluid intake to 3 L/day within limits of cardiac reserve and renal function.
- Give medications as prescribed and document effectiveness and side effects.
- Coordinate with respiratory or physical therapy for chest physiotherapy and nebulizer management.
- Provide postural drainage, percussion, and vibration as prescribed.
- Provide oral care every 4 hours.
(Wayne, 2024)
ALTERED BREATHING PATTERN
Breathing pattern alterations can result in inhalations and exhalations that do not allow for adequate ventilation. Patients with asthma are prone to dysfunctional breathing patterns most often related to hypoxia, the underlying inflammatory process, tracheobronchial constriction, decreased energy, fatigue, or anxiety, as evidenced by:
- Cough
- Cyanosis
- Dyspnea
- Nasal flaring
- Prolonged expiration
- Changes in respiratory depth
- Tachypnea
- Accessory muscle use
Goals/Outcomes
- Reach and maintain optimal breathing pattern as evidenced by:
- Relaxed and normal breathing pattern
- Normal breathing rate
- Absence of dyspnea
Nursing Assessment
- Vital signs for evidence of hypoxia and hypercapnia:
- Changes in blood pressure
- Changes in heart rate
- Respiratory rate, depth, and rhythm for signs of impending respiratory failure:
- Inability to breathe, cyanosis related to hypoxemia
- Increased respiratory rate, confusion related to hypercapnia
- Breath sounds for signs of respiratory failure:
- Decreased wheezing
- Indistinct breath sounds
- Relationship of inspiration to expiration
- Signs of dyspnea:
- Flared nostrils
- Chest retractions
- Accessory muscle use
- Conversational dyspnea (inability to converse without difficulty)
- Fatigue (may lead to respiratory failure)
- Presence of pulsus paradoxus greater than 12 mmHg during inspiration (decrease in systolic blood pressure and pulse amplitude during inspiration)
Nursing Interventions
- Plan for periods of rest between activities to reduce metabolic rate and oxygen requirements.
- Maintain elevated head of bed to 45 degrees.
- Demonstrate and encourage diaphragmatic and pursed-lip breathing.
- Administer medications as ordered.
- Monitor oxygen saturation levels (normal is 95%–100%).
- Monitor PEF and FEV1 as taken by respiratory therapy.
(Martin P, 2024)
ALTERED EXCHANGE OF GASES IN THE LUNGS
Alterations in the exchange of gases in the lungs results in an excess or deficiency in oxygenation and/or carbon dioxide related to altered oxygen supply due to bronchospasm, mucosal edema, and mucus plug formation, as evidenced by the same manifestations as patients with both impaired airway clearance and impaired breathing pattern but also:
- Changes in vital signs
- Oxygen saturation <90%
- Anxious appearance
- Diaphoresis
- Restlessness
- Irritability
- Confusion
- Altered skin color: pallor, cyanosis, duskiness
- Abnormal lung sounds, rate, rhythm, and depth
- Tripod position
- Dyspnea
Goals/Outcomes
- Absence of respiratory distress signs and symptoms
- Vital signs within patient’s normal limits
- Clear breath sounds
- Oxygen saturation persisting at >90%
- Normal mentation
Nursing Assessment
- Characteristics of respirations (rate, rhythm, depth, use of accessory muscles)
- Oxygen saturation, monitoring continuously
- ABGs, monitoring frequently
- Lung sounds, auscultating at least every 2–4 hours, listening for adventitious breath sounds
- Ability to cough and clear secretions, noting characteristics of sputum: amount, color and consistency
- Skin and mucous membranes, monitoring for peripheral cyanosis (nailbeds) or central cyanosis (lips/earlobes, tongue) (duskiness and central cyanosis indicate advanced hypoxemia)
- Mentation, for irritability, restlessness, and confusion, and lethargy and somnolence as late signs of hypoxia
- Patient’s level of stress and anxiety
- Nutritional status
- Hemoglobin level
Nursing Interventions
- Monitor oxygen saturation utilizing continuous pulse oximetry.
- Administer oxygen as ordered to maintain oxygen saturation above 90%.
- Administer medications as ordered and assess for effectiveness and side effects.
- Elevate the head of the bed (30 to 45 degrees) to minimize difficulty breathing and promote maximum lung expansion, using high Fowler’s position or over-the-table positioning if necessary.
- Adjust position frequently to maintain correct body alignment for easier ventilation and gas exchange.
- Encourage prone position as tolerated to increase PaO2.
- Consider a RotoProne-type therapy system or mattress with a percussion function to help loosen and remove secretions.
- Encourage frequent pulmonary hygiene measures:
- Cough and deep breathing exercises
- Use of incentive spirometry
- As directed by respiratory therapy, use of a flutter valve to loosen secretions (a handheld device that causes airway vibration and positive expiratory pressure)
- Provide small, frequent meals and add supplements.
- Encourage ambulation as tolerated.
- Provide rest periods between activities of daily living (ADLs) and pace activities.
- Provide reassurance for the patient who is anxious.
For the critical care patient:
- Anticipate need for intubation.
- Suction airway as needed.
ANXIETY
Asthma causes stress, which in turn may cause anxiety. As symptoms worsen, the patient may become more anxious, which then increases asthma symptoms, resulting in a sensation of panic. Anxiety and stress are also known triggers for asthma exacerbations.
Common factors may include:
- Change in environment
- Change in health status
- Loss of control
- Hypoxia
- Respiratory distress
Common assessment cues include:
- Apprehensiveness
- Dyspnea
- Fear of being left alone in a room
- Restlessness
- Tachycardia
- Tachypnea
Goals/Outcomes
- Use an effective coping mechanism
- Verbalize a reduction in level of anxiety experienced
- Demonstrate reduced anxiety as evidenced by a calm demeanor and cooperative behavior
Nursing Assessment
- Signs of anxiety:
- Feelings of panic, fear, uneasiness
- Tachycardia
- Cold or sweaty hands or feet
- Shortness of breath
- Restlessness
- Oxygen saturation
Nursing Interventions
- Encourage verbalization of concerns.
- Provide comfort measures (e.g., a calm, quiet environment; soft music).
- Explain every procedure in a simple and concise manner.
- Update significant others of the patient’s progress, with patient’s permission (since family anxiety can be easily transferred to the patient).
- Stay with the patient and encourage slow, deep breathing.
- Assure the patient and significant others of close, consistent monitoring that will ensure prompt intervention.
- Encourage use of relaxation techniques:
- Progressive muscle relaxation
- Diaphragmatic and pursed-lip breathing
- Use of imagery, repetitive phrases
ASTHMA PATIENT TEACHING
Clinicians play an important role through teaching patients and families during the inpatient stay, providing education on the asthma disease process and symptom recognition, and discussing other topics. Subjects covered in patient teaching include:
- Cough and deep breathing methods
- Types of oxygen therapy to be used at home, if applicable
- Early signs of decreased oxygenation and interventions
- Education on smoking cessation and resources that can help
- Correct use of medications:
- Indications for use
- Dosage
- Frequency
- Differentiating between rescue and controller medications and effects
- Demonstration and verification of correct inhaler use
- Demonstration and verification of correct nebulizer use
- Development or updating of the asthma action plan
- Environmental control of triggers and aggravators
- Demonstration and verification of correct peak flow meter use
- Importance of posthospitalization follow-up with the primary care provider
- Energy conserving techniques
(RNlessons, n.d.)
Asthma Inpatient Respiratory Therapy
Respiratory therapists follow and assess patients throughout their hospital stay, adjusting their treatment and educating them according to guidelines. Respiratory therapists:
- Recommend, administer, and evaluate the pharmacology regimen for a patient
- Perform airway clearance:
- Pulmonary hygiene techniques
- Deep-breathing exercise
- Chest physiotherapy
- Recommend, administer, and evaluate oxygen therapy
- Perform rest and exercise oximetry
- Perform arterial blood gas sampling and interpretation
- Recommend, administer, and evaluate humidification/aerosol therapy
- Recommend, administer, and evaluate noninvasive positive-pressure ventilation therapy
- Recommend, administer, and evaluate airway management
- Recognize the causes of ventilator/respiratory failure and recommend, perform, and evaluate ventilator management
- Establish and maintain mechanical ventilation with a given ventilator
- Perform and interpret pulmonary function tests
(NSCC, 2023/2024)
CHEST PHYSIOTHERAPY
Chest physiotherapy (PT) is routinely carried out by both respiratory and physical therapists depending on a facility’s policies and staffing. Chest PT involves a group of treatments meant to eliminate secretions in the airway and works best if applied along with a bronchodilator. The purpose of these treatments is to:
- Facilitate removal of retained airway secretions
- Optimize lung compliance and prevent collapse
- Decrease the work of breathing
- Optimize the ventilation-perfusion ratio and improve gas exchange
Postural drainage involves placing the patient in a position in which gravity can assist in airway clearing. Positions vary based on specific segments of the lungs with large amounts of secretions. Each position should generally be held for 3–15 minutes.
Percussion, also called cupping, involves intermittently applying kinetic energy to the chest wall and lungs by rhythmically striking the chest with a cupped hand or mechanical device directly over the area of the lung being drained.
Vibration involves the use of a fine tremorous action over the area being drained. The rapid vibratory impulse is transmitted through the chest wall from the hands of the therapist to loosen and dislodge the airway secretions (Physiopedia, 2021).
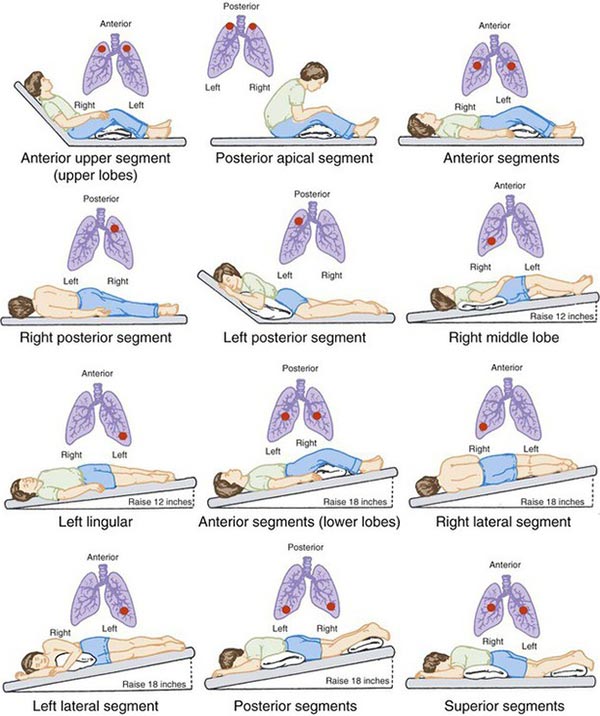
Postural drainage positions. (Source: Adapted from Potter & Perry, 1997.)
(See also “Physical Therapy” later in this course.)
LONG-TERM ASTHMA MANAGEMENT
Asthma is a chronic illness, and good asthma therapy is built on a long-term plan. The ultimate goal for a patient with asthma is the prevention of functional and psychological morbidity to provide as healthy a lifestyle as possible for the individual’s age. Because the goal of asthma treatment and control is for each patient to live a near-normal life, asthma control should minimize the symptoms that interfere with work, school, sleep, exercise, and leisure activities. Asthma exacerbations should be prevented or reduced, and ED visits should be rare.
Control of symptoms and risk reduction are the main features of long-term asthma management. Asthma control, adherence, and inhaler technique are assessed at every visit, not just when the patient presents because of their asthma.
Control of Symptoms
Symptom control relies on medication that is adjusted in a continuous cycle of assessment, fine-tuning, and review of response. Medications are prescribed at the minimum necessary to maintain control of symptoms.
ASTHMA MEDICATION MANAGEMENT
Medication management for a patient diagnosed with asthma is based on the patient’s severity of symptoms and follows step therapy guidelines (see “Pharmacology Step Therapy” above). Patients should be seen 1–3 months after starting treatment and every 3–12 months thereafter. After an exacerbation, a review visit within 1 week should be scheduled.
Pregnant women, however, should be reviewed every 4–6 weeks. Since asthma exacerbations can have negative consequences during pregnancy and infancy, stepping down treatment is not advised until after delivery (GINA, 2024).
ASSESSING ASTHMA CONTROL
Asthma control has two domains that require assessment: symptom control and future risk of adverse outcomes. Lung function is an important part of the assessment of future risk and is measured at the start of treatment, after 3–6 months of treatment (to identify the patient’s personal best), and periodically thereafter for ongoing risk assessment (GINA, 2024).
Achieving and maintaining asthma control are the goals of therapy. Accurate assessment is difficult due to the complex nature of asthma control and to the limitations of assessment methods. Lung function testing is insufficient because patients may have normal spirometry readings between exacerbations. Asthma control level is often overestimated by both clinicians and patients. Patients often underreport asthma symptoms, failing to recognize how asthma affects their daily activities.
There are several standardized tools developed to quantify the level of asthma control, including the following (GINA, 2024; University of Newcastle, 2022):
- Asthma Control Test (ACT) is a five-item questionnaire for patients ages 12 and older. It is a patient-centered/completed questionnaire that assesses only symptom control (night and day) over the prior 4 weeks, including:
- Activity limitation
- Shortness of breath
- Use of rescue medications
- Nighttime awakening
- Patient’s perception of asthma control
- Childhood Asthma Control Test (cACT) is used with children ages 4–11. Both child and caregiver perspectives are assessed for the previous 4 weeks. It is composed of seven questions, four child-reported and three caregiver-reported.
- Asthma Control Questionnaire (ACQ), a five-, six-, or seven-item questionnaire, including spirometry for ages 11 and older, involves asking patients to recall their symptom control over the previous week. It is the only tool that includes lung function testing.
- Asthma Therapy Assessment Questionnaire (ATAQ) is a brief, self-administered tool for use in adults 18 and older that assesses the level of asthma control during the prior 4 weeks. It includes questions about symptoms, missed work or school, effect on activities of daily living, and use of rescue inhalers. A parent-completed ATAQ version is available for children and adolescents ages 5–17 years.
- Global Initiative for Asthma (GINA) provides a four-item questionnaire for ages 6 and older about daytime and nighttime symptoms, reliever inhaler use, and activity limitation.
- Asthma Daytime Symptoms Diary (ADSD) and Asthma Nighttime Symptom Diary (ANSD) are six-item daily measures of asthma symptom severity that assess breathing symptoms, chest symptoms, and cough. Together, they are intended for twice-daily completion, once upon awakening referring to symptoms during the night and once in the evening referring to symptoms experienced during the day (U.S. FDA, n.d.).
ASSESSING QUALITY OF LIFE
Health-related quality of life is considered an important variable to be managed in patients with asthma. Besides physical symptoms, patients may experience fatigue, psychomotor sluggishness, irritability, and mood and cognitive disturbances. The combination of physical symptoms and emotional and functional problems may diminish a patient’s quality of life.
The Asthma Quality of Life Questionnaire (AQLQ) is one of several assessment tools used to measure functional problems (physical, social, occupational) that are most bothersome to adults ages 17–70 with asthma. There are also several questionnaires appropriate for pediatric patients with asthma. (See also “Resources” at the end of this course.)
ADDRESSING CHALLENGES
There are many challenges to successfully maintaining asthma control. Adherence to asthma medication regimens tends to be very poor, with reported rates of nonadherence ranging from 20% to 80%. Medication-related factors include difficulties with inhaler devices, complex regimens, side effects, dislike of medication, distant pharmacies, and especially the price of inhalers (Apter & Gleeson, 2024).
COST OF ASTHMA MEDICATIONS
Asthma disproportionately affects those with a lower socioeconomic status. In adults with asthma, a disruption in health insurance, no health insurance, or being on Medicaid or Medicare increases the risk of having an exacerbation. Some people without health insurance may delay or stop filling their prescriptions for asthma medications or adjust the dose on their own to make their medications last longer (Suri et al., 2022).
In a study of the impact of health insurance and the Affordable Care Act (ACA) on asthma outcomes in low-income adults, Suri and colleagues (2022) found that the ACA significantly decreased the number of uninsured individuals but there was no significant change in asthma outcomes. They noted that insured individuals still faced cost barriers for obtaining medications and visiting healthcare providers.
The cost of asthma inhalers in the United States is significantly higher than in other countries. In 2024, some of the major manufacturers of asthma inhalers revealed that they were placing a $35/month cap on out-of-pocket costs for those with commercial or private insurance as well as those without insurance (AAFA, 2024f).
Other challenges to asthma control that are not related to medications include:
- Misunderstanding or lack of instruction
- Fears about side effects
- Dissatisfaction with healthcare professionals
- Unexpressed/undiscussed fears or concerns
- Inappropriate expectations
- Poor supervision/training or follow-up
- Anger about one’s condition or its treatment
- Underestimation of severity
- Cultural issues
- Stigmatization
- Forgetfulness or complacency
- Attitudes toward ill health
- Religious issues
- Social barriers such as work schedules
- Stress, depression, and comorbidities
In addition to the above challenges, adolescents face developmental challenges that can affect adherence. At this age, individuals are searching for greater autonomy and have a need to be accepted by peers. Challenges may include:
- Denial of asthma diagnosis or severity
- Burdensome medication routine that conflicts with the need for greater autonomy
- Embarrassment around the use of inhalers in front of peers
- Greater risk of depression and anxiety among this age group
Developing an Asthma Action Plan
A successful asthma management plan requires the continued attention of a disease manager, and the patient or patient’s caregiver should take that role. With their primary care provider, patients design a plan that is realistic, and the patients and caregivers must then ensure that the plan is carried out. To these ends, it is important that providers and patients design an action plan together.
The more patients understand the reasons for their healthcare providers’ recommendations, the more likely it is that those recommendations will be carried out. Providers must shape their recommendations to be realistic for and understandable to each patient; they should also listen to be certain that they are addressing their patients’ goals (Apter & Patel, 2024).
ASTHMA PATIENT EDUCATION
The plan of action includes patient education. It is known that clinician care is necessary, but such care is not sufficient for a patient to achieve control of asthma. The patient also must be taught effective self-management strategies that support the goals of:
- Improved quality of life
- Improvement in symptoms
- Fewer activity limitations
- Improved medication adherence
- Fewer urgent care visits
- Fewer hospitalizations
- Reduced asthma-related expenditures
Patient education begins at the initial visit and is reinforced with every visit thereafter. Both patients and caregivers are involved in the educational process, which includes instruction and demonstration of understanding of:
- Pathophysiology of asthma and causes for airflow obstruction that leads to the symptoms of asthma
- Recognition of various symptoms of a potential asthma attack
- Medications used for treatment of asthma, including clear instructions and demonstration of the correct use of each type of inhaler and spacer or chamber device being considered for treatment
- Explanation for and demonstration of the use of a peak flow meter to help detect changes in airflow before symptoms are present and to obtain objective confirmation of changes in airflow when symptoms do develop
- Premedicating to prevent onset of symptoms and treatment of symptoms
(Apter & Patel, 2024)
CASE
PATIENT EDUCATION
JONAH, AGE 11 (continued from earlier in this course under “Comorbid Factors”)
Jonah, the 11-year-old identical twin who was brought to the pediatrician’s office by his mother, returned to the office to meet with the nurse after being diagnosed with asthma and given a prescription for a reliever inhaler. The following patient education was accomplished at this visit:
- The nurse gave Jonah the inhaler, described how to use it, and told him he is to use it when he experiences an asthma attack while at home or at school. The nurse then explained how the inhaler works, demonstrated the technique, and had Jonah return the demonstration using a dummy inhaler. She also gave him a pamphlet that pictorially describes the use of the inhaler and instructions on the prescribed dosage and frequency of inhaler use.
- The nurse gave Jonah tips to help him assess the severity of an attack, noting that when he starts to wheeze, cough, and have difficulty breathing or talking during normal activities, those symptoms signal a need for the use of the inhaler.
- The nurse reviewed the use of the peak flow meter with Jonah and his mother. Jonah practiced using it to arrive at his “personal best.” This and detailed instructions on how to assess Jonah’s values were discussed.
- The nurse helped prepare a written set of instructions for Jonah and a separate, more detailed set of instructions for his mother. The mother’s instructions focused more specifically on when to repeat bronchodilator treatment, call his primary care provider, or take Jonah to the emergency department based on his response to the reliever bronchodilator as determined by peak flow values and the severity and/or persistence of symptoms.
- The nurse gave Jonah and his mother a list of patient education websites and videos addressing asthma in children, including a link to an online video series on asthma education for children. (See “Resources” at the end of this course.)
- Because Jonah’s identical twin brother also has asthma, the nurse discussed with his mother some issues and challenges that might arise between the two brothers. This might include competing between themselves to see who waits the longest before using a rescue inhaler or other ways they may find in which to compare and contrast their illness.
- The nurse made a separate copy of the mother’s instructions for the school nurse, which Jonah’s mother indicated she would deliver herself.
ELEMENTS OF THE ASTHMA ACTION PLAN
The most effective way to ensure that patients understand how to manage their asthma is by developing an individualized action plan between the patient and their healthcare provider. An action plan is a written worksheet that indicates specific instructions for early treatment of asthma symptoms, what steps should be taken to prevent asthma from worsening, and guidance on when to call a healthcare provider or when to seek emergency treatment (ALA, 2024b).
The following is an example of an action plan that includes recommendations and directions for both adults and children.
SAMPLE ASTHMA ACTION PLAN
Person’s name: _________________________
Primary care provider: _________________________
Provider’s phone number: _________________________
Hospital or emergency department phone number: _________________________
Date: _________________________
Personal best peak flow: _________________________
|
||
| Medicine | How much to take | When to take it |
| Long-term control medicines. Take every day, even if not having any asthma symptoms. Avoid asthma triggers. | ||
| Before exercise: | ||
| Number of puffs: _____ | 5 minutes before exercise | |
|
||
| Medicine | How much to take and how often | Nebulizer |
| 1. Keep taking green zone medications and avoid triggers. | ||
| 2. Add reliever medicines. | ||
| Reliever:_______ | ____ puffs | OR Nebulizer: ______ (Use once.) |
| 3. If symptoms (and peak flow) do not return to Green Zone after 1 hour of treatment, take the following: | ||
| Reliever:_______ | ____ puffs | OR Nebulizer: ______ (Use once.) |
| Oral steroids:_______ | ____ mg/day for ___days | |
| 4. Call the doctor before taking oral steroid OR ______ minutes/hours after taking an oral steroid. | ||
|
||
| Medicine | How much to take and how often | Nebulizer |
| 1. Take these medications: | ||
| Reliever:_______ | ____ puffs Can repeat every __ minutes, up to __ times |
Nebulizer:________ Can repeat every __ minutes, up to __ times |
| Oral steroid:_______ | ____ mg | |
| 2. Call your primary care provider now. Go to your hospital or call an ambulance if you are still in the Red Zone after 15 minutes and you have not reached your provider.
If you have these DANGER SIGNS: trouble walking or talking due to shortness of breath or your lips or fingernails are blue, pale, or gray, then… Take __ puffs of your reliver medicine and go to the hospital or call 911 NOW. These DANGER SIGNS mean you need help right away. Don’t wait to hear back from your doctor. |
||
(See also “Resources” at the end of this course for a link to the NHLBI “Asthma Action Plan” worksheet.)
(Adapted from CDC, n.d.)
CASE
ASTHMA ACTION PLAN
Sixteen-year-old Nadia, recently diagnosed with asthma, is meeting with the office nurse, who is assessing Nadia’s current status so she can report her findings to Nadia’s physician. The nurse judges Nadia’s asthma severity to be moderate and notes her baseline FEV1 and PEF values. She also notes that Nadia’s asthma appears to be triggered by exercise, dust mites, and fragrances, and that Nadia’s knowledge of the disease appears to be minimal.
The nurse then counsels Nadia on the basics of asthma management, focusing on issues such as carrying an inhaler (particularly during exercise), avoiding asthma triggers, using a peak flow meter, and anticipating and handling an attack. These matters are incorporated into the written asthma action plan, which includes a diary for Nadia to record the following information:
- The daily state or level of Nadia’s asthma (including assessment of her symptoms, lung function, and ability to perform routine activities)
- Nadia’s response to asthma attacks
- Phone numbers and website addresses for Nadia’s physician, the local hospital, and organizations providing asthma-related educational information and counseling
The medication portion of the written plan outlines step therapy for asthma management, starting with short-acting beta agonist inhalers and progressing to corticosteroids (at increasing doses) and other medications as appropriate. These instructions emphasize the need to administer the minimal amount of medication to control Nadia’s symptoms as well as the importance of assessing her asthma severity level at each step of the protocol.
Once Nadia has reviewed and accepted the written plan, she schedules a follow-up appointment in 2 weeks, at which time her degree of asthma control will be assessed and her medications will be adjusted as necessary.
Recognizing Asthma Triggers and Exposure Reduction
Patients will usually know many of the factors that trigger or worsen their asthma symptoms. As the patient and clinician work to identify all the environmental factors that are asthma aggravators, it is helpful to give the patient a list showing the wide range of common triggers and how to avoid them. (See also “Asthma Triggers and Aggravating Factors” earlier in this course.)
EXPOSURE REDUCTION STRATEGIES FOR COMMON ASTHMA TRIGGERS
Dust mites are tiny insects not visible to the naked eye that can be found in every home in dust, mattresses, pillows, carpets, cloth furniture, sheets and blankets, clothes, stuffed toys, and other cloth-covered items. If sensitive:
- Use mattress and pillow covers that prevent dust mites from going through them, along with high-efficiency particulate air (HEPA) filtration vacuum cleaners.
- Launder bedding weekly in hot water.
- Do not use down-filled pillows, quilts, or comforters.
- Consider reducing indoor humidity to below 50% using a dehumidifier or central air conditioning system.
Cockroaches and rodents leave droppings that may trigger asthma. If sensitive:
- Consider professional pest management.
- Keep food and garbage in closed containers to decrease chances for attracting roaches and rodents.
- Use poison baits, powders, gels, pastes (e.g., boric acid), or traps to catch and kill pests.
- If using a spray to kill roaches, stay out of the room until the odor disperses.
Animal dander (the flakes of skin or dried saliva from animals with fur or hair) are an allergen to some people. If sensitive:
- Consider keeping pets outdoors.
- Confine pets to common areas of the home only and keep out of bedrooms.
Indoor mold:
- Explore professional mold removal or cleaning to support complete removal.
- Wear gloves to avoid touching mold with bare hands if removing it by oneself.
- Ventilate the area if using a cleaner with bleach or strong smell.
- Dry damp or wet items within 24–48 hours.
- Do not let damp clothes sit in a basket or hamper.
- Fix water leaks throughout the home.
- Remove carpet from basements, bathrooms, and bedrooms.
- Replace absorbent materials, such as ceiling tiles and carpet, if mold is present.
- Use an inexpensive hygrometer to check humidity levels and keep humidity no higher than 50%.
- Empty, defrost, and clean refrigerators regularly.
- Empty and clean air conditioning drip pans regularly.
- Run the bathroom exhaust fan or open a window when showering.
Pollen and outdoor mold. When pollen or mold spore counts are high:
- Keep windows closed.
- If possible, stay indoors with windows closed from late morning to afternoon, which is when pollen and some mold spore counts are highest.
- When traveling by car, keep windows closed and air conditioning on in the recirculation mode.
- Leave lawn mowing, weed pulling, and other gardening chores to others.
- After going outside, change clothes as soon as possible and put dirty clothes in a covered hamper or container to avoid spreading allergens in the home.
- Wear a pollen mask if doing outside chores.
- Talk with a healthcare provider to see if it is necessary to increase anti-inflammatory medicine before the allergy season starts.
Tobacco smoke:
- Quit smoking (or ask a healthcare provider for assistance).
- Ask and encourage family members to quit smoking.
- Do not allow smoking in the home or the car.
Smoke, strong odors, and sprays:
- If possible, avoid using a wood-burning stove, kerosene heater, or fireplace.
- Vent gas stoves to outside the house.
- Avoid air fresheners.
- Avoid strong odors and sprays, such as perfume, talcum powder, hair spray, and paints.
Vacuum cleaning:
- Enlist someone else to vacuum once or twice a week, if possible. Stay out of rooms while they are being vacuumed and for a short while afterward.
- If one must vacuum, use a HEPA filtration vacuum cleaner.
Foods and medications:
- To avoid sulfites in foods and beverages, do not drink beer or wine or eat dried fruit, processed potatoes, or shrimp if they cause asthma symptoms.
- Inform a healthcare provider about all medicines being taken. Include aspirin, vitamins, and other supplements as well as nonselective beta blockers (including those in eyedrops).
Weather:
- Monitor the weather forecast to be prepared for changes that may trigger asthma symptoms.
- Carry a small scarf to go over the nose and mouth in windy or cold weather.
Physical activity and exercise:
- Use rescue medicines before sports or exercise to prevent symptoms, if included in asthma plan.
Viruses, colds, influenza, bronchitis:
- Wash hands often.
- Avoid touching eyes, nose, or mouth.
- Avoid contact with people who have colds.
- Get a flu shot every year, preferably in the fall, per provider recommendations.
- Get a pneumonia vaccine per provider recommendations.
- Get the COVID-19 vaccine if eligible.
Recreational drugs increase the risk of life-threatening exacerbation and can cause missed doses of prescribed asthma medications.
- Avoid use of recreational drugs, including cannabis, cocaine, crack cocaine, hallucinogens and dissociative drugs, heroin, inhalants, and poppers.
Strong emotions (laughing, crying, feeling stressed or anxious, anger, fear, yelling):
- Avoid stress-inducing situations whenever possible.
- Use relaxation exercises and techniques.
- Take advantage of work breaks and lunch hour.
(NHLBI, 2024b; Mayo Clinic, 2024e; CDC, 2024c; Asthma UK, 2022b)
INTERDISCIPLINARY THERAPIES
Pulmonary Rehabilitation
Pulmonary rehabilitation is a program that involves a team of healthcare providers who work to improve the well-being of people with chronic respiratory disorders. While professional roles may overlap, each individual brings their own expertise to the rehabilitation effort. This team often includes physicians, nurses, respiratory therapists, physical therapists, occupational therapists, dietitians or nutritionists, psychologists, and social workers. Pulmonary rehabilitation is an outpatient program based in a hospital or clinic, and some therapies can also be provided in a patient’s home.
Pulmonary rehabilitation has many benefits, including improved:
- Quality of life
- Management of anxiety and depression
- Muscle strength
- Management of routine activities, work, outings, and social activities
(NHLBI, 2022)
The pulmonary rehabilitation team performs lung function, exercise, and possibly blood tests to help develop an individualized care plan. The patient’s medical history and prescribed treatment plan are reviewed, along with an assessment of mental health and diet. The team works together to create a plan that fits the individual patient’s needs in the areas described below (Celli, 2024).
Exercise training is designed to improve endurance and muscle strength. It may include:
- Endurance training
- Lower-extremity exercise
- Upper-extremity exercise
- Interval exercise training
- Resistance/strength training
- Alternative exercise training
- Breathing retraining
- Ventilatory muscle training
- Tai chi
- Flexibility training
- Transcutaneous electrical nerve stimulation
Nutritional counseling can be included in the pulmonary rehab program, since being either overweight or underweight can affect breathing. An eating plan can be developed to help the patient work toward a healthy weight.
Education about asthma and how to manage symptoms may include:
- How to avoid situations that make symptoms worse
- How to avoid infections
- When and how to take prescribed medications
- Proper use of inhalers
Promotion of healthy behaviors and health preservation may include:
- Smoking cessation
- Regular exercise
- Nutritional counseling and weight management
- Vaccines
A pulmonary rehab program may include teaching the individual energy-saving techniques for performing daily tasks, such as ways to avoid reaching, lifting, or bending.
Stress-relieving techniques may be included since stress can affect energy breathing.
Breathing techniques can be used to increase oxygen levels, decrease how often breaths are taken, and keep airways open longer.
Psychological counseling and/or group support may be part of the pulmonary rehab program, as individuals with chronic lung disease are more prone to depression, anxiety, and other emotional problems. These comorbidities are associated with poor asthma control, greater functional disability, lower quality of life, and more frequent hospitalizations and physician’s visits (Shenoy & Paul, 2023).
Respiratory Therapy
Respiratory therapists (RTs) are key members of the asthma pulmonary rehabilitation team providing treatment to patients from infants to adults. They may work in acute care settings, patients’ homes, outpatient clinics, emergency departments, and the community providing patients with asthma trigger management and asthma education and assisting in the development and implementation of the patient’s asthma action plan. RTs are involved in diagnosis, acute treatment, follow-up, and monitoring.
Respiratory therapists help identify the patient’s asthma triggers and how to manage them, demonstrate respiratory medical devices, explain new respiratory medications, and perform testing such as spirometry (Cleveland Clinic, 2023a).
(See also “Asthma Inpatient Respiratory Therapy” earlier in this course.)
Physical Therapy
Physical therapists are concerned with developing, maintaining, optimizing, and restoring an individual’s physical and functional mobility capabilities. Physical therapy has been shown to improve asthma symptom control, exercise capacity, and sense of well-being. The majority of patients who receive physical therapy treatment are seeking relief from dyspnea and hyperventilation.
Physical therapy works to:
- Maintain or improve exercise tolerance
- Improve functional abilities
- Maintain and improve physical activity, coaching patients toward improving health behavior
- Reduce breathlessness and the work of breathing
- Improve the efficiency of ventilation
- Mobilize and aid the expectoration of secretions
- Improve knowledge and understanding of the disease process
- Reduce thoracic pain
BREATHING RETRAINING TECHNIQUES
Breathing retraining improves symptoms, psychological well-being, and quality of life in adults with asthma. They may also be effective in reducing rescue bronchodilator medication usage. Patients with mild to moderate asthma may benefit the most from breathing retraining techniques. The goal is to normalize breathing patterns by stabilizing respiratory rate and increasing expiratory airflow. Instructions provided by the physical therapist may include:
- Decreasing breaths taken (reducing respiratory rate)
- Taking smaller breaths to reduce tidal volume
- Using diaphragmatic deep breathing with abdominal muscles and lower thoracic chest movement
- Breathing through the nose
- Relaxing and controlling breathing
- Decreasing expiratory flow through pursed-lip breathing.
All of these techniques help control breathing and reduce airflow turbulence, hyperinflation, variable breathing pattern, and anxiety (Physiopedia, 2021).
CHEST WALL MOBILIZATION
Structured chest wall mobilization is a physical therapy technique designed for the maintenance or improvement of mobility of the chest wall, trunk, and shoulder girdles. Chest mobilization exercises can also be used to increase chest wall mobility, flexibility, and thoracic compliance. Chest wall mobilization includes:
- Lateral flexion of the chest wall
- Chest wall extension
- Lateral gliding of thoracic spine
- Pectoralis major muscle stretching
(Tsui et al., 2023)
BUTEYKO TECHNIQUE
This technique is specific for reducing hyperinflation. It is based on the theory that bronchospasm is caused by hyperventilation that leads to a low PaCO2, resulting in asthmatic symptoms. The goal of this technique is to reduce ventilation and subsequently lung volume. The instructions for this technique include:
- Breathe normally through the nose for 2 to 3 minutes.
- Breathe out normally, then close the nose with one’s fingers and hold.
- Remember the number of seconds the breath is held.
- On the first need to breathe, release the nose and return to nasal breathing (control pause).
- Wait 3 minutes.
- Repeat and hold the breath for as long as possible (maximum pause).
Persons with mild asthma can hold the breath for up to 20 seconds, those with moderate asthma for 15 seconds, and those with severe asthma for up to 10 seconds. This is practiced twice a day, with the goal of increasing the control pause to 60 seconds and the maximum pause to 2 minutes. The aim is reduction in minute volume by reducing respiratory rate and increasing carbon dioxide levels (Physiopedia, 2021).
PHYSICAL TRAINING
Physical training increases fitness and cardiorespiratory performance, reduces symptoms, and improves quality of life. The development of asthma symptoms while exercising can reduce patients’ willingness to exert themselves physically. Because of this fear, further deterioration in physical health and quality of life may occur, which can result in anxiety and depression. It has been suggested that behavior change intervention focusing on increasing participation in physical activity may have an impact on asthma and quality of life (Physiopedia, 2021).
RESPIRATORY MUSCLE TRAINING
Hyperinflation increases lung volume, which leads to an alteration in inspiratory muscle mechanics. The muscles become shortened, resulting in a poor length-tension relationship for contraction. There is a decreased capacity for tension generation when breathing results in the use of accessory muscles for inspiration.
This training involves breathing exercises done using an external device that makes breathing more difficult. The device used sets up a load to breathe against. During inspiration, air is released only when enough effort is used to force open the values of the device. The respiratory muscles must then work harder, resulting in increased strength, which leads to easier diaphragmatic breathing and reduced hyperinflation (Physiopedia, 2021).
AIRWAY CLEARANCE TECHNIQUES
Physical therapy may assist in the removal of secretions in the airways using:
- Percussions/vibrations: This involves clapping of the chest with a cupped hand to vibrate the airways. This moves mucus from smaller airways into larger ones, where it can be coughed up. This can also be done using a device designed to vibrate the chest.
- Effective coughing:
- Deep coughing:
- Start by inhaling deeply and holding the breath for 2 to 3 seconds.
- Using stomach muscles, forcefully expel the air while avoiding a hacking cough or just clearing the throat.
- Huff coughing:
- Take a breath that is slightly deeper than normal.
- Using stomach muscles, exhale rapidly three times with the mouth open, making a “ha-ha-ha” sound.
- Follow this by controlled diaphragmatic breathing and a deep cough if mucus is felt to be moving.
- Deep coughing:
- Postural drainage: This technique uses gravity to help drain mucus by placing the body in specific positions to drain the five lobes of the lungs.
(Physiopedia, 2021)
(See also “Asthma Inpatient Respiratory Therapy” earlier in this course.)
EDUCATION
Besides specific exercises and positional instruction, physical therapists provide extensive patient education, including (but not limited to):
- Asthma disease process
- Use of bronchodilator and other medications
- Prevention of chest infection
- Correct standing and sitting posture to allow for appropriate chest expansion and lung function
(Physiopedia, 2021)
Occupational Therapy
Occupational therapists (OTs) work with patients with pulmonary diseases such as asthma to increase their potential for independence. They play a major role in pulmonary rehabilitation, combining exercise training, education, and counseling to teach patients how to live a fuller life with a chronic lung condition.
Occupational therapy may include education about the anatomy and physiology of the lungs, various medications and their purpose, and medication management. Occupational therapists may teach relaxation techniques, energy conservation, stress management techniques, and preventative actions the patient can use to manage asthma.
STRESS MANAGEMENT
Occupational therapy strategies that assist with stress management include panic control, progressive relaxation techniques, and breath support exercises to help the patient with asthma better adapt to daily life and to decrease the effects of stress. OTs offer strategies to decrease shortness of breath and improve quality of life and continued participation in meaningful occupations by introducing adaptive, compensatory, and restorative techniques and interventions.
Occupational therapy assists patients in:
- Identifying their symptoms of stress (physical, emotional, and behavioral)
- Recognizing and understanding causes of stress
- Identifying personal strengths and skills
- Learning ways to change self-defeating beliefs or thoughts to improve quality of life
- Learning new coping skills and ways to relax
- Making lifestyle changes to balance work, recreation, and rest
- Smoking cessation or elimination of other undesirable health behaviors
- Learning different relaxation and meditation techniques
Learning to relax is an essential tool in the arsenal for management of asthma. Occupational therapists teach techniques such as:
- Deep breathing
- Progressive muscle relaxation
- Autogenic therapy, in which the patient is taught to connect mind and body so that the body responds to the mind’s commands
- Guided imagery
- Mindfulness-based meditation
- Cognitive behavioral therapy
- Solution-focused therapy
- Therapeutic use of activity
- Motivational interviewing
ENERGY CONSERVATION
Occupational therapists are knowledgeable in activity analysis, grading activities, ergonomics, and body mechanics. Energy conservation and work simplification techniques reduce unnecessary oxygen expenditure while the patient is involved in activity. The occupational therapist works with the individual to determine which activities are of high importance. These activities are then prioritized and performed first or during a time of day when the patient has increased energy. Two methods used by occupational therapist include “simplification of the activity” and the “Four Ps.”
Simplification includes the following energy-saving techniques:
- Omitting parts of an activity
- Changing the order of activities
- Simplifying the way the activity is performed
- Combining activities
The Four Ps of energy conservation consist of:
- Prioritizing which daily activities should be performed now
- Planning so that energy is conserved for the most important activities
- Pacing activities and taking rests before fatigue or shortness of breath develops
- Positioning the body comfortably
(Meys et al., 2024)
FAMILY SUPPORT
Family support is also provided by occupational therapists, especially for parents of children, and helps children to discover efficient ways to adjust habits and routines to conserve energy and to take part in physical activity. Parents are provided with instruction in coping, positioning, breathing techniques, counseling, and medication management for their children.
Alternative or Complementary Treatments
A number of people with asthma look for alternative or complementary treatments to control or enhance control of asthma symptoms. Such treatments might include herbs, dietary supplements, acupuncture, chiropractic, massage therapy, biofeedback, homeopathy, nutrition, and botanicals. Because there have been limited research studies done on such treatments for asthma, the effectiveness and safety of many are unknown. Such treatments are generally not approved by the FDA or by the medical profession, and they are not prescribed by physicians.
Some treatments include:
- Breathing exercises: The Papworth method and yogic breathing (pranayama) can help prevent hyperventilation. These practices may offer modest benefits, if any, and do not seem to improve the allergic reaction that triggers asthma symptoms, but breathing exercises may help with relaxation.
- Acupuncture: Research suggests that acupuncture plus conventional treatment compared to conventional treatment alone improves symptoms but has not established any impact on lung function.
- Chiropractic manipulation: Some studies have found that spinal manipulation may help reduce the number of asthma attacks and need for medication, particularly in children. However, there is not enough evidence to support its use as an effective asthma treatment.
- Diet, vitamins, and supplements: Studies on the use of omega-3 fatty acids have had inconsistent results. One study found that probiotics may lead to fewer episodes of asthma in children and to an improvement in two markers of immune response related to allergic disease, but there was no significant improvement in asthma control, symptoms, or lung function.
- Massage: Studies suggest that massage may help children with asthma breathe more easily, including a recent study of children ages 4–8 whose lung function improved greatly after receiving gentle, 20-minute bedtime back rubs by a parent.
- Relaxation techniques: Medication, biofeedback, hypnosis, and progressive muscle relaxation have been shown to help lower blood pressure and slow breathing. It is uncertain if they help improve asthma, but they can help reduce stress.
- Herbal supplements marketed for asthma treatment have not been thoroughly tested, and the FDA does not regulate them in the same way as medicines. Issues of concern include lack of quality and dose control, minor-to-severe side effects, and drug interactions. There has been limited quality research on the use of herbal supplements and not enough evidence to recommend them for the treatment of asthma. Use of supplements should be discussed with one’s healthcare provider.
(Mayo Clinic, 2023; NCCIH, 2022)
ASTHMA COMPLICATIONS
Asthma is a serious chronic inflammatory disease that places persons with asthma at risk for multiple complications.
Disrupted Quality of Life
Asthma, to varying degrees, has an impact on physical, psychological, and social well-being. A perceived negative impact is more pronounced among those with severe or poorly controlled asthma. Although asthma places a high burden on children, the relative importance of asthma’s impact increases with age, particularly in older women.
- Poorly controlled asthma can result in psychological problems, including isolation, stress, anxiety, and depression.
- Asthma is responsible for a high number of missed school and/or work days. It can cause early permanent disability and premature death. In fact, asthma can be associated with significant limitations on physical, social, and professional/student aspects of living.
- People with asthma experience a financial burden, including decreased earning capacity triggered by absenteeism. This may be followed by difficulty in being able to afford prescribed and over-the-counter medications.
- Functional limitation is characterized by a decline in ability to complete daily activities and other types of physical activities.
- Medication side effects related to the use of oral corticosteroids may include weight gain, sleep disturbance, and neuropsychiatric symptoms. Relationships and sexual intimacy are also affected by medications used in severe asthma.
- Persistent coughing is a major quality of life issue. Chronic cough and symptoms of depression are closely related, and improvement of cough correlates with improved depression scores. Isolation due to fear of severe coughing in public places and negative effects on relationship with family members and coworkers can also result. The greatest impact has been observed in women 65 years of age and older.
Often these impacts are not addressed during standard asthma consultations. Pharmacologic and nonpharmacologic interventions such as education sessions, written asthma action plans, active symptom monitoring, physical activity, and psychological interventions may promote living well with severe asthma (Song et al., 2021; Hin & Kim, 2020).
Respiratory Complications
Persons with asthma have a high risk for developing other respiratory problems.
At the start of the COVID-19 pandemic, individuals with asthma were thought to be at a greater risk for contracting SARS-CoV-2 and for developing more severe COVID-19 disease. More recently, it is thought that a diagnosis of asthma does not confer a more severe course of COVID-19 requiring hospitalization, as do the comorbidities of older age, obesity, metabolic syndrome, diabetes, cardiovascular disease, and immunosuppression. In those with severe or uncontrolled asthma, however, the risk for being hospitalized and/or dying from COVID-19 seems to be mildly increased based on factors including age, comorbidities, morbidity, and underlying pathology (Assaf et al., 2023).
Individuals with asthma are at increased risk for severe disease and complications from influenza (flu). Influenza can affect the lungs, causing inflammation and narrowing of airways, which can trigger symptoms or an asthma attack. Asthma is the most common medical condition among children hospitalized with the flu and one of the more common medical conditions among hospitalized adults with the flu (CDC, 2024b).
A very serious asthma complication is status asthmaticus (SA), a significant medical emergency that requires immediate and aggressive treatment. This is a severe asthma attack of either slow or sudden onset in which symptoms continue and respiratory function declines despite treatment. SA can range from mild to severe and can lead to prolonged hospitalization or respiratory failure and ultimately death. As many as 6% of people hospitalized for status asthmaticus do not survive (Loengard, 2024).
Patients with asthma are at higher risk for serious illness, complications, and even death related to pneumonia. Asthma may make the lungs more receptive to infection by pneumococcal bacteria, and corticosteroids may increase the risk due to suppression of the immune system (AAFA, 2024g).
Another serious respiratory complication is secondary spontaneous pneumothorax. This can be caused by increased airway pressure or as a result of mechanical ventilation. Superimposed infection can also occur in intubated patients. Patients may require a chest tube and aggressive antibiotic therapy for a superimposed infection (Saaden, 2024).
A rare complication of an acute exacerbation of asthma is pneumomediastinum. It is an uncommon event, and the mean age of affected patients is 11 years. This is a condition in which air enters the central compartment of the thoracic cavity. It is considered a self-limiting condition that usually resolves with successful management of asthma. However, morbidity and mortality are high when it is associated with pneumothorax. During a serious attack, the combination can prove fatal (Carolan, 2022).
Complications Related to Asthma Medication Use
Iatrogenic (drug-related) Cushing’s syndrome can develop with the prolonged use of corticosteroid medications for treatment and control of asthma. Signs and symptoms of this condition include:
- Weight gain, especially in the face, supraclavicular region, upper back, and torso
- Skin changes, including purple stria, easy bruising, and other signs of skin thinning
- Proximal muscle weakness
- Menstrual irregularities and decreased libido in women
- Decreased libido and impotence in men
- Psychological problems, including depression, cognitive dysfunction, and emotional lability
- New or worsening hypertension and diabetes mellitus
- Difficulty with wound healing
- Increased infections
- Osteopenia and osteoporotic fractures
- Steroid acne
- Immunosuppression with slow wound healing and increased infections
- Growth retardation in children
(John, 2024)
Complications related to inhaled corticosteroids include:
- Thrush (candidiasis), oral or esophageal, which can be prevented by using a spacer and rinsing, gargling, and spitting after use
- Dysphonia (hoarse voice), which is common with the use of inhaled corticosteroids and may be due to myopathy and spasm of laryngeal muscle, mucosal irritation, or laryngeal candidiasis; reversible when treatment is withdrawn
- Cough and throat irritation, sometimes accompanied by reflex bronchoconstriction
- Unusual complications, such as perioral dermatitis, tongue hypertrophy, and increased thirst
(Saag et al., 2024)
SPECIAL POPULATIONS AND SITUATIONS
Healthcare must be individualized, but there are some useful general guidelines for working with patients with asthma who belong to certain populations or in specific situations.
Older Adults
It is not uncommon for adults in their 70s or 80s to develop asthma symptoms for the first time. Asthma in older adults is more dangerous, as they are more likely to develop respiratory failure, even during mild attacks. Older patients with mild asthma symptoms can have the same level of breathing difficulty as younger asthma patients experiencing a severe asthma episode. Unlike in younger persons, asthma in the older adult rarely goes into remission. Instead, it is more likely to remain a potentially serious and often disabling disease.
An asthma diagnosis in an older person may be missed because other health problems can mask the disease. Heart disease and emphysema are more common in this age group, and the symptoms of these illnesses can be similar to those of asthma.
Treatment of the older person can be complicated, since many take multiple medications for other problems. Asthma medications can react with these other medications and cause unwanted side effects. Some medications, such as beta blockers, aspirin, some other pain relievers, and anti-inflammatory medicines, can prevent asthma medications from working and may worsen asthma symptoms.
Older patients are more likely than younger ones to have mental confusion or memory problems. This may be the result of normal aging or of an illness such as Alzheimer’s disease. Whatever the cause, such problems can make it hard for certain older patients to follow treatment instructions, especially if the person also takes medication for a variety of other health conditions.
In addition, many asthma medications come in the form of metered dose inhalers, which require a certain degree of manual coordination and dexterity. Older adults are more likely to have difficulty with this type of medication delivery device and thus may not receive the correct dose. Dry powder inhalers or oral medications may be of help in this instance (AAFA, 2024c).
Pregnant Women
Asthma severity during pregnancy is related to asthma severity before pregnancy. Symptoms are more likely to worsen in women with severe asthma. About one third of pregnant women will see their asthma symptoms worsen, another third will stay the same, and the last third will see their asthma symptoms improve (GINA, 2024). Most women with asthma whose symptoms change in any way during pregnancy will return to their prepregnancy condition within 3 months following delivery (Cleveland Clinic, 2023b).
Asthma exacerbations in pregnant asthmatic patients tend to occur during weeks 29–36 of pregnancy. Patients with asthma that is not managed or who have severe asthma have a greater risk for complications than those with mild or moderate asthma, including preeclampsia, premature birth, and a baby who is small for gestational age or low birth weight. Appropriate therapy and good asthma control minimize these complications (Cleveland Clinic, 2023b).
The primary goals of asthma management are unchanged in the setting of pregnancy, and the benefit of active treatment to maintain asthma control and prevent exacerbations outweighs the potential risks of routinely using asthma medications (GINA, 2024).
Careful follow-up of asthma by clinicians is recommended every 4–6 weeks during pregnancy (GINA, 2024). It is important to monitor pulmonary function, since diminished pulmonary function during pregnancy is associated with adverse perinatal outcomes.
Spirometry is minimally affected by pregnancy, but other pulmonary function test measurements do change. Total lung capacity may decrease slightly in the last trimester. Residual volume and functional residual capacity normally decrease during pregnancy due to diaphragm elevation from the enlarging uterus. Minute ventilation increases during pregnancy, presumed to be due to circulation progesterone levels. Normal blood gases reveal a high PaO2 and a lower PaCO2 (Madappa, 2023).
For acute asthma exacerbations that require emergency management or hospitalization, fetal monitoring may be indicated in addition to routine monitoring for asthma. Early consultation with obstetrics service for comanagement is appropriate. Fetal heart rate monitoring is the best choice for determining fetal oxygenation (Little, 2021; Schatz & Weinberger, 2024).
Infants and Children
Children with asthma are treated much like adults, with inhaled corticosteroids the drug of choice for long-term management. Short-term use of high-dose inhaled or systemic corticosteroids does not appear to impact linear growth in children, and minimal changes in growth occur with regular low-dose ICS (Miculinić et al., 2024). All children with asthma, regardless of the drugs they are taking, should have their height and weight measured at each office visit.
Medications to treat asthma symptoms in infants and toddlers are often given in liquid form by using a nebulizer with a face mask or an inhaler with a spacer and face mask. Some toddlers and preschoolers are able to use an inhaler with a spacer and mask attachment.
Most babies, toddlers, and preschoolers are treated for asthma by their pediatrician. However, if asthma symptoms are not under control within 3–6 months, if symptoms are severe and persistent, or if asthma episodes required emergency treatment, it is recommended they be seen by an asthma specialist such as an allergist/immunologist or pulmonologist.
Approximately 50% of children with asthma “outgrow” it once they reach or pass through adolescence, although it may return when they are adults, as their respiratory tract remains sensitive to asthma triggers for life (AAFA, 2024h).
Infants and children are often cared for in childcare centers or family day care. Parents should be offered information on how to evaluate the childcare setting to avoid asthma triggers and discuss special needs with the care providers. The Asthma and Allergy Foundation of America (2024i) provides a checklist that can be used by both parents and childcare providers (see “Resources” at the end of this course).
Respiratory morbidity is frequent in children with asthma who are younger than 2 years, making evaluation of pulmonary function all the more important in these children. Children with asthma should be tested using spirometry at each asthma office visit (Rosen & Colin, 2024).
Surgical Patients
Surgical patients with asthma face a higher risk of complications during the perioperative period and an increased risk of various complications postoperatively. Preoperative identification and optimization of patients with asthma before elective surgery are critical in preventing harm, along with a well-planned anesthetic. When patients present for surgery, it is important to determine whether the patient’s asthma is well controlled or poorly controlled in order to mitigate perioperative complications. Elective surgery is postponed until asthma is well controlled.
Induction of general anesthesia, airway manipulation, and emergence represent the most critical times for perioperative respiratory complications. Ensuring expert personnel are involved is essential. A pediatric anesthesiologist for children has been shown to reduce risk for adverse effects.
In patients with well-controlled asthma, routine mechanical ventilation can be used. However, when airflow obstruction is present, mechanical ventilation becomes more difficult. Allowing ample time for exhalation during mechanical ventilation is critical to avoid dynamic hyperinflation, a feared complication in patients with asthma.
Postoperatively, patients are monitored very closely and returned to their preanesthesia asthma regimen as soon as possible (Kamassai et al., 2022).
Dental Patients
Drugs used to treat asthma, such as beta-2 agonists and inhaled steroids, may promote a higher risk of cavities, dental erosion, periodontal disease, and oral candidiasis. The main mechanism involved is the reduction of salivary flow. Other mechanisms include acid pH in the oral cavity induced by inhaled drugs (particularly dry powder), lifestyle (poor oral hygiene and high consumption of sweet and acidic drinks), GERD, and impairment of local immunity (Pacheco-Quito et al., 2023).
Patient management protocols include minimizing stressors, which are the most common cause of asthma exacerbations in the dental office. The increased risk for an asthma attack (i.e., due to dental anxiety, tooth extraction, allergic reactions) also requires patients to bring their reliever medicines to their appointment. Dental treatment can be postponed in the event of an upper respiratory tract infection or exacerbation of asthma (Viola, 2022).
All dental product manufacturers are required to provide a declaration statement detailing all ingredients and possible allergens in a product. Dental materials that may cause reactions are many, including amalgam, latex, sealant materials, sodium hypochlorite, titanium, nickel-chromium alloy composites, and impression materials (Fletcher et al., 2022).
Children in the School Setting
Children with asthma are dependent on parents, healthcare providers, and school staff. It is important that parents connect with the school nurse and other health services staff to inform them about their child’s asthma. Parents should include a discussion about their child’s asthma management during any parent/teacher meetings or conferences. The law requires parental permission to communicate any student health information to a child’s healthcare provider, and it is important for parents to ask about the school’s requirements for such communication.
A child with asthma should have a recent asthma action plan on file at the school and immediate access to a reliever medication in case of an exacerbation. All 50 states have laws in place allowing students with asthma to carry and self-administer asthma reliever inhalers. However, some children are still being denied access to these medications during the school day. Fourteen states have laws or state administrative guidelines allowing schools to stock reliever medications for students with asthma. Laws vary by state and school district, so it is important for parents to know a school’s policies and requirements.
The American Lung Association encourages schools to create a safe environment for children with asthma and provides a tool kit for implementation that includes the following recommendations:
- Know which students are at risk for an asthma emergency.
- Have an asthma action plan on file for each student diagnosed with asthma.
- Ensure students have access to a reliever medication.
- Ensure good indoor air quality.
- Adopt a tobacco-free policy for both indoor and outdoor environments.
- Offer education to teachers, school staff, parents, and children about asthma.
- Reduce student exposure on high pollution days.
- Provide a full-time registered school nurse all day, every day for each school.
- Assure access to primary care providers of students with asthma.
- Encourage physical education and activity for students whose asthma is well managed.
- Provide options for modified activities.
(ALA, 2023f)
Asthma in the Workplace
It is recommended that patients who are diagnosed with occupational asthma induced by a sensitizing agent be completely and promptly removed from further exposure. Patients with occupational asthma generally have progressive deterioration in lung function if they remain in the same environment.
For workers with mild occupational asthma who have a strong preference for remaining in the workplace, it is recommended that exposure be reduced by engineering controls or respiratory protective devices. However, there is conflicting evidence that this is effective, and “safe” levels of exposure have not been established. For these people, careful ongoing surveillance is advised to detect any further deterioration in lung function.
Workers with severe occupational asthma may be unable to work for several months or longer even after cessation of exposure to the trigger agent. Improvement of occupational asthma after cessation of exposure is most often gradual, reaching a plateau about 2 years following cessation of exposure. Most patients show incomplete resolution of asthma, airway responsiveness, and inflammation even many years following cessation of exposure.
Asthma patients at work should have an action plan, see a healthcare provider regularly, and take medications as directed. They should avoid tobacco smoke, and if they smoke, they should get help to quit (Lemière & Bernstein, 2024).
Traveling with Asthma
People with asthma must take precautions when traveling to avoid triggers that may cause asthma symptoms. For example, when traveling by airplane, bad air quality can be a problem, especially on full-capacity flights. Federal law requires that airlines allow service animals in passenger cabins of planes, which also increases the risk for those whose triggers include pet dander. Those with asthma may request being seated away from animals but should be aware that all flights will have pet dander on some people’s clothing (Allergy & Asthma Network, n.d.; ACAAI, 2024).
When traveling by car, it is important to replace air filters and clean the ventilation and air conditioning system (ALA, 2023d). Windows should be rolled up and air conditioning turned on.
Persons with asthma may request nonsmoking, mold-free, and pet-free rooms in hotels or resorts. They can use the air conditioning in the hotel room and keep the windows closed. If allergic to dust mites, they should bring their own pillow and hypoallergenic cover (ACAAI, 2024).
Patients should be instructed to ensure they have adequate medications for their time away and to carry their medications with them wherever they go (CDC, 2022a). When traveling abroad, they should make certain that devices such as nebulizers are equipped with an electrical current converter.
CONCLUSION
Asthma is a chronic respiratory disease in which patients experience repeated episodes of coughing, wheezing, and difficulty breathing. In a patient with asthma, the airways of the lungs are excessively reactive to irritants (called triggers) and respond by narrowing, swelling, and filling with mucus. This disabling response can usually be reversed by inhaling a short-acting bronchodilator medication.
Asthma is a common problem that often first shows up in childhood, although it can appear at any age. Currently, there is no cure, but the symptoms disappear on their own in a significant number of patients, especially during their teenage years.
A common feature of the disease is the lungs’ sensitivity to stimuli that do not produce similar symptoms in people with normal lungs. The irritants that trigger asthma can include dust, chemical vapors, exercise, sudden changes in air temperature or humidity, allergens, psychological stress, or certain medicines such as aspirin.
Between exacerbations, a person with asthma may have no noticeable breathing difficulties, although measurements of lung function will show an increase in the time that it takes the patient to forcefully empty his or her lungs. However, during an exacerbation (or “attack”), the patient develops a marked airflow obstruction that makes breathing difficult or, in extremely severe cases, leads to death.
Mild and intermittent asthma attacks can usually be treated with as needed low-dose ICS-formoterol. Severe attacks require medical attention; they are treated with bronchodilators, oxygen, and oral corticosteroids.
The best prevention for asthma attacks is a long-term management plan that includes inhaled corticosteroids plus careful avoidance of contact with the patient’s triggers. The specific regimen of controller medications (such as inhaled corticosteroids) must be tailored to the severity of the patient’s underlying disease.
At one time, the focus of asthma treatment was on avoiding or quickly treating attacks. Recently, with the realization that asthma is a chronic inflammatory condition, the goal has also been to manage and lessen the inflammation so that the daily life of an asthma patient can include as wide a variety of activities as possible.
RESOURCES
Asthma (American Lung Association)
Asthma (CDC)
Asthma (WHO)
Asthma action plan (CDC)
Asthma and Allergy Foundation of America
Asthma Quality of Life Questionnaire
Children’s asthma education video series (University of North Carolina)
Global Initiative for Asthma (GINA)
REFERENCES
NOTE: Complete URLs for references retrieved from online sources are provided in the PDF of this course.
Abdo M, Trinkmann F, Kirsten AM, Biller H, Pedersen F, Waschki B, et al. (2021). The relevance of small airway dysfunction in asthma with nocturnal symptoms. Journal of Asthma and Allergy, 14, 897–905.
Abuaish S, Eltayeb H, Bepari A, Alqahtani RS, Alqahtani AH, & Alzahrani WN. (2023). The association of asthma anxiety, depression, and mild cognitive impairment among middle-aged and elderly individuals in Saudi Arabia. Behavioral Sciences, 13(10), 1–14.
Aegerter H & Lambrecht BN. (2023). The pathology of asthma: What is obstructing our view? Annual Review of Pathology: Mechanisms of Disease, 18(1), 387–409.
Allergy & Asthma Network. (n.d.). Airline asthma and allergy policies—Can you fly safely? https://allergyasthmanetwork.org
American Academy of Allergy Asthma & Immunology (AAAAI). (2024). Drug guide. https://www.aaaai.org
American College of Allergy, Asthma, & Immunology (ACAAI). (2024). Allergies and asthma on vacation. https://acaai.org
American Lung Association (ALA). (2024a). Measuring your peak flow rate. https://lung.org
American Lung Association (ALA). (2024b). Create an asthma action plan. https://www.lung.org
American Lung Association (ALA). (2023a). Asthma and indoor air. https://www.lung.org
American Lung Association (ALA). (2023b). Methacholine challenge test. https://www.lung.org
American Lung Association (ALA). (2023c). Reduce asthma triggers. https://www.lung.org
American Lung Association (ALA). (2023d). Air pollution in your car. https://www.lung.org
American Lung Association (ALA). (2023e). Pulse oximetry. https://www.lung.org
American Lung Association (ALA). (2023f). Back to school with asthma toolkit for schools. https://www.lung.org
American Lung Association (ALA). (2022). Current asthma by state. https://www.lung.org
Apter A & Gleeson P. (2024). Enhancing patient adherence to asthma therapy. UpToDate. https://www.uptodate.com
Apter A & Patel P. (2024). Asthma education and self-management. UpToDate. https://www.uptodate.com
Assaf S, Stenberg H, Jesenak M, Tarasevych SP, Hanania NA, & Diamant S. (2023). Asthma in the era of COVID-19. Respiratory Medicine, 218, 1–6.
Asthma and Allergy Foundation of America (AAFA). (2024a). Asthma facts and figures. https://aafa.org
Asthma and Allergy Foundation of America (AAFA). (2024b). Adult-onset asthma. https://asthmaandallergies.org
Asthma and Allergy Foundation of America (AAFA). (2024c). Asthma in older adults. https://asthmaandallergies.org
Asthma and Allergy Foundation of America (AAFA). (2024d). Air pollution and asthma. https://aafa.org
Asthma and Allergy Foundation of America (AAFA). (2024e). Asthma and gastroesophageal reflux disease. https://asthmaandallergies.org
Asthma and Allergy Foundation of America (AAFA). (2024f). AAFA leads the way to lower costs of asthma inhalers. https://community.aafa.org
Asthma and Allergy Foundation of America (AAFA). (2024g). Asthma: Pneumonia. https://aafa.org
Asthma and Allergy Foundation of America (AAFA). (2024h). Asthma in infants and young children. https://asthmaandallergies.org
Asthma and Allergy Foundation of America (AAFA). (2024i). Asthma-friendly child care checklist. http://asthmaandallergies.org
Asthma and Allergy Foundation of America (AAFA). (2023). Asthma capitals 2023. https://aafa.org
Asthma UK. (2022a). Tests for severe asthma. https://www.asthma.org
Asthma UK. (2022b). Recreational drugs. https://www.asthma.org
Asthma UK. (2024a). Symptoms of asthma. https://www.asthma.org
Asthma UK. (2024b). Female sex hormones and asthma. https://www.asthmaandlung.org
Asthma UK. (2024c). Ten common mistakes with inhaler technique. https://www.asthmaandlung.org
Bao Y & Zhu X. (2022). Role of chemokines and inflammatory cells in respiratory allergy. Journal of Asthma and Allergy, 1805–22.
Bédard A, Li Z, Ait-hadad W, Camargo CA Jr, Leynaert B, Pison C, et al. (2021). The role of nutritional factors in asthma: Challenges and opportunities for epidemiological research. International Journal of Environmental Research and Public Health, 18, 3013. https://doi.org/10.3390/ijerph18063013
Britt RD, Ruwanpathirana A, Ford ML, & Lewis BW. (2023). Macrophages orchestrate airway inflammation, remodeling, and resolution in asthma. International Journal of Molecular Sciences, 24(13), 1–26.
Brustad N, Bønnelykke K, & Chawes B. (2023). Dietary prevention strategies for childhood asthma. Pediatric Allergy and Immunology, 34(7), 1–10.
Cahill KN. (2024). Acute exacerbations of asthma in adults: home and office management. UpToDate. https://www.uptodate.com
Carolan P. (2022). Pneumomediastinum. Medscape. https://emedicine.medscape.com
Celli B. (2024). Pulmonary rehabilitation. UpToDate. https://www.uptodate.com
Centers for Disease Control and Prevention (CDC). (2024a). Self-care for asthma—Using your inhaler. https://www.cdc.gov
Centers for Disease Control and Prevention (CDC). (2024b). Living with asthma. https://www.cdc.gov
Centers for Disease Control and Prevention (CDC). (2024c). Controlling asthma: Common asthma triggers. https://www.cdc.gov
Centers for Disease Control and Prevention (CDC). (2023a). Most recent national asthma data. https://www.cdc.gov
Centers for Disease Control and Prevention (CDC). (2023b). Most recent asthma state or territory data. https://www.cdc.gov
Centers for Disease Control and Prevention (CDC). (2023c). Asthma-associated emergency department visits during the Canadian wildfire smoke episodes—United States, April–August 2023. MMWR, 72, 926–32. http://dx.doi.org/10.15585/mmwr.mm7234a5
Centers for Disease Control and Prevention (CDC). (2023d). Respiratory infections and asthma. https://www.cdc.gov
Centers for Disease Control and Prevention (CDC). (2022a). Traveling abroad with medications. https://wwwnc.cdc.gov
Centers for Disease Control and Prevention (CDC). (2022b). Data, statistics, and surveillance. Most recent national asthma data. https://www.cdc.gov
Centers for Disease Control and Prevention (CDC). (2018). Know how to use your asthma inhaler. https://www.cdc.gov
Centers for Disease Control and Prevention (CDC). (n.d.). Asthma action plan. https://www.cdc.gov
Chakraborty R, Chen RJ, & Basnet S. (2024). Status asthmaticus. StatPearls Publishing.
Chatkin J, Correa L, & Santos U. (2022). External environmental pollution factor for asthma. Clinical Reviews in Allergy & Immunology, 62, 72–89.
Choi J & Azmat C. (2023). Leukotriene receptor antagonists. StatPearls Publishing.
Cleveland Clinic. (2024). Prednisone tablets. https://my.clevelandclinic.org
Cleveland Clinic. (2023a). Respiratory therapist. https://my.clevelandclinic.org
Cleveland Clinic. (2023b). Asthma & pregnancy. https://my.clevelandclinic.org
Cleveland Clinic. (2022a). Asthma. https://my.clevelandclinic.org
Cleveland Clinic. (2022b). Body plethysmography (pulmonary function test). https://my.clevelandclinic.org
Cleveland Clinic. (2021). Smoking & asthma. https://my.clevelandclinic.org
Dixon A & Nyenhuis S. (2024). Obesity and asthma. UpToDate. https://www.uptodate.com
Donoghue L, Markovetz M, Morrison C, Chen G, McFadden K, et al. (2023). BPIFB1 loss alters airway mucus properties and diminishes mucociliary clearance. American Journal of Physiology. Lung Cellular and Molecular Physiology, 325(6), L765–75. https://doi.org/10.1152/ajplung.00390.2022
Fishe JN, Okorji O, & Blake K. (2023). EMS prehospital evaluation and treatment of asthma in children. StatPearls Publishing. https://www.ncbi.nlm.nih.gov
Fletcher R, Harrison W, & Crighton A. (2022). Dental material allergies and oral soft tissue reactions. British Dental Journal, 232, 620–5.
Fong WCG, Rafiq I, Harvey M, Stanescu S, Ainsworth B, Varkonyi-Sepp J., et al. (2022). The detrimental clinical associations of anxiety and depression with difficult asthma outcomes. Journal of Personalized Medicine, 12(5), 1–17.
Garry JP. (2024). Exercise-induced asthma clinical presentation. Medscape. https://emedicine.medscape.com
Global Initiative for Asthma (GINA). (2024). Global strategy for asthma management and prevention. https://ginasthma.org
Gottwalt B & Tadi P. (2023). Methylxanthines. StatPearls Publishing.
Grant T, Croce E, & Matsui EC. (2022). Asthma and social determinants of health. Annals of Allergy, Asthma, & Immunology, 128(1), 5–11.
Gürdeniz G, Ernst M, Rago D, et al. (2022). Neonatal metabolome of caesarean section and risk of childhood asthma. European Respiratory Journal, 59, 1–11.
Han M. (2024). Asthma and COPD overlap (ACO). UpToDate. https://www.uptodate.com
Hartert T & Bacharier LB. (2024). An overview of asthma management in children and adults. UpToDate. https://www.uptodate.com
Hess D & Dhand R. (2024). The use of inhaler devices in adults. UpToDate. https://www.uptodate.com
Hin H & Kim C. (2020). Understanding the impact of chronic cough on the quality of life in the general population. Allergy Asthma Immunol Res, 12(6), 906–9.
Huang J & Namazy J. (2023). Asthma in pregnancy. JAMA Insights, 329(22), 1981–2.
Hughes KM, Rice KM, & Suphioglu C. (2022). Importance of allergen-environment interactions in epidemic thunderstorm asthma. Therapeutic Advances in Respiratory Disease, 16, 17534666221099733.
Irvin C. (2024). Bronchoprovocation testing. UpToDate. https://www.uptodate.com
Jackson DJ & Gern JE. (2022). Rhinovirus infections and their roles in asthma: Etiology and exacerbations. Journal of Allergy and Clinical Immunology: In Practice, 10(3), 673–81.
Jamali H, Castillo LT, Morgan CC, Coult J, Muhammad JL, Osobamiro O, et al. (2022). Racial disparity in oxygen saturation measurements by pulse oximetry. Annals of the American Thoracic Society, 19(12), 1951–64.
Jenkins CR, Boulet LP, Lavoie KL, Raherison-Semjen C, & Singh D. (2022). Personalized treatment of asthma: The importance of sex and gender differences. Journal of Allergy and Clinical Immunology, 10(4), 963–71.
Jesenak M, Durdik P, Oppova D, Franova S, Diamant Z, Golebski K, et al. (2023). Dysfunctional mucociliary clearance in asthma and airway remodeling—New insights into an old topic. Respiratory Medicine, 218, 107372. https://doi.org/10.1016/j.rmed.2023.107372
John TA. (2024). Iatrogenic Cushing syndrome. Medscape. https://emedicine.medscape.com
Johns Hopkins Medicine. (2024). Occupational asthma. https://www.hopkinsmedicine.org
Kamassai J, Aina T, & Hauser J. (2022). Asthma anesthesia. StatPearls Publishing.
Kim HB, Lim H, Kim S, Lee SY, Kim HC, Kang MJ, et al. (2023). Particulate matter exposure during pregnancy increases risk of childhood asthma: Modified by gender and NRF2 genotype. Asian Pacific Journal of Allergy and Immunology, 41(3), 220–6.
Kowal K & DuBuske L. (2024). Overview of in vitro allergy tests. UpToDate. https://www.uptodate.com
Laidlaw TM & Boyce JA. (2023). Updates on immune mechanisms in aspirin-exacerbated respiratory disease. Journal of Allergy and Clinical Immunology, 151(2), 301–9.
Lalbiaktluangi C, Yadav MK, Singh PK, Singh A, Iyer M, Vellingiri B, et al. (2023). A cooperativity between virus and bacteria during respiratory infections. Frontiers in Microbiology, 14, 1–17.
Lange-Vaidya N. (2024). Asthma in adolescents and adults: Evaluation and diagnosis. UpToDate. https://www.uptodate.com
Lemière C & Bernstein D. (2024). Occupational asthma, management, prognosis, and prevention. UpToDate. https://www.uptodate.com
Lexicomp. (2021). Prednisone: Drug information. UpToDate. https://www.uptodate.com
Li J. (2024). Trouble breathing: Could it be asthma? Mayo Clinic. https://www.mayoclinic.org
Liang T & Chao J. (2023). Inhaled corticosteroids. StatPearls Publishing. https://www.ncbi.nlm.nih.gov
Litonjua A & Weiss S. (2024a). Epidemiology of asthma. UpToDate. https://www.uptodate.com
Litonjua A & Weiss S. (2024b). Risk factors for asthma. UpToDate. https://www.uptodate.com
Little M. (2021). Asthma in pregnancy. Medscape. https://emedicine.medscape.com
Loengard A. (2024). How status asthmaticus differs from an asthma attack. Verywellhealth. https://www.verywellhealth.com
Madappa T. (2023). Pulmonary disease and pregnancy. Medscape. https://emedicine.medscape.com
Marchant J & Chang A. (2024). Causes of chronic cough in children. UpToDate. https://www.uptodate.com
Martin P. (2024). 8 asthma nursing care plans. Nurseslabs. https://nurseslabs.com
Martin R. (2024). Nocturnal asthma. UpToDate. https://www.uptodate.com
Mayo Clinic. (2024a). Childhood asthma. https://www.mayoclinic.org
Mayo Clinic. (2024b). Spirometry. https://www.mayoclinic.org
Mayo Clinic. (2024c). Cromolyn (inhalation route). https://www.mayoclinic.org
Mayo Clinic. (2024d). Allergy skin tests. http://www.mayoclinic.org
Mayo Clinic. (2024e). Seasonal allergies: Nip them in the bud. https://www.mayoclinic.org
Mayo Clinic. (2024f). Occupational asthma. https://www.mayoclinic.org
Mayo Clinic. (2024g). Prednisone withdrawal: Why taper down slowly. https://www.mayoclinic.org
Mayo Clinic. (2023). Childhood asthma. https://www.mayoclinic.org
Meys R, Franssen FME, Nakken N, Vaes AW, Janssen DJA, Stoffels AAF, et al. (2024). Effects of asthma on the performance of activities of daily living. Occupational Therapy in Health Care, 1–17.
Miculinić A, Mrkić Kobal I, Kušan T, Turkalj M, Plavec D. (2024). Current challenges in pediatric asthma. Children, 11, 632.
Miller RL. (2024). Patient education: Trigger avoidance in asthma. UpToDate. https://www.uptodate.com
Minnesota Department of Health (MN DOH). (2024). Know your asthma triggers. https://www.health.state.mn.us/diseases/asthma/managing/triggers.html
Moore W. (2024). What is eosinophilic asthma. WebMD. https://www.webmd.com
Morris M. (2024a). Asthma. Medscape. https://emedicine.medscape.com
Morris M. (2024b). Asthma workup. Medscape. https://emedicine.medscape.com
Moses S. (2024). Asthma inpatient management. https://fpnotebook.com
Mustafa S & Ramsey A. (2021). Skin test for allergy. MedicineNet. https://www.medicinenet.com
National Asthma Council Australia (NACA). (2023). The Australian asthma handbook. http://www.asthmahandbook.org
National Asthma Education and Prevention Program (NAEPP), Coordinating Committee Expert Panel Working Group. (2020). 2020 focused updates to the asthma management guidelines. U.S. Department of Health and Human Services. https://www.nhlbi.nih.gov
National Asthma Education and Prevention Program (NAEPP), National Heart, Lung, and Blood Institute. (2007). Expert panel report 3: Guidelines for the diagnosis and management of asthma. U.S. Department of Health and Human Services. https://www.nhlbi.nih.gov
National Center for Complementary and Integrative Health (NCCIH). (2022). Asthma and complementary health approaches: What you need to know. https://www.nccih.nih.gov
National Heart, Lung, and Blood Institute (NHLBI). (2024a). Asthma. https://www.nhlbi.nih.gov
National Heart, Lung, and Blood Institute (NHLBI). (2024b). Asthma: Causes and triggers. https://www.nhlbi.nih.gov
National Heart, Lung, and Blood Institute (NHLBI). (2022). Pulmonary rehabilitation. https://www.nhlbi.nih.gov
National Institutes of Health (NIH). (2023). Lung diffusion testing. https://medlineplus.gov
National Institutes of Health (NIH). (2022). Allergy testing—skin. https://medlineplus.gov
Nazario S, González-Sepúlveda L, & Telón-Sosa B. (2022). Inequalities in asthma mortality by ethnicity and race in the United States and Puerto Rico. The Journal of Allergy and Clinical Immunology, 10(8), 2178–80.
Newsom R & Rehman A. (2023). Nocturnal asthma. https://www.sleepfoundation.org
North Shore Community College (NSCC). (2023/2024). Respiratory care program. https://www.northshore.edu
Norwitz E. (2024). Cesarean delivery on maternal request. UpToDate. https://www.uptodate.com
Nunez K. (2021). What you need to know about exercise-induced asthma. Healthline. https://www.healthline.com
O’Byrne PM. (2024). Exercise-induced bronchoconstriction. UpToDate. https://www.uptodate.com
Pacheco-Quito EM, Jaramillo J, Sarmiento-Ordoñez J, & Cuenca-León K. (2023). Drugs prescribed for asthma and their adverse effects on dental health. Dentistry Journal, 11(5), 113.
Physiopedia. (2021). Respiratory physiotherapy. https://www.physio-pedia.com
Pichardo A. (2022). Asthma treatments. WebMD. https://www.webmd.com
Pigakis KM, Stavrou VT, Pantazopoulos I, Daniil Z, Kontopodi AK, & Gourgoulianis K. (2022). Exercise-induced bronchospasm in elite athletes. Cureus, 14(1), e20898.
Puckett Y, Gabbar A, & Bokhari AA. (2023). Prednisone. StatPearls Publishing.
Redding G. (2024). Role of viruses in wheezing and asthma: An overview. UpToDate. https://www.uptodate.com
Reyes-Angel J, Kaviany P, Rastogi D, & Forno E. (2022). Obesity-related asthma in children and adolescents. The Lancet Child & Adolescent Health, 6(10), 713–24.
RNlessons. (n.d.). Impaired gas exchange. https://rnlessons.com
Rodriguez D. (2024). Cigarette and tobacco products in pregnancy: Impact on pregnancy and the neonate. UpToDate. https://www.uptodate.com
Rosen D & Colin A. (2024). Overview of pulmonary function testing in children. UpToDate. https://www.uptodate.com
Saaden M. (2024). What causes pneumothorax in status asthmaticus? Medscape. https://www.medscape.com
Saag K, Furst D, & Barnes P. (2024). Major side effects of inhaled glucocorticoids. UpToDate. http://www.uptodate.com
Sawicki G & Haver K. (2024a). Acute exacerbation in children younger than 2 years: Home/office management and severity assessment. UpToDate. https://www.uptodate.com
Sawicki G & Haver K. (2024b). Patient education: Asthma symptoms and diagnosis in children (beyond the basics). UpToDate. https://www.uptodate.com
Scarfone R. (2024). Acute asthma exacerbations in children: Emergency department management. UpToDate. https://www.uptodate.com
Schatz M & Weinberger S. (2024). Management of asthma during pregnancy. UpToDate. https://www.uptodate.com
Schiffman G. (2022). Asthma medications. eMedicineHealth. https://www.emedicinehealth.com
Schwartzstein R. (2024). Approach to the patient with dyspnea. UpToDate. https://www.uptodate.com
Seladi-Schulman, J. (2023). What to do it you have an asthma attack but don’t have an inhaler. Healthline. https://www.healthline.com
Sharma GD. (2024). Pediatric asthma. Medscape. https://emedicine.medscape.com
Shenoy MA & Paul V. (2023). Pulmonary rehabilitation. StatPearls Publishing.
Simon RA. (2024). Allergic and asthmatic reactions of food additives. UpToDate. https://medilib.ir/uptodate/show/2405
SingHealth. (2024). How to survive an asthma attack if you’re caught without your inhaler. https://www.healthxchange.sg/asthma/complications-management/survive-asthma-without-inhaler
Song WJ, Won HK, Lee SY, Park HK, Cho YS, Chung KF, et al. (2021). Patients’ experiences of asthma exacerbation and management: a qualitative study of severe asthma. ERJ Open, 7, 1–9.
Stavropoulou E, Kantartzi K, Tsigalou C, Konstantinidis T, et al. (2021). Unraveling the interconnection patterns across lung microbiome, respiratory diseases, and COVID-19. Front Cell Microbiol, 10, 619075. https://doi.org/10.3389/fcimb.2020.619075
Sullivan B. (2024). 5 things to know about capnography. https://www.ems1.com
Suri R, Macinko J, Inkelas M, & Needleman J. (2022). The relationship between insurance status and the Affordable Care Act on asthma outcomes among low-income US adults. Chest, 161(6), 1465–74.
Thomson NC, Polosa R, & Sin DD. (2022). Cigarette smoking and asthma. The Journal of Allergy and Clinical Immunology: In Practice, 10(11), 2783–97.
Tsui AYY, Chau RMW, Cheing GLY, Mok TYW, Ling SO, Kwan CHY, et al. (2023). Effect of chest wall mobilization on respiratory muscle function in patients with severe chronic obstructive pulmonary disease (COPD): A randomized controlled trial. Respiratory Medicine, 220, 1–9.
U.S. Environmental Protection Agency (U.S. EPA). (2024). Asthma triggers: Gain control. https://www.epa.gov
U.S. Environmental Protection Agency (U.S. EPA). (2023). The inside story: A guide to indoor air quality. https://www.epa.gov
U.S. Food & Drug Administration (U.S. FDA). (2021). Pulse oximeter accuracy and limitations: FDA safety communication. https://www.fda.gov
U.S. Food & Drug Administration (U.S. FDA). (n.d.). DDT COA #000006: Asthma daily symptoms diary (ADSD). https://www.fda.gov
University of Michigan (UM). (2023). How asthma develops in children. https://www.uofmhealth.org
University of Newcastle. (2022). Questionnaires. https://toolkit.severeasthma.org
Viola T. (2022). Just breathe! Why asthma matters to the dental hygienist. Registered Dental Hygienist. https://www.rdhmag.com
Wang R, Murray CS, Fowler SJ, Simpson A, & Durrington HJ. (2021). Asthma diagnosis: Into the fourth dimension. Thorax, 76, 624–31.
Wayne G. (2024). Airway clearance therapy & coughing nursing care plan. Nurseslabs. https://nurseslabs.com
WebMD. (2024). Allergy tests and asthma. https://www.webmd.com
Weiss S. (2021). Genetics of asthma. Medscape. https://emedicine.medscape.com
World Health Organization (WHO). (2024). Asthma. https://www.who.int/news-room/fact-sheets/detail/asthma/












Customer Rating
4.9 / 855 ratings